Stroke: stages and tactics of intensive care (lecture)
Professor, academician of the Russian Academy of Natural Sciences and MANEB Nazarov I.P.
| Part 1 - Diagnostics | Part 3 – Neuroprotection |
| Part 2 – Stroke Treatment | Part 4 – Hemorrhagic stroke |
Part 2. Treatment of stroke
|
BASIC THERAPY
is aimed at relieving disturbances in vital functions (breathing, hemodynamics, swallowing), as well as status epilepticus. It is carried out immediately, before the type of stroke is determined, or when the nature of the stroke is not specified.
Basic therapy includes the following components:
- Measures aimed at emergency correction of violations of vital functions - normalization of breathing disorders, hemodynamics, swallowing - ABC program (Air - air, Blood - blood, Cor - heart).
- Relief of status epilepticus or series of seizures
- Techniques aimed at combating cerebral edema and preventing increased ICP, regulation of EBV and acid-base balance.
- Correction of autonomic hyperreactions, psychomotor agitation, vomiting, persistent hiccups.
- Measures to care for the patient, normalization of nutrition and prevention of complications.
- Metabolic protection of the brain - correction of brain dysfunction caused by stroke and disorganization of cellular metabolism - neuroprotective therapy, it is most effective in ischemic stroke.
BASIC THERAPY
I. Relief of violations of vital functions:
a) normalization of
respiratory
(restoration of airway patency, sanitation of the oral cavity, introduction of an elastic air duct, tracheal intubation, transfer to mechanical ventilation). Monitoring of respiratory functions and blood oxygen is carried out using a pulse oximeter. Patients with hypoxemia (oxygen saturation <92%) require oxygen inhalation of 2-4 L per minute. As a rule, these are patients with brainstem stroke, with extensive lesions in the middle cerebral artery basin (malignant stroke). Patients with severe lung diseases, with an impaired level of consciousness less than 9 points on the Glasgow Coma Scale, with lost brainstem reflexes and with acute aspiration, tracheal intubation is indicated. These are necessary measures to prevent early complications of stroke, reduce cerebral hypoxia, and prevent cerebral edema.
b) maintaining an optimal level of hemodynamics:
- the choice of antihypertensive drugs
in case of a sharp increase in blood pressure after the development of a stroke should be carried out taking into account 3 factors:
1. Maintaining an optimal level of heart function (SV, IOC). 2. Maintaining bcc. 3. Maintaining the linear velocity of blood flow (LBV) in the vessels of the brain at the proper level.
Regulation of the functions of the cardiovascular system primarily includes blood pressure control. Arterial hypertension occurs in 75% of patients in the acute period of cerebral stroke. In most patients, elevated blood pressure decreases within the first week, but in 30% it remains elevated. It is not recommended to reduce blood pressure in patients with ischemic stroke if systolic < 220 mm Hg and diastolic < 120 mm Hg. The exception is patients with heart failure, acute myocardial infarction, and acute renal failure. In such patients, immediate administration of antihypertensive drugs is indicated. The optimal blood pressure level in patients with a history of arterial hypertension is 180/190-105 mm Hg, without arterial hypertension - 160/90 mm Hg. To lower blood pressure, drugs with a short-term antihypertensive effect and minimal impact on cerebral hemodynamics should be used.
For this purpose,
the following drugs are used
:
- Nifedipine
(synonyms: Corinfar, Adalat, Cordafen, Procardia) is a calcium channel blocker. Prescribed sublingually (5-10 mg; onset of action in 1-5 minutes, duration of action - 2-4 hours) or orally (10-20 mg, onset of action in 30 minutes, duration of 4-7 hours). Blood pressure control - possibly a sharp reduction, especially with sublingual use. - Captopril
(synonyms: capoten, alopresin, lopril, tensiomin) is an ACE inhibitor. Captopril 6.25-12.5 mg per os, sublingually 50 mg (effective after 10 minutes 4 hours). Can be administered intravenously as a bolus: at the rate of 0.5-1.0 mg/kg body weight (onset of action in 3-5 minutes, lasting up to 4 hours). The possibility of a “first dose effect” – a sharp decrease in blood pressure – should be taken into account! - Clonidine
0.15-0.3 mg intramuscularly or intravenously or 0.15-0.075 mg per os.
The drug is a powerful cerebroprotector
and should be used during the acute period, taking into account contraindications - heart rate less than 50 beats/min and low blood pressure. - Pentamine
IV slowly (in 5-7 minutes) no more than 0.5 ml of 5% solution per 10 ml of isotonic sodium chloride solution, under blood pressure control to avoid a rapid decrease in blood pressure. The drug helps prevent and correct cerebral edema. - Labetolol
5-20 mg intravenously, in the absence of bradycardia. - In patients with diastolic pressure > 140 mm Hg. nitroglycerin or
sodium nitroprusside 0.5-1.0 mg/kg/min is indicated In this case, the decrease in blood pressure should not be sharp.
Severe arterial hypotension
Arterial hypotension occurs much less frequently in patients with ischemic stroke. Its causes may be a decrease in circulating blood volume, a decrease in cardiac output due to myocardial infarction, cardiac decompensation or arrhythmias. Therefore, patients with hypotension are advised to restore circulating blood volume by performing infusion therapy (gelatins, hydroxyethyl starches, NaCl 0.9%, polyionic solutions not containing glucose). To increase blood pressure, dopamine and glucocorticoid hormones are prescribed.
- Dopamine
- administered 50 - 100 mg in 250 ml of isotonic sodium chlorine solution (it is preferable to use an infusion pump) 3-6 drops per minute under the control of blood pressure and pulse until blood pressure increases 100-110 mm Hg. Art., the effect of dopamine is short-term. - Glucocorticoid hormones
. Prednisolone is administered as a single intravenous bolus at a dose of 120 mg or dexamethasone 16 mg as a single intravenous bolus. Then the administration mode is determined by blood pressure within the range of 100-110 mm Hg. - In case of severe tachycardia and manifestations of circulatory failure, atrial fibrillation, cardiac glycosides ( strophanthin
0.5-1.0 or 0.025% solution or
corglicon
1.0 ml 0.06% solution) can be prescribed. The drugs are diluted to 20 ml saline. solution and administered IV slowly over 5-6 minutes under the control of blood pressure and pulse.
Relief of status epilepticus or series of seizures
- Seduxen (Relanium)
2-4 ml 0.5% in 20 ml of isotonic NaCl solution slowly intravenously, then, if there is no effect, inject 2-4 ml. - Sodium hydroxybutyrate
at the rate of 70 mg/kg, every 10 ml of the drug is diluted with 10 ml of isotonic sodium chlorine solution. - If there is no effect, non-inhalation anesthesia is used - sodium thiopental or hexenal (it should be remembered that they depress respiration and hemodynamics).
- Sodium thiopental or hexenal
1g is diluted in 10 ml of isotonic sodium chlorine solution (0.9% solution), administered slowly at the rate of 1 ml per 10 kg of patient body weight. - If the status does not stop, perform mechanical ventilation and slowly inject 70-80 ml of 10% sodium thiopental solution.
- If the above measures are ineffective, inhalation anesthesia is performed in the intensive care unit with a mixture of nitrous oxide and oxygen in a ratio of 2:1 or 3:1.
- For a long duration of status epilepticus, in order to prevent cerebral edema, intravenous injection of glucocorticoids is recommended - prednisolone 200-400 mg, dexamethasone 15-20 mg.
Normalization of water and electrolyte balance
A very important area of general therapy for acute stroke is the normalization of water and electrolyte balance. It is necessary to avoid a decrease in circulating blood volume, an increase in hematocrit, and a decrease in the rheological properties of blood. The risk group in this regard consists of elderly patients who have a tendency to dehydration and, at the same time, excessive infusion increases the risk of developing pulmonary edema.
Control of glucose metabolism
It is necessary to regularly monitor your blood glucose levels. It is known that both hyper- and, especially, hypoglycemia have a negative effect on the outcome of ischemic stroke. It is recommended to use insulin in patients with glycemic levels > 10 mmol/l. Monitoring and correction of glycemia is carried out according to the glycemic profile.
Body temperature control
Hyperthermia occurs in 25-60% of patients in the first 48 hours. Hyperthermia negatively affects the outcome of ischemic stroke and increases the size of the infarction. Therefore, when body temperature rises above 37.5°C. the use of antipyretic drugs (500 mg paracetamol) is indicated. However, it must be remembered that in 80% of cases the cause of fever is a bacterial infection. In this regard, it is necessary to search for the source of infection, and if it is identified, use antibiotics as early as possible. The optimal method for assessing the development of infection is the use of a procalcitonin test.
Dysphagia control
All stroke patients should have their swallowing function tested. If there are swallowing disorders (dysphagia), a nasogastric tube is placed to prevent aspiration pneumonia and ensure adequate nutrition for the patient.
Treatment and prevention of cerebral edema
The most severe stroke occurs when cerebral edema develops. Cerebral edema usually develops in the first 24-48 hours from the onset of an ischemic stroke, reaches its peak on the 3rd – 5th day and begins to slowly regress on the 7-8th day. There is a direct relationship between the size of the infarction and the degree of cerebral edema. In some patients with an almost complete infarction in the middle cerebral artery (malignant infarction), cerebral edema and intracranial hypertension can lead to herniation and death. About 80% of patients with malignant infarction of the middle cerebral artery die due to severe cerebral edema, which leads to brain dislocation, compression of vital structures of the brainstem, which is accompanied by increasing depression of consciousness. The more severe the cerebral edema, the more severe the stroke.
To prevent the development of cerebral edema, the patient's head and upper torso must be elevated by 20-30 degrees. It is necessary to normalize body temperature, control blood pressure, relieve pain, strive for normovolemia, and avoid intravenous administration of glucose-containing and hypotonic solutions. The main methods with which the treatment of cerebral edema begins are osmotherapy and hyperventilation. The goal of osmotherapy is to increase plasma osmolarity to 300-320 mOsm/L. Among osmodiuretics, glycerol, mannitol, and Hyperhaes are used.
Dehydration
Dehydration is carried out to combat cerebral edema and increased intracranial pressure
.
Indications for prescribing drugs:
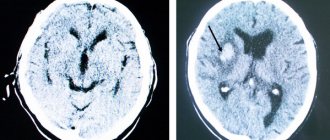
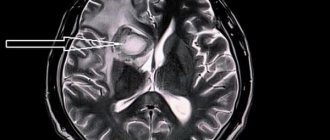
1. signs of cerebral edema identified by CT scan,
2. rapidly increasing neurological symptoms, indicating incipient dislocation and signs of brain herniation.
For dehydration, osmotic diuretics, saluretics, corticosteroid hormones, and mechanical ventilation in the mode of moderate hyperventilation are used. In addition, in the acute stage of a stroke, in the initial phase of the formation of cerebral edema, normalization of breathing, hemodynamics, stimulation of venous outflow from the cranial cavity plays no less a role than the prescription of dehydrating agents.
Osmodiuretics
- Glycerin
is the most preferable, has a longer effect (with intravenous administration - 10 hours), does not cause a significant rebound phenomenon, sudden hypervolemia and a rise in blood pressure. Prescribed IV drip - 10% solution per saline. solution at the rate of 1-2 ml/kg for 2 hours. There is a rapid regression of cerebral symptoms and a decrease in platelet aggregation. Glycerin can be administered into the stomach through a tube at the rate of 1 g/kg 1-2 times a day. A decrease in maximum liquor pressure in ischemic stroke by 72%, and in hemorrhagic stroke by 85–90% has been shown (Misyuk N.S., Kurgaev V.I., 1981). The action of glycerol is shorter than that of mannitol. - Mannitol –
increases the osmotic pressure in the tubules and interferes with the reabsorption of water, which leads to water retention in the tubules and an increase in urine volume. Administer intravenously in a stream or drip in the form of a 10-20% solution at a dose of 0.5-1.5 g/kg body weight, followed by 0.5 g/kg every 3-6 hours. If necessary, the administration of mannitol in this mode can last 3-4 days. Long-term use of mannitol, as well as exceeding the osmolarity level above 320 mOsm/L, can lead to changes in water and electrolyte balance, renal pathology, and can also cause rebound intracerebral hypertension. To prevent rebound syndrome, furosemide can be added at a dose of 1 mg/kg intravenously.
Saluretics
- Furosemide (Lasix) and uregit
increase diuresis by inhibiting the resorption of potassium and chlorine ions in the renal tubules and reduce the production of cerebrospinal fluid. - Their use is advisable only with sufficient central nervous system; they complement the action of osmotic diuretics. They themselves cannot quickly and effectively reduce ICP, but they reduce the production of cerebrospinal fluid.
- Furosemide (Lasix
) is administered intravenously and intramuscularly at a daily dose of 40 – 100 mg (1 amp. – 2 ml of 1% solution contains 20 mg of the drug). - Uregit
is administered intravenously 50 mg in 50 ml of isotonic solution; it is less effective
When prescribing any dehydrating agents, it is necessary to monitor osmolarity ( N = 295-300 mmol/kg) and the concentration of sodium, glucose, urea in the blood serum, diuresis (normally 100 ml per hour or 1500 - 2000 ml per day).
Corticosteroid hormones
(dexamethasone, prednisolone) have a predominantly membrane-stabilizing effect and contribute to the normalization of the BBB.
- Their use has no evidence base
Dexamethasone
administered at a dose of 32 mg per day 2 to 4 times a day, depending on the severity of the stroke, lasting 3-4 days.
Dexamethasone and other corticosteroids have not proven effective as a treatment for cerebral edema in strokes, and their use even increases mortality due to the development of infectious and hemorrhagic complications.
can be used to quickly and effectively reduce intracranial pressure .
It lasts for about 2-3 hours and may be useful as a maintenance measure before surgery. As with osmotherapy, if normal ventilation is resumed too quickly, the effects of increasing intracranial pressure may occur.
If the above methods are ineffective, hypothermia can be used to treat cerebral edema .
Moderate hypothermia (33-36°C) significantly reduces mortality in patients with malignant infarctions of the middle cerebral artery, as evidenced by data from studies. Side effects of hypothermia include thrombocytopenia, bradycardia, and pneumonia.
In case of ineffectiveness of drug treatment, hyperventilation and hypothermia, increasing cerebral edema (usually in patients with malignant middle cerebral artery infarction), it is necessary to consider decompression surgery
. The purpose of the decompression method is to prevent the spread of cerebral edema into the lateral ventricles, diencephalon, midbrain, reduce intracranial pressure, increase perfusion pressure, and preserve cerebral blood flow by preventing compression of collateral vessels.
Surgical treatment of cerebral edema ( hemicraniectomy
) for malignant infarctions of the middle cerebral artery can reduce mortality from 80 to 40%. Early use of this method (within the first day after the onset of stroke), according to data, can further significantly reduce mortality. Decompression of the posterior fossa for cerebellar infarctions is the first choice method and can reduce mortality from 80% with conservative treatment to 30%. Currently, several multicenter studies have been conducted that will allow us to draw a conclusion about the effectiveness of this treatment in selected groups of patients.
Neurological complications, in addition to cerebral edema, include seizures
, which may occur in 4-7% of patients. As a rule, they occur on the first day after the onset of stroke in patients with large infarctions involving the cerebral cortex, as well as in ischemic strokes caused by embolism.
What to do immediately after a stroke at home?
Proper recovery after a stroke at home with the support of relatives and under the supervision of doctors brings good results. It is important to start rehabilitation immediately and not to miss the “rehabilitation window” - this is the year after the stroke, when treatment gives the maximum result.
Recovery after strokes is divided into several periods; the time may shift depending on the patient’s condition.
| The most acute period | Acute period | Early recovery period | Late recovery period | Period of residual effects |
| First 5 days | 3-4 weeks | Up to 6 months | 6-12 months | After 1 year |
Find out how to get comprehensive rehabilitation at home in St. Petersburg with an effectiveness of 95% of the intended result
To know
Differentiated treatment of ischemic stroke
The specific (differentiated) treatment of ischemic stroke is based on reperfusion therapy aimed at restoring the lumen of the vascular bed. Among the methods of treating ischemic stroke, thrombolytic therapy is a method whose effectiveness has been proven by the results of large multicenter studies. The first study, conducted by the National Institute of Nerve Diseases and Stroke in 1995, showed that intravenous rt-PA administered within 3 hours of the onset of ischemic stroke significantly improved outcome. Also in 1995, the results of the European Study of Acute Ischemic Stroke (ECASS-1) were published, which studied the effectiveness of rt-PA prescribed within 6 hours of the onset of stroke at a dose of 1.1 mg/kg. Along with clinical improvement, some patients had a high risk of intracerebral hemorrhage. Three years later, results emerged from the ECASS-2 study, which was performed with rt-PA at a dose of 0.9 mg/kg within a 6-hour “therapeutic window.” Good recovery was observed in 54.3% treated with rt-PA, compared with 46% treated with placebo. Another large study assessed the effectiveness of rt-PA when administered within 3 to 5 hours of the onset of stroke symptoms. The results of this study, like ECASS-2, showed that the incidence of intracerebral hemorrhage was slightly higher when rt-PA was administered within 6 hours than within 3 hours.
A study of the possibility of thrombolysis within 0 to 6 hours using recombinant prourokinase, which was injected locally into the vessel for angiographically confirmed thrombosis of the middle cerebral artery, showed that thrombolytic therapy can be effective up to 6 hours from the onset of stroke, provided that patients are carefully selected. It was proposed to take measures to expand the “therapeutic window” when conducting thrombolysis in patients with acute ischemic stroke. These and other studies have made it possible to develop recommendations for thrombolytic therapy in patients with acute ischemic stroke.
The indication for its implementation is acute ischemic stroke lasting 3 hours from the onset of the disease in patients under 80 years of age. Before starting this treatment, a CT scan of the brain should be performed to rule out hemorrhagic stroke. Thrombolysis is not recommended for patients with severe stroke, large infarcts, blood pressure > 185/110 mmHg, or if the stroke occurred during sleep. Because thrombolytic agents increase the risk of bleeding, the effectiveness and safety of their use should be discussed with the patient and his family before initiating therapy.
Tissue plasminogen activator is currently recognized as the main cerebral thrombolytic. Intravenous administration of plasminogen activator (rt-PA) at a dose of 0.9 mg/kg (10% of the dose administered as a bolus, then slowly over 60 minutes) is indicated in the first 3 hours from the onset of stroke. In selected patients, rt-PA may be administered between 3 and 6 hours. Intravenous administration of streptokinase is not recommended, as there is a high likelihood of bleeding. In patients with acute basilar occlusion and occlusion of the proximal middle cerebral artery, intra-arterial administration is possible in specialized centers.
Indications for intravenous thrombolysis
- The period from the onset of the first symptoms of a stroke is no more than 3 hours
- No history of stroke
- Absence of traumatic brain injury and myocardial infarction for 3 months
- No gastrointestinal bleeding for 3 weeks
- No abdominal surgeries for 2 weeks
- systolic blood pressure is less than 180 mmHg; Diastole blood pressure less than 110 mmHg
- If anticoagulants were previously prescribed, the INR should be below 1.7; the patient did not take warfarin, phenylin
- platelet count greater than/equal to 100,000 mm
- glucose content is greater than/equal to 2.7 mmol/l and not more than 22.5
- Absence on CT of signs of multifocal and extremely extensive infarctions (more than 1/3 of the hemisphere)
- The patient and his relatives should be aware of the potential effect and risk of thrombolysis
Monitoring the patient during thrombolysis
The general condition of the patient is assessed by the doctor during thrombolysis every 15 minutes, every 30 minutes for 6 hours after thrombolysis, then every hour until 24 hours have elapsed from the start of thrombolysis.
If a severe headache, nausea, or vomiting occurs, thrombolysis is stopped and a CT scan is urgently performed. Blood pressure is measured every 15 minutes for the first 2 hours, every 30 minutes for the next 6 hours, and then every hour until 24 hours after the start of thrombolysis.
When systolic blood pressure is greater than/equal to 180 mmHg or diastolic blood pressure is greater than/equal to 105 mmHg. antihypertensive drugs are prescribed (lobetalol 10 mg over 1-3 minutes, if necessary, the same dose is repeated every 10-20 minutes, maximum dose 300 mg).
Despite its proven effectiveness, thrombolytic therapy is used in European countries only in 1-7% of patients with ischemic stroke, which is due to strict criteria for selecting patients for this treatment method.
Restoration of cognitive functions
After a stroke, the patient often experiences speech and memory impairments. It is important to pay special attention to this, since impaired cognitive functions make it difficult to communicate normally and cause strong feelings.
How to get your speech back
After a stroke, many patients experience speech impairment. Disorders manifest in the patient while he is still in the hospital. Most often, recovery is carried out by a speech therapist at the hospital, or you can invite a doctor to your home.
The specialist works with the patient himself and gives recommendations to the family or caregiver on how to help perform the exercises. It is important for loved ones to change their behavior in everyday life so that the person’s speech recovers faster. You need to speak more slowly than usual, use simple words and phrases, accompany them with gestures and, if necessary, drawings. You can give the patient a notebook and pencil, ask him to write a series of numbers, letters, or his own name. Near each piece of furniture in the house it is necessary to put a card with its name, so the patient will remember the words again.
Useful tips to help a person restore speech:
- involve him in the conversation: say hello and goodbye;
- if there is a discussion, make sure that the patient listens and participates at least non-verbally;
- if there is a discussion, make sure that the patient listens and participates at least non-verbally;
- if it is difficult for a person to name some objects, use their names more often in your speech;
- As the patient recovers, correct his speech errors. Increase his vocabulary;
- Monitor the patient's emotions. If the person becomes upset or irritated, change the subject.
How to resist memory changes
After a stroke, it will be more difficult to solve ordinary problems. To return to your normal routine, you need to divide all tasks into small subtasks and take your time. It’s worth planning your day, setting aside more time to complete a task, focusing on only one thing and taking breaks to rest.
Several rules of behavior for the patient that will help him restore his memory and feel better:
- take care of your brain. Do not overload it, and if you feel that you are tired and have begun to think more slowly, rest;
- remove everything unnecessary. If you are busy with important work, choose a quiet place where you will not be distracted;
- concentrate on only one thing;
- get rid of anxiety. Restless thoughts interfere and distract. Often it is sadness, apathy and depression that interfere with memory functioning. It is important to concentrate on interesting activities, develop talents, and be more in nature if your health allows it. Pleasant actions distract from negative thoughts. It is important to change the attitudes: “I no longer need a good memory” or “I am not able to improve my memory” are not suitable.
Exercises to train attention and memory
- describe your yesterday minute by minute, recreate the complete picture of that day. If you forgot something, be distracted by something else or take a rest. After half an hour, return to the exercise and try to remember again;
- Make a mental shopping list, imagine what the products look like: their color, size, packaging. After an hour, try to reproduce this list;
- close your eyes, imagine the number 1. When you see it clearly, erase it and imagine 2 in its place. Do this until 10.
Psychological support
An important point in rehabilitation after a stroke at home is the patient’s motivation. His optimistic attitude and desire to achieve his rehabilitation goal.
After a stroke, care at home should be psychologically comfortable. A person who has had a stroke may have problems controlling their emotions. He may often get angry, cry, scream and laugh. Such a person's mood changes quickly, he may be depressed or confused, experiencing anxiety, fear, frustration, hostility and anger. Psycho-emotional disorders can hinder recovery of health.
At such moments, the patient cannot be left alone for a long time; you need to talk to him, even if it seems that he does not hear or does not understand you. You should definitely involve him in household chores, for example, asking him to help peel potatoes or serve an item, if possible.
Be sure to walk with the patient, leave the house more often, so that he feels part of society. If a person cannot walk yet, invite acquaintances and friends to visit so that he can see other people and communicate with them.
If you follow all these tips, the patient’s recovery will progress, rehabilitation after a stroke at home will have its effect, and the person will definitely achieve the goals that the doctor prescribes for him.
You will see certain signs that the patient is getting better:
- shows interest in the environment, becomes proactive;
- sits down and walks on his own with a walker or without orthopedic devices at all;
- does some things independently: can wash the dishes or prepare a salad;
- expects your arrival at the appointed time or remembers an appointment, for example, on Tuesday at 14:00;
- can find a word in a dictionary or a name in a notebook;
- follows his own meal and medication schedule.