What is the aorta
The aorta is the largest vessel in the human body, which carries blood from the heart to the organs and limbs. The upper section of the aorta runs inside the chest, this section is called the thoracic aorta . The lower part is in the abdominal cavity and is called the abdominal aorta . It delivers blood to the lower part of the body. In the lower abdomen, the abdominal aorta divides into two large vessels - the iliac arteries , which carry blood to the lower extremities.
The aortic wall consists of three layers: internal (intima), middle (media), external (adventitia).
Pathogenesis
The picture of the disease unfolds gradually - day by day, month by month. Blood flow in the abdominal aorta decreases, the elastic frame of its wall is disrupted. It is noteworthy that the anterior wall of the aneurysm contains many collagen and elastin fibers. The side walls, as well as the back wall, are much thinner and more fragile. And since “where it’s thin, it ruptures,” aneurysm ruptures most often occur in the retroperitoneal area. The larger the size of the aneurysm itself, the higher, of course, the risk of rupture.
Abdominal aortic aneurysm
Abdominal aortic aneurysm is a chronic degenerative disease with life-threatening complications. An abdominal aortic aneurysm is defined as an increase in its diameter by more than 50% compared to the norm or a local bulging of its wall. Under the pressure of blood flowing through this vessel, the dilatation or bulging of the aorta may progress. The diameter of a normal aorta in the abdominal region is approximately 2 cm. However, at the site of an aneurysm, the aorta can be dilated to 7 cm or more.
Why is an aortic aneurysm dangerous?
An aortic aneurysm poses a major health risk as it can rupture. A ruptured aneurysm can cause massive internal bleeding, which in turn leads to shock or death.
An abdominal aortic aneurysm can cause other serious health problems. Blood clots (thrombi) often form in the aneurysm sac or parts of the aneurysm tear off, which move with the blood flow along the branches of the aorta to the internal organs and limbs. If one of the blood vessels becomes blocked, it can cause severe pain and lead to organ death or loss of a lower limb. Fortunately, if an aortic aneurysm is diagnosed early, treatment can be timely, safe and effective.
Causes
Most aortic aneurysms appear in the part of the aorta that belongs to the abdominal cavity. Although the exact cause of abdominal aortic aneurysms is unknown, many factors may play a role, including:
- Smoking tobacco.
Cigarette smoking and other forms of tobacco use increase the risk of aortic aneurysms. In addition to the harmful effects that smoking has directly on the arteries, smoking contributes to the accumulation of lipid plaques in the arteries (atherosclerosis) and high blood pressure. Smoking can also cause rapid growth of the aneurysm and subsequent damage to the aorta. - Hardening of the arteries (atherosclerosis).
Atherosclerosis occurs when lipids and other substances deposit on the inner wall of a blood vessel, increasing the risk of an aneurysm. - Infection of the aorta (vasculitis).
In rare cases, an abdominal aortic aneurysm may be caused by an infection or inflammation that weakens part of the aortic wall. - Aneurysms can develop anywhere along the aorta, but when they form in the upper part of the aorta, they are called thoracic aortic aneurysms. Most often, aneurysms form in the lower part of the aorta and are called abdominal aortic aneurysms.
Types of aortic aneurysms
There are “true” and “false” aortic aneurysms. A true aneurysm develops due to the gradual weakening of all layers of the aortic wall. A false aneurysm is usually the result of trauma. It is formed from the connective tissue surrounding the aorta. The cavity of the false aneurysm is filled with blood through a crack in the aortic wall. The aortic walls themselves do not participate in the formation of an aneurysm.
Depending on the form there are:
- saccular aneurysm - expansion of the aortic cavity on only one side;
- spindle-shaped (fusiform) aneurysm - expansion of the aneurysm cavity on all sides;
- mixed aneurysm - a combination of saccular and fusiform forms.
Postoperative period
After surgery, the recovery period takes 3-4 weeks. The patient undergoes regular examinations; cardiologists monitor the functioning of the heart and aorta. Depending on the technique of the intervention performed and the size of the aortic aneurysms, clinical recommendations suggest minimal physical activity only under medical supervision.
Physical therapy with the use of special simulators is indicated so that the heart and blood vessels learn to work in new conditions (with a stent or shunt). After a month, if there are no complications after surgery, the patient can return to the pre-operative lifestyle. It is recommended to reduce physical activity and the amount of fatty foods in the diet so as not to provoke the development of atherosclerosis.
Causes and risk factors for the development of abdominal aortic aneurysm
The causes of the development of abdominal aortic aneurysms are very diverse. The most common cause of aneurysm development is atherosclerosis. Atherosclerotic aneurysms account for 96% of the total number of all aneurysms. In addition, the disease can be either congenital (fibromuscular dysplasia, Erdheim's cystic medianecrosis, Marfan syndrome, etc.) or acquired (inflammatory and non-inflammatory). Inflammation of the aorta occurs when various microorganisms invade (syphilis, tuberculosis, salmonellosis, etc.) or as a result of an allergic-inflammatory process (nonspecific aortoarteritis). Non-inflammatory aneurysms most often develop with atherosclerotic lesions of the aorta. Less commonly, they are the result of injury to its wall.
Risk factors for developing an aneurysm
- Arterial hypertension;
- Smoking;
- The presence of aneurysms in other family members. Which indicates the role of hereditary factors in the development of this disease;
- Gender: men over 60 years of age (abdominal aortic aneurysms occur less frequently in women).
Who is in more danger?
- Age - 50-79 years
- Gender – male (3 times more often)
- Smoking (increases risk 4-5 times)
- Patients with uncontrolled arterial hypertension (high blood pressure);
- Overweight patients;
- Patients with atherosclerotic lesions of blood vessels supplying the brain;
- Patients with impaired blood cholesterol metabolism (dyslipidemia);
- Patients whose relatives also had an aneurysm (the risk is doubled).
Men who smoke in adulthood are at greatest risk (statistically, every 10 have an aneurysm).
Symptoms and signs of abdominal aortic aneurysm
In most patients, abdominal aortic aneurysms occur without any symptoms and are an incidental finding during examinations and operations for other reasons.
When signs of an aneurysm develop, the patient experiences one or more of the following symptoms:
- A feeling of pulsation in the abdomen, similar to a heartbeat, an unpleasant feeling of heaviness or fullness.
- Dull, aching pain in the abdomen, in the navel area, usually on the left.
Indirect signs of abdominal aortic aneurysm are important :
- Abdominal syndrome. Manifested by the appearance of belching, vomiting, unstable stool or constipation, lack of appetite and weight loss;
- Ischioradic syndrome. Manifested by lower back pain, sensory disturbances and movement disorders in the lower extremities;
- Syndrome of chronic ischemia of the lower extremities. Manifests itself in the appearance of pain in the muscles of the lower extremities when walking, sometimes at rest, coldness of the skin of the lower extremities;
- Urological syndrome. It manifests itself as pain and heaviness in the lower back, difficulty urinating, and the appearance of blood in the urine.
Harbingers of rupture may be increased abdominal pain.
When an aneurysm ruptures, the patient suddenly feels an increase or appearance of abdominal pain, sometimes “radiating” to the lower back, groin area and perineum, as well as severe weakness and dizziness. These are symptoms of massive internal bleeding. The development of such a situation is life-threatening! The patient needs emergency medical care!
Two techniques
Aortic rupture can be prevented with surgery. Until 1995, in Russia they were made only in one way: they opened the peritoneum, cut out the deformed section of the aorta, and replaced it with a prosthesis made of durable synthetic material the size of a healthy aorta. The full course of recovery after such an operation takes 2-3 months. The success rate of treatment is 90%. Since 1991, it has become possible to perform operations using the endovascular method, that is, intravascularly. What does it look like? Incisions are made in the femoral arteries, through which surgeons insert the components of the prosthesis, packaged in a delivery device with a diameter of 7-8 mm (and the normal width of the aorta is 2 cm), and pull these parts along a path 30-40 cm long to the desired section of the abdominal aorta. And already there, inside the aorta, the prosthesis is assembled. The endoprosthesis consists of a mesh frame that supports the diameter of the vessel and a thin synthetic material that does not allow blood to pass through. All these manipulations are carried out under fluoroscopy control. Fantastic? Surgeons say: “The technique is simple.” True, endoprostheses are not produced in Russia, and they are not cheap; they are made to individual standards in the West. But there are no quotas for such gentle, non-traumatic, modern operations; the state does not pay for them. Therefore, up to 90% of operations for aortic anervism are still performed in our country using an open surgical method.
Diagnosis of abdominal aortic aneurysms
Most often, abdominal aortic aneurysms are detected by ultrasound examination of the abdominal organs. Typically, the discovery of an aneurysm is an incidental finding. If a doctor suspects a patient has an aortic aneurysm, modern diagnostic methods are used to clarify the diagnosis.
Methods for diagnosing abdominal aortic aneurysm
- Computed tomography in angio mode;
- Magnetic resonance imaging in angio mode;
- X-ray contrast aorto- and angiography;
- Ultrasound duplex or triplex angioscanning of the abdominal aorta.
If necessary, the abdominal and thoracic aorta is examined.
Prognosis and prevention
Unfortunately, abdominal aortic aneurysm is one of the most insidious and unpredictable vascular pathologies, in which the probability of death exceeds 50%. Prevention and timely detection of an aneurysm are essential for a positive outcome. Quitting nicotine addiction, as well as monitoring blood pressure and taking timely measures to normalize it, helps reduce the risk of developing an aneurysm.
Technological progress is helping to reduce the number of diagnostic errors: modern research methods make it possible to identify pathology even in the absence of symptoms. Therefore, people who are at risk - smokers, hypertensive patients, elderly people, as well as those who have a high probability of developing a congenital pathology - should consult a doctor more often for a diagnostic examination. Often, patients are unaware of the development of an aneurysm until it ruptures, but then medical care may not be provided in a timely manner.
Be sure to consult a cardiac surgeon about being examined for the presence of an abdominal aortic aneurysm. Timely detection of the disease can save your life and in any case preserve your health and performance.
Treatment methods for aortic aneurysm
There are several methods for treating aortic aneurysm. It is important to know the advantages and disadvantages of each of these techniques. Approaches to the treatment of abdominal aortic aneurysms:
Monitoring the patient over time
If the aneurysm is less than 4.5 cm in diameter, the patient is recommended to be monitored by a vascular surgeon, since the risk of surgery exceeds the risk of rupture of the aortic aneurysm. Such patients should undergo repeated ultrasound examinations and/or computed tomography at least once every 6 months.
When the aneurysm diameter is more than 5 cm, surgical intervention becomes preferable, since as the size of the aneurysm increases, the risk of aneurysm rupture increases.
If the size of the aneurysm increases by more than 1 cm per year, the risk of rupture increases and surgical treatment also becomes preferable.
Open surgery: aneurysm resection and aortic replacement
Surgical treatment is aimed at preventing life-threatening complications. The risk of surgery is associated with possible complications that include heart attack, stroke, limb loss, acute intestinal ischemia, male sexual dysfunction, embolization, prosthetic infection, and renal failure.
The operation is performed under general anesthesia. The essence of the operation is to remove the aneurysmal expansion and replace it with a synthetic prosthesis. The average mortality rate for open procedures is 3-5%. However, it may be higher if the renal and/or iliac arteries are involved in the aneurysm, as well as due to the patient’s concomitant pathology. Observation in the postoperative period is carried out once a year. Long-term treatment results are good.
Endovascular repair of aortic aneurysm: installation of a stent graft
Endoprosthetics of aortic aneurysm is a modern alternative to open surgery.
The operation is performed under spinal or local anesthesia through small incisions/punctures in the groin areas. Through the above approaches, catheters are inserted into the femoral artery under X-ray control. According to which, in the future, the endoprosthesis will be brought to the aneurysmal extension. An endoprosthesis or stent-graft of the abdominal aorta is a mesh frame made of a special alloy and wrapped in synthetic material. The last stage of the operation is the installation of a stent graft at the site of the aneurysmal expansion of the aorta. Eventually, the aneurysm is “switched off” from the bloodstream and the risk of rupture becomes unlikely. After aortic replacement, the patient is observed in the hospital for 2-4 days and discharged.
This technique allows to reduce the incidence of early complications, shorten the length of patient stay in the hospital and reduce the mortality rate to 1-2%. Observation in the postoperative period is carried out every 4-6 months using ultrasound techniques, CT angiography, X-ray contrast angiography. The endovascular treatment method is certainly less traumatic. About 40,000 such operations are performed annually in the United States alone.
Thus, the choice of treatment method for abdominal aortic aneurysm is based on the individual characteristics of the patient.
Important!
- A myocardial infarction suffered 3 months ago - with stable ECG readings, as well as a stroke - in the absence of a pronounced neurological deficit are not a contraindication to surgery.
- If there is severe coronary insufficiency, then coronary angiography is performed and the state of coronary blood flow is determined to decide on the priority implementation of coronary revascularization.
Abdominal aortic aneurysm surgery
Abdominal aorta replacement
This is a standard open surgical procedure. In our Center, this operation is performed through a mini-access - an incision on the abdominal wall 5-7 cm long (while in the standard version the incision is 15-20 cm long). After processing the surgical field and preparing a vascular prosthesis of the required length for the time required for the operation, the abdominal aorta is clamped above and below the aneurysm. The aneurysm is excised and a prepared vascular graft is sewn in place of the removed area. After checking the tightness of the seams and installing drains, the wound is sutured.
At the Clinic of High Medical Technologies named after. N.I. Pirogov St. Petersburg State University in the treatment of an aneurysm of the abdominal aorta uses vascular prostheses impregnated with silver, which differ from conventional ones in being particularly resistant to infection. The operations last on average 3-4 hours, after which the patient is transferred to the intensive care unit for observation. In the standard course of the early postoperative period, the next morning the patient is transferred to the ward of the specialized department. The total length of hospitalization for such patients is about 7 days.
It should be noted that there are various forms of the disease that complicate the standard course of treatment, which in some cases may require longer hospitalization.
Aortic endoprosthetics
- A more modern method of treating abdominal aortic aneurysm, related to hybrid surgery. This method combines open surgical technologies with endovascular ones; it represents the replacement of an aneurysmally dilated section of the aorta from the inside using a special prosthesis, made in most cases “to order” (this explains its high cost). The vascular prosthesis is specially placed in the delivery system. It is straightened directly into the cavity of the aneurysm, under the control of an X-ray machine. Thus, the prosthesis eliminates the impact of systemic arterial blood flow on the weak, stretched walls of the aorta.
This method allows you to achieve results comparable to the open surgical technique, only with fewer complications, reducing the length of hospitalization and rehabilitation of the patient by 2 times! The use of this modern method is limited only by some anatomical parameters of the aorta itself and the high cost of the endoprosthesis.
Instrumental examination
X-ray examination. For aneurysms of the thoracic aorta, radiography is performed in three projections with mandatory contrasting of the lumen of the esophagus. The expansion of the shadow of the vascular bundle is characteristic. Aneurysms of the descending aorta bulge into the left pulmonary field. Most patients experience displacement of the contrast-enhanced esophagus. Sometimes calcification (calcification) of the aneurysmal sac is determined. In case of aneurysms of the abdominal aorta, plain radiography of the abdominal cavity in two projections allows us to identify calcification of the aortic wall and urination of the lumbar vertebral bodies.
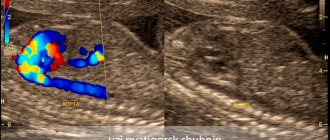
Ultrasound examination (ultrasound) of the aorta and heart. Ultrasound allows us to identify the presence and size in diameter and along the length of aneurysms of the ascending, descending aorta, aortic arch, abdominal aorta, the condition of the vessels extending from the aorta, as well as the presence of aortic valve defect, the nature of changes in the aortic wall.
Computed tomography (CT). When the lumen of the aorta is more than 4 cm, its expansion is considered to be aneurysmal. When performing computed tomography, it is possible to determine the involvement of large arteries in the process and identify signs of dissection (dissection) of the walls (in case of dissecting aortic aneurysm). Angiographic examination (aortography). It is used, as a rule, before surgery when planning its nature and volume.