Almost every doctor encounters arterial hypertension in his daily activities. This fact cannot but be alarming, since this pathology is associated with a high risk of cardiovascular disasters (myocardial infarction, intracerebral hemorrhage), which leads to significant socio-economic and demographic losses. The goal of modern cardiology is to select the optimal means for correcting blood pressure. Sartans for arterial hypertension effectively cope with the task.
Pharmacodynamics of a group of drugs
The increase in blood pressure occurs due to the release of angiotensin 2 (AT 2). When it acts on the receptors, the vascular wall of the arteries contracts, causing a narrowing of the lumen. This leads to an increase in blood pressure. Taking angiotensin receptor blockers (ARBs) interferes with this action.
The effect of the drug occurs due to blocking of receptors, which is why AT 2 does not act.
There are other therapeutic effects aimed at improving the patient's well-being. They are taken into account when prescribing the type of medicine. The data is presented in the table.
| Effect on the body | Action |
| Protection of blood vessels and heart | Reducing the load on the myocardium, which leads to the elimination of ventricular hypertrophy. Reducing the risk of sudden tachycardia, atrial fibrillation |
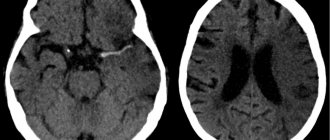
| Brain protection | Improving mental activity and concentration. Eliminate headaches, reduce the risk of stroke |
| Protection of renal tissue, glomerular apparatus | Normalization of diuresis, elimination of edema, microalbuminuria. Reducing cell damage, which inhibits kidney failure. Normalization of mineral metabolism by eliminating the excretion of minerals and protein in the urine |
| Normalization of metabolism | Eliminating the accumulation of cholesterol and other lipoproteins in blood vessels, preventing atherosclerosis. Hypoglycemia, stabilization of diabetes mellitus, increased tissue sensitivity to insulin |
Favorable pharmacodynamic effects are observed in people who use sartans for a long time. A single use of the product only stabilizes the pressure. But this is a temporary effect.
What is the role of activation of the renin-angiotensin-aldosterone system in the development of hypertension?
In the pathogenesis of arterial hypertension, one of the main neurohormonal systems that negatively affects the course of the disease and determines damage to target organs is the renin-angiotensin-aldosterone system. Thus, angiotensin II causes vasoconstriction, stimulation of aldosterone synthesis and its release, sodium reabsorption in the kidneys, cardiac muscle growth, proliferation of smooth muscle cells of blood vessels, increased peripheral noradrenergic activity and a number of other effects.
A turning point in understanding the significance of activation of the renin-angiotensin-aldosterone system in the development of pathology of various organs was the discovery of local tissue RAAS found in the cells of the kidneys, heart, brain, vascular endothelium and other tissues. Experimental and clinical studies have established that hyperactivation of the tissue RAAS occurs in hypertension. At the same time, the secretion of the main substrate of this system - angiotensin II (AT II) - by the tissue of the kidneys, heart, and vascular endothelium increases many times. In particular, it has been established that the local renal concentration of AT II is thousands of times higher than its content in the blood plasma. The mechanisms of the pathogenic action of AT II are due not only to its powerful vasoconstrictor effect, but also to proliferative, prooxidant and prothrombogenic activity. By activating a whole complex of cytokines, AT II promotes the development of fibrosis and sclerosis of the tissue in which it is locally synthesized, be it kidney tissue, heart tissue, retinal vessels or vascular endothelium.
Therefore, today it is absolutely impossible to imagine therapeutic practice without the use of blockers of the renin-angiotensin system. It is these pharmacological drugs that in recent decades have contributed to a significant breakthrough in the treatment of a number of cardiovascular diseases, including such a common human disease as arterial hypertension. It should be remembered that thanks to RAAS blockers, today there is a real opportunity to improve the prognosis and increase the life expectancy of patients by influencing different stages of the cardiovascular continuum. In modern recommendations for the treatment of most cardiovascular diseases, RAAS blockers are considered basic and mandatory pharmacological agents.
A fairly fundamental issue for most practitioners remains the question of the relationship between ACE inhibitors and ARBs (especially when choosing treatment for patients with hypertension), since until recently it was believed that these classes of drugs have the same pharmacological properties. The ARB group was positioned as an alternative to ACEIs and was recommended for use only in cases of dry cough while using ACEIs. The latter had its own specific historical reasons and, of course, contributed to the reticence of doctors regarding the widespread use of ARBs.
Each group of drugs has its pros and cons. The uniqueness of ACE inhibitors is that they provide a double therapeutic effect: they weaken the aggression of AT II (pressor link) and enhance the protective effect of bradykinin (depressor link). But, like any medal that has a downside, it is the bradykinin mechanism of action of ACE inhibitors, which plays an important role in the remodeling of the heart and blood vessels, that underlies the occurrence of cough (5-7% of patients receiving ACE inhibitors for a long time), which sometimes forces them to stop treatment. In addition, experience with the use of ACE inhibitors shows that with long-term (almost constant) use of these drugs, some patients experience the so-called “escape effect,” that is, a weakening of the antihypertensive activity of the drugs.
The discovery of this fact led pharmacological researchers to search for ways to block the action of AT II not by inactivating ACE, but by blocking the receptors to which this peptide binds.
Drug names
Each group of drugs and its representative differ in chemical structure. They have indications for use, contraindications, and side effects. Therefore, before prescribing a medication, a medical history is first collected and instrumental and laboratory examinations are performed. The following groups and related drugs are distinguished.
- Biphenyl tetrazole derivatives. Valsartan, Irbesartan, Losartan, Candesartan.
- Non-biphenyl tetrazole derivatives. Eprosartan or Teveten.
- Biphenyl non-tetrazole compounds. Telmisartan, olmesartan.
Different chemical compounds of drugs are similar in their mechanism of action. That is, the groups have a similar effect on the adrenal hormone. Based on their effect on AT 2, the following drugs are distinguished:
- competitive - block receptors, displacing the hormonal substance from the complex (Eprosartan, Losartan);
- non-competitive - do not displace the hormonal substance, so the effect on the body lasts for a long time (Telmisartan, Valsartan, Candesartan).
In terms of its effect on receptors and vascular tissue, the drug differs from ACE inhibitors. However, the indications for use are identical. Therefore, sartans are often prescribed to patients who have developed resistance to pril (Enalapril).
Division by generation
There are 2 generations, each of which includes a list of medications. Their division is based on the quality of receptor blocking. The data is described in the table.
| Generation | List of drugs | Effect on receptors, additional effects |
| 1 | Losartan, Valsartan, Candesartan, Irbesartan | Block angiotensin 1. Reduce blood pressure, the amount of lipoproteins and cholesterol in blood vessels, protect against kidney and heart tissue |
| 2 | Telmisartan | Suppress all AT receptors and peroxisome activators. Eliminate atherosclerosis, reduce lipoproteins and glucose. Stimulates the pancreas. Relieves the inflammatory reaction |
Groups of 1st and 2nd generations are similar in blood pressure regulation. Their difference is insignificant and cannot be detected using instrumental examinations. If the patient does not have diabetes mellitus or atherosclerosis, a 1st generation drug is preferable.
It is often impossible to find the main name of the drug in a pharmacy. However, there are trade names that correspond in chemical composition and mechanism of action. The following classification of medicines is distinguished:
- Valsartan: Valsacor, Tareg;
- Losartan: Bloktran, Zisacar, Lozap, Larista, Renicard;
- Irbesartan: Aprovel, Firmasta;
- Candesartan: Angiakand, Giposart, Candecor, Ordiss;
- Olmesartan: Cardosal.
If a patient has side effects to one of the prescribed drugs, it is prohibited to independently replace it with another substance. Complications arise. This makes you feel worse and leads to an excessive decrease in blood pressure.
Areas of use
The main indication for use is stable arterial hypertension. The product also regulates other deviations of internal organs. Therefore, it is additionally recommended for patients suffering from the following conditions and diseases:
- heart failure, left ventricular hypertrophy, replacement of the myocardium with connective tissue after a heart attack, atrial fibrillation;
- proteinuria, renal failure, nephritis;
- diabetes mellitus, hyperglycemia;
- metabolic syndrome;
- atherosclerosis.
The advantage of ARBs is the possibility of combined use with other antihypertensive drugs. The combination with Amlodipine showed effectiveness. If you use only 1 type of drug, the success of therapy decreases. When 2 or more drugs are combined, the patient’s well-being is stable, improvements occur in the heart, kidneys, blood vessels, and brain.
The result of therapy does not appear immediately; it is formed with a long course of use of the prescribed drug.
If diabetes mellitus, atherosclerosis and other diseases are observed, but the blood pressure is normal, it is prohibited to prescribe sartans. Systemic hypotension and sudden syncope will occur.
The only drug from the sartan group approved for post-myocardial infarction is Valsartan. It is prescribed 3 days after a heart attack, but in the absence of the risk of a sudden drop in blood pressure.
Pharmacological effects
The renin-angiotensin system is responsible for blood flow and blood pressure. The functions of this system are to regulate vascular tone, the interaction of the liver, kidneys, adrenal glands, and the volume of fluid released. The enzyme angiotensin 2 constricts blood vessels, which increases blood pressure.
The group of sartans protects cells from the action of angiotensin 2. The drugs block the production of the enzyme, thereby protecting the walls of blood vessels. The vessels remain dilated, and the pressure does not rise.
Sartans not only have antihypertensive properties, but are also effectively used to treat renal disorders and abnormalities of the heart.
Sartans are one of the groups of drugs for the treatment of hypertension
The therapeutic effects of sartan drugs are reflected in the table.
| Action | Result |
| Cardioprotective, vasoprotective | the load on the myocardium is reduced; the rate of increase in the mass of the left ventricular myocardium slows down; the risk of developing atrial fibrillation is reduced; normalizes heart function in case of insufficiency |
| Neuroprotective | the risk of cerebrovascular accident is reduced; the risk of cognitive impairment in hypertensive patients decreases |
| Renoprotective | tissue swelling decreases; potassium content increases; the risk of protein appearing in urine is reduced; the degree of development of kidney failure is reduced |
| Metabolic | sensitivity to insulin increases; blood sugar concentration decreases; the risk of developing atherosclerotic lesions is reduced; the likelihood of diabetes in hypertensive patients decreases; the level of triglycerides, cholesterol, and low-density lipoproteins decreases; the level of high-density lipoproteins increases. |
Scheme describing the mechanism of action of sartans
Advantages and side effects
Cardiologists often prescribe sartans because of the immediate effect and beneficial effect on internal organs. The drugs have the following positive aspects:
- a small number of contraindications;
- The recommended dose of tablets is taken once a day and is slowly eliminated from the body;
- side effects develop in a small percentage of patients, they are reversible with dose adjustment;
- Possibility of reception for elderly people;
- no side effects such as cough caused by ACE inhibitors;
- reducing mortality, improving living standards;
- reducing the risk of heart attack and stroke;
- absence of development of malignant neoplasms in lung tissue.
Side effects are rare. There is no negative effect on the entire body. Slight dizziness caused by a decrease in blood pressure is possible. If the condition develops frequently, doctors adjust the dosage of the tablets. Side effects are eliminated.
Advantages of the sartan group
The main benefits of taking angiotensin 2 receptor antagonists:
- almost complete absence of contraindications;
- It is enough to take a long-acting drug once a day to lower blood pressure for a day;
- the likelihood of developing adverse reactions is minimal;
- drugs are prescribed for diabetes, in old age, and for impaired renal function;
- do not cause cough;
- increase the life expectancy of patients with disorders of the heart and blood vessels by several years;
- reduce the likelihood of developing cerebrovascular accidents;
- do not provoke the development of lung cancer.
Contraindications for use
The medicine has been tested on different categories of patients. Its quality has been confirmed by pharmacologists. After the data received, it was revealed that it is prohibited for use by the following groups of people:
- hypersensitivity, intolerance to 1 of the components of the composition;
- pregnancy, breastfeeding.
The active substance penetrates the placental barrier and into breast milk, affecting the fetus and newborn. Possible slowdown in development and dysfunction of internal organs. If an unplanned conception occurs, stop taking the pills.
There is a group of patients to whom the drug can be used, but with caution. The doctor regulates the dosage, so the risk of negative effects is eliminated. Control of the number of tablets is indicated for patients with the following conditions:
- minors under 18 years of age;
- the total volume of circulating blood is below the norm for gender;
- renal failure in the stage of decompensation;
- cirrhosis, malignant degeneration of the liver;
- cholelithiasis, other pathologies leading to blockage of the bile ducts;
- taking medications aimed at preserving potassium in the body.
If at the initial stage of treatment no contraindications were identified, but side effects developed, the drug was immediately discontinued. You will not develop an addiction to it, but complications will arise.
Drug interactions
The ARB group of drugs is prescribed with other drugs, since they rarely enter into chemical interactions without interfering with the therapeutic effect. It is recommended to take it together with other medications aimed at improving the patient’s well-being with cardiovascular pathologies and diabetes.
However, when selecting the dosage, it is taken into account that when combining antihypertensive substances, the pressure will decrease even more. To eliminate the risk of systemic hypotension and syncope, adjust the dose of both drugs used.
There is a group of drugs that can change the condition of the cardiovascular system, liver, and kidneys when combined with sartans. The risk of this action is minimal, but periodic laboratory tests of blood and urine are required. Such means include:
- non-steroidal anti-inflammatory drugs;
- diuretics with no potassium removal effect;
- anticoagulants;
- medicines containing potassium.
These medications may cause side effects. For example, if you take Heparin along with Valsartan, the blood will become excessively thin. The patient may experience sudden bleeding from minor bruises.
How dosages of drugs containing angiotensin receptor antagonists depend on the dose taken?
It has long been proven that blood pressure depends on the dose of the drug taken by the patient. What specific effects depend on the size of the dose of the drug, scientists tried to find out during a study called IRMA 2. Experts found that the decrease in microalbuminuria during the use of irbesartan was pronounced if a person took 300 milligrams per day. The risk of reducing the development of proteinuria was significantly reduced compared with a dose of 150 milligrams per day. At the same time, while taking Aprovel, a dose of 300 milligrams made it possible to significantly reduce the progression of the disease and the occurrence of macroalbuminuria.
The study also showed an important factor: while taking cordarone irbesartan with a dose of 300 milligrams together with the main therapy, the heart of a patient with a persistent form of atrial fibrillation maintained sinus rhythm after cardioversion. The increased dose of the drug was compared with a dose of 150 milligrams taken per day.
Is it possible to develop malignant neoplasms?
Some medications aimed at lowering blood pressure cause the development of malignant tumors. Cancer usually forms in the lung tissue. The first sign of pathology is the presence of a cough. This is a side effect that occurs with ACE inhibitors. Therefore, it is difficult to recognize a complication or cancer in the early stages.
Studies have been conducted to determine the presence or absence of cell malignancy when using sartans. The following recent research findings have been identified:
- absence of the slightest percentage of development of malignant cells;
- reducing the risk of neoplasms of a benign or malignant nature.
Research on cancer is still not closed. Some antihypertensive drugs have this effect. The risks of cancer are minimal. If a patient with arterial hypertension does not take medications, there is a possibility of a heart attack or stroke. When using ARBs, people's lives are prolonged and their quality is improved.
Comparison with ACE inhibitors
ARBs or ACE inhibitors have similar mechanisms of action of active substances on the body. But ACEI affects the conversion of angiotensin 1 to angiotensin 2. This prevents its effect on vascular endothelial receptors. Later it was discovered that it was possible to eliminate not only this reaction, but also the direct effect of the hormonal substance on the cells. This enhances the hypotensive effect and improves a person’s well-being faster.
There are other types of receptors that cause increased blood pressure. Sartans do not affect them. Therefore, these drugs will not completely eliminate the use of ACE inhibitors.
ACE inhibitors remain the drugs of choice at the initial stage of identified hypertension.
In terms of the degree of reduction in blood pressure, both drugs have a similar effect.
Angiotensin receptor blockers are used for patients who have a dry cough. With its long-term formation, an exhausting condition occurs and a headache develops.
If a person does not have a cough, it is better to use an ACE inhibitor.
ARBs are considered best if the patient develops not only hypertension, but also other diseases. For example, diabetes mellitus, atherosclerosis, renal failure. Since these are new drugs, their effect on the body has not been fully studied. This is especially true for patients who have been using pills for many years.
Modern advances in the field of cardiology at the cellular and molecular level have made it possible to critically rethink previously considered fundamental positions in the pathophysiology and treatment of cardiovascular diseases (CVD), in particular arterial hypertension (AH). The polygenic nature of essential hypertension has been finally recognized, which means that it needs to be considered not as a disease of chronically high blood pressure (BP), but as a complex set of interrelated hemodynamic, metabolic and neurohumoral disorders.
According to the unified cardiovascular renal continuum proposed in 1991 by V. Dzau and E. Braunwald, in which the renin-angiotensin-aldosterone system (RAAS) is represented as the leading link in the adaptive regulation of central hemodynamic parameters, hypertension should be considered as one of the main modifiable risk factors in the progression of coronary heart disease (CHD) and chronic heart failure (CHF) [1, 14].
Changes in the views of leading specialists in the field of cardiology on the pathophysiology, diagnosis and treatment of hypertension that have occurred over the past decades of clinical practice are reflected in the European recommendations for the diagnosis and treatment of hypertension (2010–2013), which postulate the main direction of treatment measures - the need to correct endothelial dysfunction , because, according to many leading experts, hypertension is an “endothelial disease” [4, 7, 9, 17].
Endothelial dysfunction is a decrease in the ability of endothelial cells to secrete endothelium-dependent relaxation factor – NO, with a relative or absolute increase in the secretion of vasoconstrictor, aggregation and proliferative factors. One of the important components in the formation of endothelial dysfunction is increased activation of the RAAS. The interrelation of changes in the function and structure of several organs and body systems within the cardiovascular continuum suggests the presence of common pathophysiological processes in the development and progression of organ damage. Basically, the entire variety of mechanisms of adaptation and maladaptation can be reduced to genetic, neurohumoral and hemodynamic factors. Among them, one of the central links belongs to the activation of the RAAS, which can be traced at almost all stages of the cardiovascular continuum [1, 2, 3, 6, 9, 17].
Arterial hypertension occupies a leading place in the structure of CVD and its complications in all countries with developed economies, which defines it as a socio-medical international problem. Consistently high blood pressure level > 140/90 mm Hg. Art. 3–4 times increases the risk of developing cardiovascular complications: cerebral stroke, acute coronary syndrome, myocardial infarction, heart failure with a fatal outcome.
According to an epidemiological study conducted in the Russian Federation among the adult population, 42.5 million people have elevated blood pressure levels: 41.1% of women and 39.2% of men (Fig. 1).
Metabolic syndrome, as defined by WHO experts: “...a non-infectious pandemic of the early 21st century.” Metabolic syndrome is a complex of metabolic disorders and CVD (hypertension, ischemic heart disease, heart failure), the sequence of development of which is pathogenetically interconnected with insulin resistance and manifests itself as disorders of carbohydrate metabolism, atherogenic dyslipidemia, increased triglycerides, low-density lipoproteins, decreased high-density lipoproteins against the background of the visceral-abdominal type obesity [8, 11, 12].
Breaking old stereotypes about the concept of the pathogenesis of chronically high blood pressure (instead of the concept of the priority of hemodynamic unloading - reducing blood pressure) determined the main direction of treatment measures - the need to correct endothelial dysfunction, since, according to leading WHO experts, pathologically high blood pressure levels (> 140 /90 mmHg), as mentioned above, is an “endothelial disease” [1, 3, 4, 9, 17].
Currently, a number of significant additions have been made to the European recommendations for the diagnosis and treatment of hypertension:
The “abdominal” (androgenic) form of obesity has been identified as a marker of “metabolic syndrome”, one of the components of which is hypertension.
Disorders of carbohydrate metabolism have been identified as one of the leading risk factors that increase the incidence of high blood pressure.
C-reactive protein, a high level of which is a significant predictor of cardiovascular complications, has been added to the number of risk markers for endothelial damage (the main link in the pathogenesis of hypertension).
The presence of microalbuminuria is considered as a sign of target organ damage in hypertension (in particular, the kidneys), while proteinuria is considered as a sign of associated kidney pathology.
An increase in creatinine levels in the range of 107–133 mmol/l is considered a sign of target organ damage, while a serum creatinine concentration exceeding 133 mmol/l indicates a multimorbid condition [7].
The renin-angiotensin-aldosterone system plays an important role in the regulation of blood pressure, electrolyte and water balance, and therefore pharmacological blockade of this system at any level can have positive effects in the treatment of hypertension.
In the arsenal of primary care doctors in the Russian Federation there are currently 3 groups of drugs that can block the activity of the RAAS: angiotensin-converting enzyme inhibitors (ACEIs), angiotensin II receptor blockers (BRATII) - sartans, a direct renin inhibitor.
To date, the maximum evidence base has been obtained on the direct hypotensive, pleiotropic effectiveness of angiotensin-converting enzyme inhibitors - ACE inhibitors [1, 3, 6, 10, 15–17].
In terms of the strength of their effect on the endothelium, ACE inhibitors are equal to statins, the effectiveness of which in the prevention and regression of atherosclerotic lesions and endothelial dysfunction has been proven in numerous studies. The multidisciplinary action of ACEIs has made it possible to call them the “golden” standard in the treatment of CVD [1, 3, 15].
The history of the study of the RAAS dates back to 1898, when at Stockholm Karolinska University, the Finnish physiologist Robert Tigelstedt and his student Per Gunnan Bergman isolated the first component of the RAAS, renin, from kidney tissue. More than 50 years later, in 1940, two groups of researchers independently identified a substance that was formed under the influence of activated renin. A group of researchers at the Argentine University of Buenos Airos, led by Professor E. Braun-Menendez, isolated a biologically active hypertensive substance, which they called “hypertensin.” In the same year, a group of scientists led by an outstanding specialist in the field of renal physiology and pathophysiology of arterial hypertension I.
Page identified a substrate called angiotonin, which, under the influence of renin, had a powerful hypertensive effect. In 1958, the terms “hypertensin” and “angiotonin” were united by mutual agreement under the single name “angiotensin” [2, 8, 10].
In 1960, the Brazilian researcher S. Ferreira identified angiotensin-converting enzyme (ACE), initially called “bradykinin-potentiating factor.” Subsequently, several scientific and biological laboratories showed that the enzyme that stabilizes bradykinin is identical to ACE.
The first attempt at pharmacological control of the activity of the RAAS was experimental studies on the competitive ability of the angiotensin II (ATII) receptors of the amino acid compound 1-Asp-S-Ala-ATII (Salarasin), carried out in 1971 by D. Pals and co-workers. The clinical use of Salarazine was delayed for more than 20 years due to the short duration of the hypotensive effect and the need for intravenous administration. And already in 1971, the first ACE inhibitor was synthesized in the laboratory - teprotide, isolated directly from the venom of the Bothrops Jararaca snake. Despite its stable hypotensive effect, its toxic effects have become an obstacle to use in clinical practice. In 1975, the first oral ACE inhibitor SQ14.225, Captopril, was created in the same laboratory, and two other ACE inhibitors, Enalapril and Lisinopril, were soon synthesized.
But only today, after more than 50 years, the important role of the RAAS and ACE inhibitors becomes clear not only in the homeokinetic regulation of blood pressure, tissue perfusion, fluid and electrolyte balance, but also in a wide range of prevention of pathological processes of the cardiovascular continuum.
The renin-angiotensin-aldosterone system is a unique regulatory system, the active effector of which is ATII, produced in the intercellular space by sequential proteolytic cleavage of its precursors. The precursor of ATII is angiotensinogen (ATG) - a biologically inert globulin containing 14 amino acid components, synthesized mainly in the liver, which, under the influence of renin, by cleavage of 4 terminal amino acid components is converted into angiotensin I (ATI).
In turn, ATI is biologically active (vasoconstrictor); under the influence of ACE, exopeptidase, localized on the membranes of various cells (endothelial cells, epithelial cells of the proximal renal tubules, neuroepithelial cells), is converted into active ATII by cleavage of two more amino acid components (Fig. 2).
The main effector of the RAAS is ATII, the action of which is realized through specific angiotensin II receptors (RATII). To date, 4 subtypes of PATII1–4 have been identified. The most important are PATII1, 2, through the stimulation of which the majority of both physiological and pathophysiological effects of ATII are realized.
PATII1 is localized in blood vessels, heart, kidneys, adrenal glands, liver, brain and lungs. PATII2 is widely present in the brain, kidneys and other tissues and plays a counter-regulatory role in relation to ATII1 (see table). The functions of PATI3 are poorly understood, and their stimulation appears to be involved in the spectrum of lipid metabolism in adipocytes, while stimulation of PAII4 modulates the synthesis of plasminogen activator inhibitor. Recently, specific prorenin receptors have also been identified, and their role is being clarified. The experiment shows their effect on the development of diabetic nephropathy. As the identification of ATII receptors and their share in the functioning of the RAAS improves, from the standpoint of clinical pharmacology, new ATII receptor blockers (BRATII) have been created - sartans, which currently include non-peptide compounds with a highly selective blocking effect of AT1 receptors: valsartan, irbesartan, candesartan , losartan, telmisartan, eprosartan.
Currently, according to their pharmacodynamic characteristics, BRATII are divided into two generations: the first affects only the RAAS through the blockade of AT1 receptors, the second generation BRATII are bifunctional drugs that not only block AT1 receptors, but also activate PPAR-γ (nuclear receptors , activated by peroxisomal proliferators-γ), involved in the regulation of intracellular carbohydrate and lipid metabolism.
In total, the mechanisms of action of BRATII are due to the influence on the main neurohumoral links in the regulation of vascular tone of the RAAS and the sympathetic nervous system. Drugs of this group not only block the biological effects of ATII, realized through the AT1 receptors of blood vessels and adrenal glands, but also interact with presynaptic receptors of adrenergic neurons. At the same time, the antihypertensive effect of selective BRATII is based on their affinity ability to selectively block presynaptic PATII1, which controls the rate of synthesis and secretion of norepinephrine into the synaptic cleft. By reducing the synthesis and secretion of norepinephrine into the “synaptic cleft,” BRATII realize their hypotensive effect through a decrease in the tone of the sympathetic nervous system (Fig. 3).
Without affecting the activity of ACE, BRATII does not affect the metabolism of bradykinin, it helps to increase the release of NO and the duration of its biological life, which ultimately results in more effective vasodilation.
Numerous multicenter studies have identified additional mechanisms of the hypotensive effect through the effect of BRATII on hemorheology and microcirculation, which is mediated through the biological structures of homeokinesis:
A. BRATII do not block the tissue activity of the kallikrein-kinin system, which is one of the components of the internal cascade of conversion of plasminogen to plasmin. In turn, plasmin helps remove excess fibrinogen from the vascular bed.
B. BRATII reduce the activity of the platelet-vascular component of hemostasis. Human platelets have receptors for ATII. The antiplatelet activity of BRATII is associated, on the one hand, with the blockade of platelet receptors, on the other, with their beneficial effect on the vascular endothelium (antiplatelet effects) and a decrease in the intracellular calcium concentration in platelets.
B. Selective BRATII inhibit the growth, migration and proliferation of vascular smooth muscle cells, the transformation of monocytes into foam cells, and cause regression of structural changes in arterioles.
G. BRATII improve the blood lipid profile by reducing the concentration of atherogenic lipids and increasing high-density lipoprotein cholesterol; reduce glucose tolerance through an increase in the sensitivity of cellular receptors to insulin, which overall leads to a decrease in blood viscosity [2, 6, 8, 10, 15].
Literature data indicate a violation of the functional activity of platelets already at the early stage of hypertension, which is manifested by an increase in their aggregation activity and increased sensitivity to aggregation inducers [4, 12, 13].
The reasons for the increase in platelet aggregation activity in hypertension may be activation of the sympathetic-adrenal system (due to hypercatecholaminemia), the RAAS with an increase in plasma renin concentration, which provokes the formation of intravascular erythrocyte-platelet aggregates and the release of adenosine diphosphate. Dyslipidemia makes a significant contribution to functional platelet hyperactivity. An increase in the content of total cholesterol, low-density lipoprotein cholesterol and very low-density lipoprotein cholesterol causes hypersecretion of thromboxane A2 with an increase in platelet aggregation activity. This is due to the presence of apo-B and apo-E lipoprotein receptors on the surface of platelets. Platelet activation may also be associated with endothelial dysfunction, the occurrence of an imbalance between the production of activating and blocking mechanisms, and subsequently with remodeling of the vascular wall.
In turn, the deformability of erythrocytes decreases due to the absorption of plasma proteins, primarily fibrinogen, on the surface of erythrocyte membranes. Disturbances in the deformability of erythrocytes occur with changes in the lipid spectrum of the blood, primarily with a violation of the cholesterol/phospholipid ratio, and in the presence of lipid peroxidation products. A change in the elastic properties of erythrocyte membranes is accompanied by a decrease in their surface charge with the subsequent formation of erythrocyte aggregates. In total, this increases the viscous resistance to blood flow at the level of arterioles and is an additional factor in increasing blood pressure [13].
Thus, the antihypertensive effect of BRATII is based on their total effect directly on the cardiovascular system and indirectly on improving the rheological parameters of the blood (viscosity, aggregation activity of platelets and erythrocytes).
The results of numerous clinical studies, in which the pleiotropic effects of sartans were identified, made it possible to formulate a number of new indications for the use of this group of drugs in clinical practice - metabolic syndrome, diabetic nephropathy with microalbuminuria or proteinuria, CHF, atrial fibrillation, diseases of the cardiovascular system with hypertrophy of the left ventricle, intolerance to ACE inhibitors (dry cough, neurotic edema).
Currently, in the pharmaceutical system of the Russian Federation, telmisartan (Mikardis®) is considered one of the first representatives of the second generation sartans with bifunctional pharmacological properties approved for the treatment of CVD. Telmisartan was obtained from the active metabolite of losartan (EXP 3174) by replacing the benzimidazole with the lipophilic imidazole component, which determined the more pronounced lipophilicity and tissue bioavailability of this drug among all BRATII. Due to the presence of a lipophilic group, telmisartan at a dosage of 80 mg once a day is rapidly absorbed in the gastrointestinal tract (bioavailability up to 50%) reaching peak plasma concentrations after 0.5–1.0 hours with a half-life of more than 20 hours. A stable therapeutic concentration of telmisartan in the blood plasma occurs after 5–7 days of taking the drug with a stable hypotensive effect [8].
The clinical effectiveness of telmisartan in various comorbid conditions of the cardiovascular system has been documented in numerous multicenter studies - TRANSCEND, PROTECTION, PRISMA I, PRISMA II, SMOOTH, ATHOS, PROBE, which assessed the presence of hypotensive, antidiabetic, nephroprotective, antiplatelet properties of telmisartan [2 , 5, 6, 8, 10, 11, 16]. The results of these studies convincingly showed that telmisartan has pleiotropic pharmacodynamic effects with organ protection, improving the quality and prognosis of life among patients with various CVDs.
The modern strategy for correcting high blood pressure levels implies, first of all, reducing the risk of cardiovascular complications, deaths, and improving the condition of target organs against the backdrop of effective blood pressure control. This goal is consistent with the further development of bifunctional drugs - BRATII (sartans), which have two or more biopharmacological mechanisms of action and have a protective effect on target organs, which will increase efficiency in the treatment of patients with CVD.
Thus, ATII receptor blockers (ATII1) are a large group of drugs with pleiotropic pharmacological properties, possessing multicomponent antihypertensive efficacy and good tolerability. In recent years, convincing evidence has been obtained that BRATII can improve the long-term prognosis for patients with hypertension, especially when combined with disorders of carbohydrate and lipid metabolism, and the presence of signs of diabetic nephropathy, which are components of the metabolic syndrome. The use of sartans - selective BRATII (telmisartan) in the clinical practice of a primary care physician is promising in the treatment of CVD, especially in the early stages of the cardiovascular continuum and metabolic syndrome.
Effect of ARBs on patients at risk of myocardial infarction
The only drug from the ARB group whose effectiveness has been proven in myocardial infarction is Valsartan. It is prescribed from day 3 after a heart attack, but in the absence of a risk of hypotension. If there is one, the time is extended to 10 days.
Researchers believe that other drugs can cause circulatory problems in the myocardium. This will cause a sudden drug-induced heart attack. However, this theory remains unproven.
Due to the availability of such data, studies were conducted. The results were contradictory. Some patients develop a heart attack, others do not. Therefore, it is believed that the risk of heart attack is present, but it is negligibly small. More often it develops in patients who neglect the rules of a healthy lifestyle:
- smoking;
- frequent drinking of alcoholic beverages, alcoholism;
- taking chemicals, drugs;
- eating fatty, fried, spicy, smoked, salty foods.
Scientists who consider sartans to be the drugs of choice for hypertension explain that a heart attack is not caused by the medicine, but by an incorrect lifestyle. For example, in case of violation of the ban on bed rest, physical overload. Other researchers make reasonable arguments that the incidence of heart attacks increases with ARB use. Therefore, the question is considered open and unproven.
The essence of treatment with ARBs
Angiotensin receptor blockers are medications that significantly improve the quality of life of a patient with arterial hypertension. Blood pressure decreases, and a normal state of systemic blood flow is formed. The drug can be used not only as a monotherapy, but also in combination with other drugs. The possibility of side effects and negative drug interactions is extremely low.
The advantage of the product is in a small dosage used per day. 1 tablet in the prescribed dose is enough to have an effect. This is due to prolonged metabolism in the liver and excretion by the kidneys. If hypertension occurs due to diabetes mellitus or atherosclerosis, the disease will be controlled, so repeated surges in blood pressure will not occur.
Possible adverse reactions
Sartans are considered to be the safest blood pressure medications. The likelihood of developing side effects of sartans is so small that it is not included in a separate list. In rare cases, blood pressure sartans without side effects can cause dizziness due to a decrease in blood counts. Doctors advise taking pills at night to avoid any discomfort.
A side effect of taking sartans may be dizziness.