Anatomical data about the heart as an organ
For more than 30 years, there has been a so-called heart-lung machine, which for a short time can replace the pumping function of the heart, although, of course, it cannot be completely replaced. And this fact makes us worry about the motor of the body, because we cannot live without it.
Mammals of the primate order, which includes humans, are characterized by a 4-chambered heart, i.e. it consists of 4 chambers - 2 ventricles (left and right), and 2 atria (also left and right). The right parts of the heart are responsible for pumping blood through the so-called “lesser” circulation, i.e. heart - lungs (in which the blood is enriched with oxygen); and from the left sections the blood enters the “large circle”, i.e. left atrium - left ventricle - body.
The right atrium communicates with the right ventricle through the tricuspid (three-leaf) valve, and the left atrium communicates with the left ventricle through the mitral (bicuspid) valve, the damage of which will be discussed in this article.
Mitral valve prolapse - symptoms and treatment
Diagnosis criteria
Mitral valve prolapse is most often diagnosed using non-invasive examination methods - the doctor takes into account the patient’s complaints and heredity. But the final diagnosis is made using transthoracic echocardiography.
Instrumental diagnostic methods
During auscultation (listening to the heart) with a stethoscope, the doctor may hear a characteristic systolic click and/or late systolic murmur over the apex of the heart. With the patient standing, the systolic click and murmur appear at the beginning of systole (contraction). With the patient lying or squatting, these sound phenomena are reduced.
The electrocardiogram can detect nonspecific changes in the ST segment and T wave in leads III and aVF. In the presence of mitral valve prolapse, the ECG can diagnose the phenomenon of pre-excitation (“short PQ syndrome”), supraventricular (atrial) tachycardia, and ventricular extrasystole.
chest x-ray Cardiac enlargement may be diagnosed in some patients with a very small anteroposterior chest size.
Transthoracic echocardiography ( Echo-CG) . It is carried out using an ultrasound sensor placed by a doctor on certain points of the chest. It is the most important routine examination in the diagnosis of mitral valve prolapse. Distinctive and important echocardiographic signs of this pathology include deflection of the posterior or both leaflets of the mitral valve into the cavity of the left atrium in mid-systole, in late systole or throughout systole. Deflection (sagging) of the mitral valve in mid-systole is more common, which corresponds to the data obtained by auscultation and angiography.
There are other echocardiographic signs, they are nonspecific, but highly sensitive:
- dilatation (expansion) of the mitral ring;
- increased range of motion of the mitral valve, diastolic contact of the leaflets with the interventricular septum;
- an increase in the range of diastolic divergence of the leaflets and the speed of opening of the anterior valve leaflet;
- systolic displacement of the anterior and posterior leaflets of the mitral valve (more than 3 mm) into the left atrium below the closure of the mitral line;
- thickening of the mitral valve leaflets;
- signs of disruption of the internal structure of the valve tissue (myxomatous valve degeneration);
- reverse blood flow;
- signs of increased pressure in the pulmonary artery.
Transthoracic echocardiography is recommended every 6 to 12 months in all asymptomatic patients with moderate to severe mitral regurgitation. This is necessary to assess the ejection fraction (pumping function of the heart, normally it should be at least 55%) and end-systolic size.
Transesophageal echocardiography. This is an ultrasound test in which a probe is inserted into the esophagus. Indicated only in the absence of contraindications in the following cases:
- Echo-CG does not assess the severity and mechanism of mitral regurgitation and/or the state of left ventricular function;
- The patient is about to undergo valve surgery; during the examination, the question of the nature of the surgical intervention is decided.
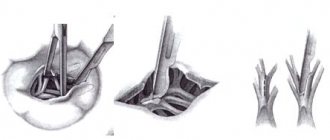
A type of prolapse is the so-called valve . It is usually detected by rupture of the chordae or avulsion of the papillary muscle (more common in acute myocardial infarction). With echocardiography in B-mode, the freely moving papillary muscle and the “dangling” mitral valve leaflet are clearly visible. The valve makes irregular, voluntary movements during diastole (the period of relaxation of the heart muscle) and “falls” into the cavity of the left atrium during ventricular systole. In M-mode, characteristic echocardiographic signs of such a valve are the presence of:
- additional echo signals from the mitral valve leaflet in the cavity of the left atrium during the period of ventricular contraction;
- diastolic vibration of the anterior valve leaflet or paradoxical movement of the posterior mitral leaflet in systole and diastole.
Radionuclide equilibrium ventriculography is performed to assess ejection fraction and assess the severity of heart failure. The method is based on the intravenous administration of a radionuclide with its fixation on red blood cells and subsequent quantitative assessment of the contractility of the heart.
Differential diagnosis
The strategy and tactics of patient management depend on the origin of the prolapse - congenital or acquired, therefore differential diagnosis is carried out only between these types of mitral valve prolapse.
Causes of the disease
Myxomatous mitral valve degeneration
The exact cause of myxomatous mitral valve degeneration is not known; this pathology is often associated with a hereditary predisposition. Most often, this disease affects people who have impaired formation of cartilage tissue, congenital defects and joint diseases.
In recent years, scientists have associated degeneration of the mitral valve (mitral valve myxomatosis) with hormonal disorders of various origins. There is also a certain connection between this pathology and various viral diseases that have a damaging effect on the valves of the heart, as well as streptococcal infection, which causes direct damage not only to the valve apparatus, but also to the endocardium of the heart.
Surgical treatment of mitral valve insufficiency
CLASS I
- 1. Patients with acute severe mitral regurgitation (Level of Evidence: B)
- 2. Patients with chronic severe mitral valve insufficiency and NYHA class II, III, IV heart failure, in the absence of severe LV dysfunction (severe LV dysfunction is defined as an ejection fraction less than 30%) and/or ESR greater than 55 mm. (Confidence level: B)
- 3. Asymptomatic patients with chronic severe mitral regurgitation and mild to moderate LV dysfunction, ejection fraction 30-60% and/or ESR greater than or equal to 40 mm. (Confidence level: B)
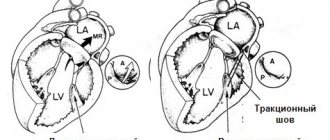
- 4. Mitral valve repair is preferred over mitral valve replacement in most patients with severe chronic mitral regurgitation who require surgery, and patients should be referred to surgical centers with extensive experience in MV repair. (Confidence level: C)
CLASS IIA
- 1. MV repair is indicated in asymptomatic patients with severe chronic mitral regurgitation and normal LV function (ejection fraction greater than 60% and ejection fraction less than 40 mm), in whom the probability of good results of valve repair is greater than 90%. (Confidence level: B)
- 2. Intervention on MV is indicated in asymptomatic patients with severe chronic mitral regurgitation with normal LV function and paroxysmal atrial fibrillation. (Confidence level: C)
- 3. Intervention on MV is indicated in asymptomatic patients with severe chronic mitral regurgitation with preserved LV function and pulmonary hypertension (systolic PA pressure more than 50 mm Hg at rest or more than 60 mm Hg during exercise). (Confidence level: C)
- 4. Intervention on MV is indicated in patients with severe chronic MR*, which developed as a result of primary pathology of the mitral structures, symptoms of NYHA class III-IV and severe LV dysfunction (ejection fraction less than 30% or ESR more than 55 mm), for whom restoration is more suitable MK. (Confidence level: C)
CLASS IIB
- Mitral valve repair is possible in patients with chronic severe mitral valve regurgitation due to severe LV dysfunction (ejection fraction less than 30%), who, despite optimal HF therapy, including a biventricular pacemaker, have symptoms of NYHA class III-IV. (Confidence level: C)
CLASS III
- 1. Mitral valve intervention is not indicated for asymptomatic patients with mitral regurgitation and normal LV function (ejection fraction more than 60% and ejection fraction less than 40 mm), who have significant doubts about the possibility of MV repair. (Confidence level: C)
- 2. Isolated MV surgery is not indicated for patients with mild or moderate mitral regurgitation. (Confidence level: C)
In many cases, the type of operation—plasty or prosthetic valve replacement—is important in choosing the timing of the operation. Although the type of surgical intervention is never actually determined before surgery, in many cases the choice of surgical intervention can be determined in advance. Mortality during planned operations for mitral regurgitation after mitral valve replacement is 2–7%, after mitral valve repair 1–4%. Currently, three main methods of correcting mitral regurgitation are used: valve plastic surgery, mitral valve replacement with partial or complete preservation of the chordal apparatus, and mitral valve replacement without preservation of the chordal apparatus. In most cases, valve repair is the procedure of choice and should be performed whenever possible.
Timely surgical intervention allows one to achieve good results in surgical correction of heart defects, reduces the degree of surgical risk and improves long-term results of surgical treatment.
Pathogenesis of disease development
Thickening of the mitral valve leaflets
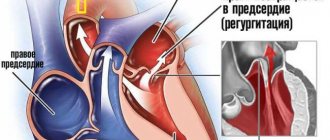
Stretching and thickening of the mitral valve leaflets causes a violation of the closure of the latter, which contributes (due to higher pressure in the left ventricle than in the left atrium) to the return of blood into the cavity of the left atrium. This in turn causes hyperfunction with subsequent hypertrophy of the left atrium and relative insufficiency of the pulmonary vein valves, and subsequently hypertension in the pulmonary circulation, which causes most of the symptoms of this disease.
Depending on the thickness of the valve leaflets, the following stages of the disease are distinguished:
I degree - the valves are thickened to 3-5 millimeters, while the closure of the valve is not impaired, so the patient has no clinical manifestations, because of this, it is possible to identify the disease at this stage only when examining diseases of other systems or during preventive examinations.
Stage I mitral valve myxomatosis does not require any special treatment, there are not even restrictions on physical activity, the main thing is to lead a healthy lifestyle, try not to get sick from various viral and streptococcal infections and periodically carry out preventive examinations (most often recommended 2 times a year).
Degenerative mitral valve disease
II degree - thickening of the valves reaches 5-8 millimeters, valve closure is impaired, and backflow of blood is observed. Also, during the examination, isolated detachments of the chord and deformation of the mitral valve contour are detected. At this stage, the doctor describes the lifestyle, nutrition and frequency of preventive examinations.
III degree - the thickening of the valves exceeds 8 millimeters, the valve does not close, and complete detachments of the chord are observed. In this case, the patient’s condition sharply worsens, symptoms of acute left ventricular failure arise, therefore, emergency specialized treatment of this patient is necessary, and early seeking medical help is very important at this stage.
Etiology of mitral regurgitation:
- Congenital pathology: cleft valve, prolapse, etc.
- Ischemic mitral valve dysfunction in ischemic heart disease.
- Degenerative processes: myxomatous degeneration, Marfan and Ehlers-Danlos syndromes, mitral annulus calcification.
- Inflammatory lesions: rheumatism, systemic lupus erythematosus, systemic scleroderma, aortoarteritis.
- Infection: infective endocarditis.
- Injury.
According to the course, mitral regurgitation is divided into chronic and acute and, accordingly, requires a different approach when determining the indications for the urgency of surgical intervention.
Correction of chronic mitral regurgitation must be carried out before left ventricular decompensation develops, taking into account echocardiography criteria for assessing the severity of mitral regurgitation. The development of acute mitral regurgitation, refractory to drug therapy, is an indication for emergency surgery.
The manifestation of clinical symptoms of mitral regurgitation is determined by the severity of mitral valve insufficiency and the functional state of the left ventricle.
MV degeneration - clinical manifestations
Shortness of breath on exertion
The clinical picture of this disease directly depends on the stage of the disease and the degree of compensation of the body.
The first degree in the vast majority of cases has no clinical manifestations, since there is no regurgitation (backflow of blood) and, in general, the hemodynamics of the body are not disturbed. Of course, general symptoms may occur - dizziness, increased fatigue, decreased exercise tolerance, but these symptoms occur in a huge variety of other diseases and even in completely healthy people.
In the second degree, there are already small detachments of the chord, and there is also regurgitation, although its level is not critical, but the patient will feel it physiologically and clinically. There is a decrease in performance, general weakness, and troublesome shortness of breath during physical exertion, and under such exertion, under which there were no such symptoms before (for example, climbing to the third floor).
Also, such patients may be bothered by tingling in the heart area, rhythm disturbance, which also begins after short physical activity.
But all these symptoms may not exist; if you notice at least a few of these, then you should immediately consult a doctor, because early treatment increases the chances of a full recovery several times.
Foamy cough streaked with blood
For the third degree, due to the depletion of the body’s compensatory ability, all of the above symptoms are characteristic, but since due to the complete separation of the chord, the closure of the valves is severely impaired or absent altogether, the symptoms will be very pronounced. The patient complains of severe shortness of breath even with the slightest physical exertion, and is also sometimes bothered by a cough, often foamy, streaked with blood.
I am worried about dizziness, which often leads to fainting. Sometimes patients are bothered by angina pain in the heart area, which does not subside even after taking nitrate drugs such as nitroglycerin. At this stage, any delay in providing qualified medical care can lead to death.
Diagnostic algorithm for suspected MD MK
General clinical tests
Mitral valve degeneration is diagnosed based on the patient’s complaints, which we discussed above (in the section “Mitral valve degeneration - clinical manifestations”), but even in their absence, the patient should be examined using special methods, which we will discuss below.
Next, the doctor prescribes general clinical tests to the patient, such as a complete blood count, a general urinalysis and a biochemical blood test. Most often, there are no changes in them, but with the third degree of insufficiency, a general blood test may reveal anemia or, conversely, signs of blood thickening (an increase in the level of red blood cells, platelets, hemoglobin and a decrease in the level of ESR), this is due to the release of the liquid part of the blood into the third space (lungs ).
Ultrasound examination of the heart with Doppler measurements
The “gold” standard for detecting valve insufficiency and chord rupture is an ultrasound examination of the heart with Doppler. This method allows us to identify the stage and degree of decompensation of the disease, and this can be done even before the child is born, which means it can be detected early and early treatment can be prescribed.
Not highly specific methods, but necessary for early diagnosis of the disease, are ECG examination and X-ray examination of the chest organs. In the first case, we will identify signs of hypertrophy of the left parts of the heart, and in the third stage hypertrophy of the right parts of the heart will also join, various supraventricular tachyarrhythmias such as atrial fibrillation or flutter, supraventricular extrasystoles are also detected.
And an X-ray examination will show signs of pulmonary hypertension, bulging of the left atrium arch, as well as expansion of the borders of the heart (in the third stage, the development of a “bull” heart).
To clarify the diagnosis, special research methods can be used - catheterization of the left and right ventricles, as well as left ventriculography, which will help clarify the presence of the disease and its degree.
Diagnosis of mitral insufficiency
Echocardiography (ECHOCG)
occupies a leading place in the diagnosis of mitral valve insufficiency and determination of indications for patient management tactics. If transthoracic echocardiography is insufficiently informative and the possibility of reconstructive surgery on the mitral valve is clarified, transesophageal echocardiography should be performed.
Echocardiography allows you to determine the etiology of mitral regurgitation, its severity - the compensatory capabilities of the left ventricle, the presence of complications (left ventricular failure, pulmonary hypertension, right ventricular failure), and identify other heart defects.
An echocardiography study allows one to assess the degree of mitral valve insufficiency based on the ratio of the area of regurgitation flow to the area of the left atrium:
- Minor mitral valve insufficiency less than 20%
- Moderate deficiency 20-40%
- Severe deficiency 40%
If ischemic heart disease is not the cause of mitral regurgitation and there is no evidence of concomitant ischemic heart disease, indications for surgery can be determined without cardiac catheterization.
The use of invasive examination methods is indicated for patients with ischemic mitral valve dysfunction:
Coronary angiography makes it possible to clarify the presence of stenotic lesions of the coronary arteries and determine indications for myocardial revascularization in combination with surgical correction of mitral regurgitation.
Indications for surgical treatment of mitral insufficiency
Classification of recommendations and levels of evidence in ACC/AAC format:
- Class I: Conditions for which there is evidence and/or general agreement that a procedure or treatment is beneficial, useful and effective.
- Class II: Conditions for which there is conflicting evidence and/or differences of opinion about the usefulness/efficacy of a procedure or treatment.
- Class IIA: Weight credibility/opinion in favor of usefulness/effectiveness.
- Class IIB: Benefit/effectiveness less well established by evidence/opinion.
- Class III: Conditions for which there is evidence and/or general consensus that the procedure/treatment is not beneficial, not effective, and in some cases may be harmful.
In addition, the levels of evidence to support the recommendations are outlined as follows:
- Level of Evidence A: Data are from multiple randomized clinical trials.
- Level of Evidence B: Data are from single randomized trials or non-randomized trials.
- Level of Evidence C: Expert consensus only, individual case studies and standards of care.