The mitral valve is one of the four heart valves. It opens and closes to control blood flow between the left atrium and the left ventricle. The valve consists of two valves - front and rear.
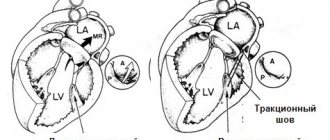
With mitral valve prolapse, one or both valve leaflets are too large or the chordae (ligaments attached to the underside of the leaflets and connected to the ventricular wall) are too long. Due to such a violation, the valve bends back or is “sucked” into the left atrium, taking on the appearance of a parachute.
Additionally, during each heartbeat, the valve does not close tightly enough, which leads to the return of a portion of blood from the ventricle to the atrium.
What is MVP (mitral valve prolapse)?
Mitral valve prolapse (MVP) is a cardiac anomaly and one of the most common heart pathologies.
In the presence of this pathology, the mitral valve leaflets sag/bulge into the atrium cavity; this occurs at the moment of contraction of the left ventricle of the heart. As a result of this cardiac abnormality, regurgitation can occur, where some blood flows back into the left atrium. This pathology is benign (unlike heart defects, for example), but, unfortunately, it can also have serious unpleasant consequences. Severe regurgitation can cause disability. In some cases, mitral valve prolapse requires serious treatment (medical or even surgical), in others, doctors limit themselves to only monitoring the patient; the person must undergo regular examinations and monitor his lifestyle. Very often a person does not know that he has PMH and this anomaly is discovered during a medical examination on some other issue, since the symptoms of this disease are often non-specific: headache, fatigue, dizziness, cardiac pain. Therefore, it is very important if you have health problems, even if it is mild fatigue or malaise, which is long-lasting, not to put off visiting a doctor.
Does the prognosis change for people with MVP?
Mitral valve prolapse is a benign pathology.
But the forecast directly depends on the following factors:
- degree of prolapse;
- regurgitation is present or absent;
- Are there any complications?
With minor prolapse (1st degree without regurgitation or with 1st degree regurgitation), the prognosis is favorable. This pathology does not affect life expectancy.
For prolapse with 2nd degree regurgitation, in addition to taking medications, it is important for patients to follow a restrictive regimen. For example, boxing, weightlifting, and professional running are contraindicated for patients. Young people have restrictions on their suitability for military service. At the military medical commission, depending on the presence of complications, they are assigned categories “B”, “C”, and “D”.
Possible and negative consequences
Despite its apparent harmlessness, mitral valve prolapse is dangerous due to complications that can become a real threat to the patient’s life.
Adverse effects of MVP include:
- chronic heart failure - due to regurgitation, some of the blood does not enter the aorta, so the left ventricle is forced to compensatory hypertrophy (thicken). Over time, this will lead to its dysfunction and deterioration of blood circulation throughout the body;
- heart rhythm disturbances (atrial fibrillation, prolongation of the QT interval, paroxysmal supraventricular and ventricular tachycardia). Regurgitation leads to stretching and expansion of the cavity of the left atrium, in the wall of which foci of pathological electrical activity may appear;
- ischemic stroke - a vortex flow of blood is created in the dilated cavity of the left atrium, which contributes to its thickening and the formation of blood clots;
- acute mitral regurgitation - with a pronounced degree of prolapse and regurgitation, the tendon threads that are attached to the valves are strongly stretched. As a result, their rupture and sudden overload of the parts of the heart located on the left are possible;
- infective endocarditis - during some medical procedures (tooth extraction, catheter installation, bronchoscopy), a small amount of bacteria enters the general bloodstream. With prolapse, they can settle on the valve flaps and begin to multiply. To prevent this, people with MVP are advised to take antibiotics before procedures.
These complications can quickly lead to the death of the patient.
Mitral valve prolapse: causes
There are 2 types of mitral valve prolapse - primary and secondary, depending on the origin of the pathology.
The causes of primary mitral valve prolapse are genetic defects. This issue has not yet been fully studied, but there is evidence that MVP is a disease that is inherited. In addition, negative factors that have a negative effect on the fetus while still in the womb can affect the possibility of a person developing MVP. Such factors include viral diseases of the mother during pregnancy, gestosis, and poor environmental conditions.
Primary MVP is divided into:
- Mitral valve prolapse as an independent disease.
- Mitral valve prolapse as a manifestation of connective tissue development disorders (connective tissue dysplasia, Marfan syndrome, Ehlers-Danlos syndrome). In this case, the pathology, in addition to MVP, can be manifested by hypermobility of the joints, curvature of the spine, deformation of the chest; a person often experiences dislocations and subluxations of the joints, and other symptoms.
The causes of secondary MVP are other diseases, and it is against their background that secondary cardiac prolapse occurs:
- congenital heart defects;
- acquired heart defects;
- ICHD (coronary heart disease);
- myocarditis;
- rheumatic heart disease;
- cardiomyopathy.
Pathogenesis of MVP.
The mitral valve separates the cavities of the ventricle of the heart and its left atrium. When the mitral valve is normal, its leaflets are “deviated” downward at the moment the myocardium relaxes and the cavities of the heart are filled with blood, and vice versa – the leaflets are “raised” upward at the moment of atrial contraction, the left atrioventricular orifice is closed. With MVP, the valve does not work correctly: during the phase of atrial contraction, the valve leaflets “bend” into the cavity of the left atrium, but this should not be the case. Indeed, for this reason, the atrioventricular opening is completely or partially blocked and a reverse movement of blood occurs from the left ventricle to the left atrium (mitral regurgitation).
If a person has mitral valve prolapse, the ability of the heart muscle to contract may decrease, which in turn can lead to circulatory failure; The presence of arterial hypotension, borderline pulmonary hypertension, metabolic disorders and dysfunction of the autonomic nervous system may also be noted.
The mechanism of pathology development
Grade 1 MVP is a defect of the mitral valve. Normally, the anatomical structure acts as a partition between the left atrium and the ventricle of the same name.
Blood moves strictly in one direction - from the atria to the ventricles. Against the background of the described condition, a reverse flow of liquid connective tissue is observed. The mitral valve is weak, its leaflets fall into the previous chamber, making regurgitation possible. The amount of blood in the left ventricle decreases.
The severity depends on the amount of regurgitation. The larger it is, the smaller the volume of ejection into the aorta and, accordingly, the large circle.
General hemodynamics drops, lack of nutrition affects all organs and systems. Brain, kidneys, liver, including the heart itself: the coronary arteries do not bring enough nutrients and oxygen.
In some cases, the process at stage 1 continues for years. Since the volume of regurgitation (reverse blood flow) is minimal (no more than 10-15%), the patient may not notice any abnormalities in his own condition.
Progression occurs, but for some within a couple of months, for others for decades the degree of deviation does not change. Based on the dynamics of the process, the doctor decides on treatment tactics. Stagnating forms do not require immediate surgical therapy.
Mitral valve prolapse: symptoms.
Mitral valve prolapse can occur either with pronounced symptoms or absolutely “quietly”, without making itself felt. It is necessary to pay attention to the body’s signals, including “simple” headaches and fatigue, do not attribute them, for example, to stress, do not ignore them and find the cause.
In children and adolescents, quite often the disease is asymptomatic or accompanied by only minor discomfort in the chest area. Also, in the presence of primary MVP, diseases are detected in children that indicate a disorder in the development of connective tissue:
- scoliosis;
- chest deformation;
- joint hypermobility;
- hip dysplasia;
- flat feet;
- hernias (umbilical, inguinal);
- nephroptosis, etc.
At the same time, it is possible to identify symptoms characteristic of mitral valve prolapse:
- low blood pressure, resulting in dizziness;
- rapid heartbeat;
- feeling that the heart is working “intermittently”;
- pre-fainting state, which is manifested, among other things, by a feeling of nausea, spots before the eyes;
- pressing or squeezing (sometimes stabbing) pain behind the sternum or in the chest (its left side) - can appear both from physical activity, stress, and for no specific reason;
- feeling of constant fatigue, breathing problems (difficult), swelling of the legs, pain in the right side (the cause of the pain is an enlarged liver).
Secondary MVP is also supplemented by symptoms of the patient’s underlying disease - Marfan syndrome, heart defects (congenital), rheumatic carditis.
Expert advice: treatment of MVP for connective tissue dysplasia
People suffering from hereditary connective tissue disorders have a magnesium deficiency. This microelement promotes the formation of collagen fibers, and consequently the strengthening of connective tissue. Therefore, I recommend that such patients include foods rich in magnesium in their diet: oatmeal, bananas, nuts, buckwheat and others. It is also worth taking additional dietary supplements: Magne B6, Magnerot. To improve magnesium absorption, you can add ascorbic acid.
Degrees of mitral valve prolapse (classification).
Mitral valve prolapse is classified into primary and secondary (according to the origin of the disease), into prolapse of the anterior, posterior and both valve leaflets (according to location.
According to severity, 3 degrees of MVP are determined
- I degree - the valve leaflets “fall out” by 3–6 mm, the closure of the mitral valve leaflets is complete (for this reason, degree I MVP can be asymptomatic).
- Stage II - the valve leaflets “fall out” by 7–9 mm, the mitral valve leaflets do not close tightly, and there is a backflow of blood from the ventricle into the atrium (returgitation).
- III degree - valve flaps “fall out” over 9 mm.
In addition, doctors separately classify the severity of mitral regurgitation (reverse movement of blood from the left ventricle to the left atrium):
- I degree - reverse movement of blood occurs at the level of the valves;
- II degree - the wave of regurgitation reaches the middle of the left atrium;
- III degree - the regurgitation wave passes more than half of the atrium;
- IV degree - the wave of regurgitation reaches the opposite end of the atrium.
Forecast
Favorable in the first stage of mitral valve prolapse. Surgery is not always necessary. Survival rate is maximum and is almost 100%. With rapid progression of the disease, the probability is slightly lower. It correlates with the speed of the violation.
Negative factors significantly worsen the prognosis, first for the course of prolapse, and then for life in general.
Among the unfavorable points:
- Bad family history. There is partial genetic causation. At least predispositions.
- The presence of somatic concomitant pathologies.
- Poor response to treatment.
- Impossibility of surgical intervention when indicated.
- Age over 50 years.
- Several heart defects at the same time.
- Genetic nature of the deviation.
- Being male.
The more negative aspects, the worse the prognosis for the development of the condition.
- Prolapse of the anterior leaflet of the mitral valve, grade 1
Diagnosis of PMC.
Mitral valve prolapse in the vast majority of cases is detected using non-invasive examinations, the final diagnosis is made using echocardiography, and a number of other studies are also used:
- Interviewing the patient for complaints, collecting anamnesis.
- General blood analysis.
- Blood chemistry.
- Auscultatory examination. The doctor listens to the heart with a stethoscope and can detect a specific click and/or systolic murmur at the apex of the heart that is characteristic of the disease - these sounds decrease with the patient standing, sitting or lying down.
- Electrocardiography (ECG). On it, the doctor can see nonspecific changes in the ST segment and T wave in leads III and aVF, as well as “short PQ syndrome”) and supraventricular tachycardia.
- Echocardiography (ultrasound of the heart). Here the doctor can detect such signs of disease as sagging of the mitral valve leaflets (posterior or both at once) into the cavity of the left atrium in mid-systole, in late systole or throughout systole. Echocardiography is one of the most important examinations in diagnosing MVP in a patient.
- Chest X-ray. It may show signs of smoothed lordosis (but it may also be normal).
- MRI (chest).
After all the studies, the cardiologist prescribes the necessary treatment.
Diagnosis criteria
To make an accurate diagnosis, I use specially developed criteria:
- The main ones.
- Additional.
- Non-specific.
The first include:
- late systolic click/click, late systolic murmur at the apex of the heart on auscultation. Sometimes, in order to better listen to the noise, I resort to some tricks: I ask the patient to do 10 squats or lie on his left side;
- displacement of the leaflets at the time of ventricular systole, prolapse (bending) of the leaflets more than 3 mm.
Additional criteria:
- neurotic disorders;
- the presence of MVP in close relatives (father, mother, grandparents, siblings);
- The patient’s appearance is tall, thin, long arms and legs, malocclusion, deformities of the chest or spine.
Non-specific criteria include:
- patient complaints - pain in the heart, difficulty breathing, rapid heartbeat, panic attacks;
- changes on the ECG film - negative T wave in leads II, III, aVF, frequent extrasystoles and slowing of intraventricular conduction.
The presence of 2 main criteria or one main and 2 additional criteria allows one to reliably make a diagnosis of mitral valve prolapse. In addition, these criteria help to carry out differential diagnosis, that is, to distinguish MVP from acquired heart defects.
Mitral valve prolapse: treatment.
Treatment for MVP can only be prescribed by a cardiologist; it is required if a person has pain in the heart and there is an abnormal heart rhythm.
Factors influencing the need for treatment:
- degree of “fallout” of the valve leaflet;
- presence of returgitation;
- presence of complications.
In case of grade I MVP and the person does not have any complications, pain, or discomfort, treatment is not required. However, it is necessary to quit smoking and consume large quantities of coffee; It is important to constantly visit a doctor and get examined.
For grade I MVP with grade I regurgitation and degree II and III MVP (especially if cardiac arrhythmias and/or circulatory failure are detected), drug therapy is prescribed. In addition, in difficult cases, surgical treatment is prescribed.
It is also recommended for patients diagnosed with MVP:
- avoid excessive physical activity, avoid overwork; physical activity should be moderate;
- give up smoking, alcohol, coffee and strong tea;
- maintain a sleep schedule;
- eat a balanced diet.
Nutrition
The diagnosis of Barlow's disease requires the patient to reconsider his habits and lifestyle. To avoid excessive stress, it is necessary to avoid the abuse of alcohol and caffeine, avoid smoking, and intense physical exercise.
The cardiovascular system is negatively affected by excess fat and salt. If you have MVP, you should avoid or minimize the consumption of fatty meat dishes, store-bought confectionery, smoked meats, marinades, fatty and hot sauces, and snacks with a high salt content. The choice of products for MVP is quite wide. The body should receive a sufficient amount of potassium and magnesium and vitamins. The optimal diet is one that includes lean meat, fresh and baked vegetables, fruits, vegetable oils, fish and seafood, nuts, milk and low-fat dairy products, and cereals. Instead of baked goods and industrially produced flour products, you should eat bread made from wholemeal flour.
Honey, dried apricots, prunes, raisins, dates are suitable as a dessert. It is better to drink tea and coffee with milk. Sources of heart-healthy magnesium include almonds, oatmeal, cashews, pumpkin seeds, and buckwheat. Potassium is found in dried apricots, raisins, beans, pumpkin and flax seeds, bananas, and potatoes.
PMC: prognosis and prevention.
In general, the prognosis for MVP is quite favorable, the main thing is constant clinical monitoring of the patient to determine the degree of mitral valve insufficiency. Often, mitral valve prolapse does not affect physical activity (among people with MVP there are professional athletes, dancers, etc.), however, there are signs, the identification of which is an “alarm bell” and leads to a ban on active anaerobic exercise:
- long QT syndrome;
- Marfan syndrome;
- history of loss of consciousness (without reason);
- left ventricular dysfunction;
- attacks of atrial tachycardia;
- severe mitral regurgitation.
All patients with MVP need to monitor their health, avoid frequent infections and be sure to treat them if they occur.
Prevention of MVP is the absence of adverse effects on the health of the pregnant woman and the fetus developing in the womb, timely diagnosis and treatment of diseases that damage the valvular apparatus of the heart.
Do not under any circumstances neglect the diagnosis of MVP and always strictly follow the doctor’s recommendations!
Case study: a woman with arrhythmias and prolapse
I would like to present to you a case of arrhythmia caused by mitral valve prolapse.
A 38-year-old woman approached me. For a long time, she was worried about “interruptions in the heart,” an irregular pulse, as well as episodes of rapid heartbeat, during which her well-being significantly worsened, which manifested itself in the form of nausea and dizziness. During the last such attack, the woman fainted, which is why she got scared and decided to turn to me. During the general examination, the patient’s thinness and tall stature were striking. During the examination, it was possible to note hypermobility of the elbow and wrist joints. The woman also said that as a child she often had dislocations in her arm joints. I ordered Holter ECG monitoring and echocardiography, which showed QT prolongation, episodes of torsade de pointes (TdP), and leaflet prolapse of 7 mm without signs of regurgitation. Based on the results, I made a diagnosis: grade 2 mitral valve prolapse without regurgitation with complications (prolonged QT interval, PVT, CHF class 0). I prescribed Bisoprolol (1 tablet once a day) and Magne B6 (2 tablets 3 times a day). I also provided the patient with a list of foods high in magnesium.
When taken again after 3 months, the woman noted a significant improvement: her pulse returned to normal and the attacks stopped. And the ECG showed no signs of heart rhythm disturbances.