General information
The term “Hypercholesterolemia” usually means increased cholesterol levels in the blood (more than 5.18 mmol/l). Hypercholesterolemia is a special case of the concept of dyslipidemia . At the same time, an increase in the concentration of cholesterol in the blood is not a disease as such, but only a symptom (laboratory indicator). ICD-10 hypercholesterolemia code: E78.0 (pure hypercholesterolemia).
A little about cholesterol and lipid metabolism
Cholesterol is a natural lipophilic alcohol that is present in human cell membranes. Most of it is produced by the body (about 80%) by the liver, adrenal glands, kidneys, and intestines, and the rest is ingested with food. Cholesterol is insoluble in water, but soluble in organic solvents/fats. Circulates in the blood in the form of a compound (complex) of lipid (fat) and protein, called lipoproteins.
There are several types of lipoproteins depending on their density:
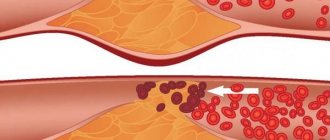
- Low-density lipoproteins (abbreviated LDL). Their main function is the transfer of cholesterol from liver cells to other cells of the body tissues. LDL is considered to be “bad” cholesterol, since it is directly involved in the formation of atherosclerotic plaques. And the higher the LDL level, the greater the risk of cardiovascular disease.
- High-density lipoproteins (abbrev. HDL). Their function is exactly the opposite - they carry cholesterol back to the liver, where it is broken down/excreted from the body. HDL is classified as “good” cholesterol and does not participate in the formation of plaques. That is, the higher the HDL cholesterol level, the lower the risk of developing cardiovascular diseases.
- Triglycerides . They represent the form of existence of fats in the body, in particular in the blood plasma, where they, in combination with cholesterol, form blood fats (plasma lipids).
- High-density lipoproteins (HDL) transport the same cholesterol, but HDL cholesterol does not participate in the formation of plaques, but removes excess “bad cholesterol” from body tissues. That's why HDL cholesterol is called "good" cholesterol.
There are standard indicators for the content of fat fractions in the blood (lipoproteins), which are:
- Total cholesterol content is less than 5.2 mmol/l.
- Triglycerides - less than 2.0 mmol/l.
- LDL - less than 3-3.5 mmol/l.
- HDL - more than 1.0 mmol/l.
Hypercholesterolemia has traditionally been considered as a leading factor in the development of cardiovascular diseases caused by atherothrombosis and, above all, coronary heart disease , peripheral arterial diseases/cerebrovascular diseases.
A direct relationship has been reliably established between blood cholesterol levels and mortality rates from coronary artery disease. The prevalence of hypercholesterolemia in Russia reaches 58.4%; elevated LDL cholesterol levels - in 59.7% of cases, and decreased HDL cholesterol levels - in almost 20% of cases. It was found that a decrease in LDL cholesterol significantly correlates with an improvement in the clinical course of coronary artery disease and mortality rates from it.
Forecast for the development of complications
The occurrence of coronary heart disease in patients with hypercholesterolemia who do not have a diagnosis of “atherosclerotic disease” is determined by the following number of factors:
- Arterial hypertension (systolic pressure ≥ 140 mm Hg);
- Consumption of tobacco products (any amount in the past month);
- HDL level below 40 mg/dl;
- Men and women 45 years of age and older;
- Presence of a negative family history: clinical ischemic disease or sudden death under 55 years of age in the male line or women under 65 years of age.
In turn, an HDL content of 65 mg/dl or more is a favorable factor that reduces the likelihood of coronary disease.
The risk of complications can be significantly reduced with the timely use of drug therapy aimed at reducing plasma cholesterol. It has been established that a decrease in this organic substance by 1% reduces the risk of sclerosis of the coronary arteries by 2%.
Body weight control, low-fat diets, and high daily physical activity have a significant effect on total cholesterol concentrations and increase the quality and length of life.
Irina Kostyleva
Pathogenesis
The pathogenesis of dyslipidemia depends on its type - primary or secondary. It has been established that familial dyslipidemia (primary) is based on genetically determined factors (mutations in the genes encoding LDL receptor proteins), inherited in an autosomal dominant manner and causing homozygous/heterozygous hypercholesterolemia . The accumulation of LDL is caused by a decrease in the activity of the receptor, which is responsible for the excretion of lipoproteins. It is their accumulation in the subendothelial space that underlies the formation of atherosclerotic plaques. Moreover, the higher the LDL level, the higher the intensity of the process. When inherited, gene mutations can cause overproduction (high levels of LDL) or underproduction/overexcretion of HDL. LDL is especially poorly excreted in individuals with homozygous hypercholesterolemia, since the mutation is present in two paired genes, which significantly reduces the functionality of the receptor and is poorly corrected by drug treatment and dietary nutrition. In cases of heterozygous type hypercholesterolemia, only one gene is defective, that is, half of the receptors retain their functions, therefore, despite the increase in LDL, clinical manifestations are absent for a long time.
The pathogenesis of secondary hypercholesterolemia is based on excessive intake of cholesterol from high-calorie foods or an increase in the concentration of LDL, due to its increased synthesis in various diseases ( obesity , endocrine pathologies , kidney diseases , etc.) or taking various medications.
Classification
The classification of hypercholesterolemia is based on a number of factors.
By origin they are distinguished:
- Primary (family) - heterozygous , in which genetic mutations in genes are inherited from both parents, and homozygous , in which a defect in genes is inherited from only one of the parents.
- Polygenic . Caused by a combination of exposure to unfavorable exogenous factors (smoking, nutrition, etc.).
- Secondary . The pathology of cholesterol metabolism develops against the background of endocrine disorders, certain diseases, or taking medications.
According to the degree of increase in the concentration of cholesterol in the blood, they are distinguished:
- Mild hypercholesterolemia - LDL is quantitatively increased within the range of 5.0 - 6.4 mmol/l.
- Moderate hypercholesterolemia - LDL is quantitatively increased within the range of 6.5 - 7.8 mmol/l.
- High hypercholesterolemia – elevated cholesterol levels within 7.9 mmol/l and above.
Also in practice, the Friederikson classification is used, based on the predominance of various cholesterol fractions (table below).
Causes
The etiological factors of hypercholesterolemia vary significantly depending on its type.
Hereditary hypercholesterolemia . Caused by mutations in various genes that are responsible for the process of encoding the expression of lipoprotein receptors (PCSK9, LDLR, ApoB-100), or a specific enzyme - lipoprotein lipase . As a result, catabolism is impaired, contributing to a significant increase in blood cholesterol levels. Familial forms of hypercholesterolemia are characterized by high cholesterol concentrations from early childhood (in homozygous patients up to 20 mmol/l), which is associated with the rapid development of atherosclerosis by the age of 25 and a high risk of cardiovascular complications. Aggressive lipid-lowering treatment is necessary.
Physiological reasons . They occur mainly against the background of physiological changes in hormonal balance, for example, during pregnancy or heavy consumption of fatty foods before donating blood for analysis.
The most common causes of secondary hypercholesterolemia are:
- Obesity . Among etiological factors, excess weight is the leading cause of hypercholesterolemia. It develops against the background of the formation of insulin resistance, which leads to activation of lipolysis and accelerated release of FFA (free fatty acids), from which one of the cholesterol fractions (VLDL) is synthesized in the liver. Hypercholesterolemia increases in proportion to the degree of obesity, but can return to normal against the backdrop of normalization of body weight, but it can become irreversible over a long course.
- Kidney diseases . As a rule, these are diseases that are accompanied by nephrotic syndrome: nephropathy (diabetic/hypertensive), glomerulonephritis in the initial stage, which is caused by the loss of enzymes involved in the processes of lipid catabolism (lipoprotein lipase/lecithin-cholesterol acetyltransferase), as well as carrier proteins with urine. The level of hypercholesterolemia significantly correlates with the severity of proteinuria . After relieving nephrotic syndrome, as a rule, cholesterol levels return to normal.
Endocrine disorders . Hypercholesterolemia develops against the background of excessive/insufficient production of one or another hormone, which causes lipid metabolism disorders. Such disorders include:
- Diabetes mellitus type 2 . The degree of cholesterol increase is directly proportional to the severity of diabetes.
- Syndrome/ Itsenko-Cushing's disease . Hypercortisolism increases cholesterol levels both indirectly and directly.
- Hypothyroidism . A decrease in the level of thyroid hormones causes a slowdown in the process of VLDL catabolism and the process of transformation of cholesterol into bile acids. The process is reversible. Hypercholesterolemia disappears after hormone replacement therapy.
Cholestasis . Occurs in diseases of the liver/biliary tract, accompanied by stagnation of bile - hepatitis (alcoholic, viral), fatty liver . Hypercholesterolemia is caused by a violation of the process of cholesterol utilization, and its degree directly correlates with the severity of cholestasis.
Autoimmune diseases ( hypergammaglobulinemia / systemic lupus erythematosus ).
Mental illness ( anorexia nervosa).
Metabolic disorders (storage diseases, gout ).
Taking oral contraceptives/medicines (beta-blockers, immunosuppressants, thiazide diuretics, etc.).
The main risk factors for the development of hypercholesterolemia include:
- age (after 45 years)
- male gender;
- physical inactivity;
- Poor nutrition (excessive consumption of animal fats).
Correction
Conservative therapy
If hypercholesterolemia is detected, it is imperative to consult a doctor to find out the cause of this laboratory phenomenon and select appropriate treatment. Much attention is paid to the fight against the underlying disease (immunosuppressive therapy for nephrotic syndrome, hormone replacement therapy for hypothyroidism, choleretic therapy for cholestasis), since its elimination can lead to normalization of cholesterol levels without additional intervention.
Non-drug methods for correcting hypercholesterolemia include complete smoking cessation and limiting alcohol consumption. Also, in order to reduce body weight, obese patients must follow a diet with a decrease in the proportion of animal fats in the diet (butter, fried meat, sausages) and an increase in vegetable fats (vegetables, seafood), fruits and whole grains, and regularly perform various physical exercises.
For the drug correction of hypercholesterolemia, the following drugs are used:
- Statins
(atorvastatin, rosuvastatin). The most effective and frequently prescribed means to reduce cholesterol levels. The mechanism of action is based on the suppression of cholesterol synthesis in the liver. - Fibrates
(clofibrate). These drugs stimulate the activity of the LPL enzyme, thereby accelerating the degradation of the drug. They reduce not only cholesterol, but also triglycerides, so they often become the drugs of choice for patients suffering from diabetes. - Ezetimibe
. Inhibits the absorption of cholesterol in the intestine. Used in combination with statins. - PCSK9 inhibitors
(alirocumab). These are monoclonal antibodies that bind to LDL receptors in the liver, which stimulates the breakdown of lipoproteins. Prescribed when statins are ineffective. - Bile acid sequestrants
(cholestyramine, colestipol). They are ion exchange resins that suppress the absorption of bile acids in the intestine. Depletion of FA reserves activates their synthesis from cholesterol in the liver. Used in patients with cholestasis. - A nicotinic acid
. This drug reduces the flow of fatty acids into the liver, which suppresses the synthesis of lipid. It has a weak hypocholesterolemic effect, therefore it is used as an addition to other drugs. - Omega-3 fatty acids
. Eicosapentaenoic acid and docosahexaenoic acid are components of fish oil. These substances bind to the nuclear PPAR receptors of liver cells, which leads to a decrease in serum lipid levels.
Surgery
One of the prerequisites for the effective treatment of hypercholesterolemia is normalization of body weight. For patients with morbid obesity (body mass index above 40), especially in combination with type 2 diabetes mellitus, if conservative methods are unsuccessful, bariatric surgery is indicated - gastric banding, gastric bypass or resection.
If hypercholesterolemia is caused by cholestasis due to cholelithiasis, surgical removal of the gallbladder (cholecystectomy) is performed. Patients with Cushing's disease undergo endoscopic transnasal adenomectomy (removal of the pituitary adenoma). For Itsenko-Cushing syndrome, bilateral adrenalectomy is used.
Symptoms
Hypercholesterolemia, in itself, is predominantly asymptomatic, however, as already indicated, it can cause vascular damage, which is manifested by clinical symptoms of coronary heart disease , peripheral artery disease, and stroke . Symptoms of hypercholesterolemia are present in a minority of patients. Most often these are tendon xanthomas, which are compactions of cholesterol in the form of nodules that can be felt over the tendons.
With high levels of LDL against the background of familial hypercholesterolemia in the homozygous form a corneal arch (arc-shaped opacification of the cornea), as well as characteristic xanthomas of the knee, elbow, Achilles tendon and tendons in the area of the carpophalangeal joints, may appear. Another manifestation may be xanthelasmas, which are cholesterol deposits under the skin of the eyelids in the form of yellow plaques located in the medial part of the eyelids.
In advanced cases, mosaic symptoms of damage to internal organs develop (at the stage of development of atherosclerosis ).
What does pathology affect?
The syndrome affects pathological changes in the structure of the vascular membranes of the blood flow system throughout the body of a sick person.
These violations manifest themselves:
- In changes in the lumen of the main arteries of large diameter;
- In lesions of the coronary arteries;
- In disorders in the vascular wall of cerebral vessels;
- In a pathological change in the structure of the cardiac myocardium;
- In violations of blood patency in small capillaries of the extremities and the entire peripheral sphere of the blood flow system;
- Disturbances in internal organs and in the vessels of these organs.
A complicated form of hyperlipidemia is atherosclerosis, which affects all vessels in the bloodstream and causes serious diseases that can be fatal.
Tests and diagnostics
The diagnosis is based on the collection of personal/family history (patient’s age, presence of hypercholesterolemia in relatives, medication use), physical examination (presence of xanthoma and/or lipoid arch of the cornea). The main informative diagnostic method is a lipidogram (lipid profile study), which allows you to determine the level of total cholesterol and LDL level.
Much less frequently, genetic screening is carried out to identify mutations and their nature. If necessary, hormonal studies are carried out (concentration of thyroid hormones, TSH, cortisol levels in the blood) and immunological tests (markers of viral hepatitis, antimitochondrial/antineutrophil antibodies).
To identify vascular changes, instrumental diagnostic methods can be prescribed - Dopplerography, angiography, magnetic resonance angiography. An abdominal ultrasound may be prescribed to determine the condition of the liver/gallbladder (fatty infiltration of the liver, stones/thickening of the gallbladder walls).
Diet
Diet for high cholesterol
- Efficacy: therapeutic effect after 2 months
- Terms: 2 months or more
- Cost of food: 1700 - 1800 rubles per week
If LDL cholesterol is elevated, this means that, along with drug therapy, it is necessary to organize proper nutrition, since diet therapy is one of the most important conditions for the qualitative/quantitative correction of lipid metabolism disorders. It has been established that an increase in cholesterol intake in a ratio of 100 mg per 1000 kcal/day increases the concentration of cholesterol in the blood by 12%. Limits on dietary intake of exogenous cholesterol should range from 250 to 500 mg/day depending on the type of hyperlipidemia. According to NOPH recommendations, for severe hypercholesterolemia, the amount of cholesterol in the diet should not exceed 200 mg/day, and for moderate hypercholesterolemia, 300 mg/day. For this purpose, products containing a lot of cholesterol are excluded from the diet - fish caviar, brains, fatty cheeses, internal organs of animals, egg yolk, butter, etc.).
The fat content in the daily diet should not exceed 30% of its calorie content (70–80 g/day). At the same time, the share of saturated fatty acids should account for 8–10% (sausages, fatty fish/meat, dairy products, etc.); polyunsaturated acids - 7-9% (butter) and monounsaturated acids - 10-15% (vegetable oils - olive, sunflower, cottonseed, corn, etc.).
It is extremely important to use PUFAs of the omega-3 family in the diet - various fatty sea fish (water herring, mackerel, halibut, sardines, etc.) containing eicosapentaenoic/docosahexaenoic long-chain fatty acids, which take part in the production of leukotrienes, prostaglandins, which have anti-inflammatory, antiplatelet, hypotensive effect.
Phospholipids, which have a hypolipidemic effect and reduce the absorption of cholesterol in the intestine, are also extremely necessary in the diet. Their main source is unrefined vegetable oils. They can also be introduced into the diet in the form of dietary supplements (for example, Vitol ).
In addition to the fat component in the diet, soy protein/isoflavones, as well as dietary fiber, have a significant effect on lipid metabolism. Sources of vegetable protein can be legumes (especially soybeans and products based on it), baked goods, and cereals. Soy isoflavones have a positive effect: consuming 25 g of soy protein daily significantly reduces blood cholesterol levels. An obligatory component of the diet is dietary fiber (pectin, cellulose, hemicellulose), which is achieved by including grains, wheat bran, vegetables, and fruits in the diet, which allows you to fully meet the daily requirement for them (30–50 g).
It is equally important to control the intake of carbohydrates into the body. It has been established that the consumption of refined carbohydrates contributes to an increase in the concentration of low-density lipoproteins/triglycerides in the blood, while the consumption of complex carbohydrates contributes to a decrease in the concentration of atherogenic lipoprotein fractions in the blood serum, excess body weight, and blood pressure levels. And in general, the consumption of refined carbohydrates contributes to an increase in calorie content, an increase in body weight and endogenous cholesterol synthesis (increases by 20 mg/kg of excess body weight).
A number of micronutrients play an important role in the regulation of lipid metabolism:
- Iodine - has a hypocholesterolemic effect, affects the function of the thyroid gland, and prevents the formation of atherosclerotic plaque. Its main sources are seafood: seaweed, sea fish, mussels, shrimp.
- Chromium is involved in lipid metabolism and prevents the process of lipid deposition in the vascular wall. Sources of chromium: legumes, wholemeal wheat/rye flour, baker's yeast, meat, corn/pearl barley.
- Selenium - has antioxidant activity, reduces the risk of atherosclerosis , normalizes blood clotting.
- Vitamins with antioxidant effects - vitamin E (vegetable oils, legumes, nuts, seeds); vitamin A (eggs, liver, chum salmon caviar, butter) and beta-carotene (its precursor (green onions, carrots/red peppers, spinach, sorrel, tomatoes, sea buckthorn, rowan); vitamin C (vegetables/fruits); group vitamins B (milk, meat, fish, liver, seafood, soybeans, beans, buckwheat, millet, cauliflower, green onions, yeast, cauliflower).
Flavonoids contained in vegetables/fruits, legumes, Rosaceae, buckwheat and Asteraceae have biological activity in relation to fat metabolism, which is due to their antioxidant effect. The antioxidant/hypolipidemic effect of squalene, which is contained in amaranth seed oil and shark liver oil, is also known.
Of significant interest are phytosterols/phytostanols, which are contained in rapeseed coconut, soybean oil, seeds, nuts, and coniferous seed oil, which have a mild effect on lipid metabolism.
To reduce the fat/calorie content of the diet, you should use the correct cooking technology (boiling, baking, stewing).
The possibility of using alcohol to influence the lipid profile should be done with caution (assuming that the patient will comply with the recommended dose) - vodka/cognac/whisky at a dose of 45–50 ml/day, table wine (red/white) at a dose of 150 ml per day day.
Can dietary supplements increase cholesterol levels? If you follow the instructions, no, they can’t; at the same time, if they are abused, side effects can develop. For example, long-term use of dietary supplements containing fiber in doses of more than 60 g/day can cause disruption of the absorption of microelements/vitamins.
Menu (Power Mode)
It is necessary to organize 5 meals a day. If you feel hungry in the evening before going to bed, you can eat apples, oranges, carrots or drink kefir. The menu for three days might look like this:
The first day
| Breakfast |
|
| Lunch |
|
| Dinner |
|
| Afternoon snack |
|
| Dinner |
|
Second day
| Breakfast |
|
| Lunch |
|
| Dinner |
|
| Afternoon snack |
|
| Dinner |
|
Day three
| Breakfast |
|
| Lunch |
|
| Dinner |
|
| Afternoon snack |
|
| Dinner |
|
Below is a table of products on the basis of which you can create a varied diet for the whole week.
| Products name | Featured | Prohibited |
| Meat | Turkey, chicken, veal, rabbit, lean beef (twice a week). Poultry without skin; additionally remove fat from meat. | Pork, fatty beef, lamb, duck and goose meat, all sausage products, pates, sausages, sausages, liver, kidneys, brains. |
| Eggs | Up to 3 pieces per week. | Egg yolk. |
| Fats | Unrefined sunflower, corn, olive or soybean oils up to 2.5 tablespoons per day in all dishes. | Margarine, lard, animal fat, palm and coconut oil, butter. |
| Fish | Lean sea fish (hake, blue whiting, pollock, navaga, pollock, haddock) and pike three times a week. | Fatty species: salmon, mackerel, sardine, eel, mackerel, tuna, herring, oysters, caviar, shrimp, processed fish, limited river fish. |
| Dairy | Skim milk or 1% fat, low-fat kefir, natural yogurt, “Grace” or “Fitness” cheeses, 20% low-fat cottage cheese. | Full-fat cottage cheese, cream, sour cream, ice cream, curd mass and glazed sweet cheeses, processed cheeses, condensed milk. |
| Vegetables | All fresh and frozen vegetables, legumes, corn. | French fries and chips. |
| Fruits | All fruits except banana and grapes, dried fruits. | Candied fruits, peanuts, pistachios and hazelnuts. |
| Cereals | Brown rice, oatmeal, durum and whole grain pasta, whole grain bread. | White rice, semolina, limit buckwheat. |
| Bakery | Oatmeal cookies, bread and fitness cookies. | Biscuits, rolls, pastries, cakes, puff pastry products. |
| Sweets | Low-fat puddings, sugar-free jellies, popsicles, frozen juice. | Chocolate, pastry cream, toffee, marmalade, pastille, sugar, syrups, glucose and fructose. |
| Beverages | Juices without sugar, tea, weak coffee, still mineral water. | Cocoa, coffee with cream and milk, alcoholic and sweet carbonated drinks. |
Prevention
The main measures for the primary prevention of hypercholesterolemia include:
- Normalization of weight to the norm corresponding to gender and age.
- Dietary food with a reduced fat content, enriched with fiber/vitamins and a reduction in salt intake to 5 g/day.
- Increasing the level of physical activity (selected individually).
- Refusal/minimization of alcohol intake and avoidance of smoking.
- Limiting overloads in the psycho-emotional sphere.
- Maintain normal blood pressure/blood glucose levels.
- Timely treatment of diseases that contribute to the development of dyslipidemia ( diabetes mellitus , liver, thyroid, kidney diseases).
List of sources
- Diagnosis and treatment of familial hypercholesterolemia (Russian recommendations) / M.V. Ezhov, I.V. Sergienko, T.A. Rozhkova [and others] // Bulletin of modern clinical medicine. - 2021. - T. 10, issue. 2. - P.72-79.
- Bubnova M.G., Kukharchuk V.V. Recommendations of the European Society of Cardiology and the European Society of Atherosclerosis for the diagnosis and treatment of dyslipidemia: main provisions // Cardiology. - 2021. - No. 3. - P. 85-59.
- Practical lipidology with methods of medical genetics: a guide / V.A. Koshechkin, P.P. Malyshev, T.A. Rozhkova. - M.: GEOTAR-Media, 2015. - 112 p.
- Low and very low density lipoproteins: pathogenetic and clinical significance / V.N. Titov, I.A. Vostrov, S.I. Kaba et al. // Clinical medicine. - 2013. - No. 1. - With. 20-27.
- Familial hypercholesterolemia: screening, diagnosis and treatment of children and adult patients: clinical guidelines prepared by the expert group on familial hypercholesterolemia at the National Lipid Association of the USA // Atherosclerosis and dyslipidemia - 2012 - No. 1.
Possible consequences
Among the complications:
- Heart attack. Acute disturbance of coronary blood flow and cardiac nutrition. Accompanied by tissue death.
- Stroke. The process is identical in nature. It is characterized by necrosis of nerve fibers in the brain.
- Vascular dementia.
- Renal dysfunction.
- Liver disorders.
- Permanent asthenic syndrome.
Disturbances in the balance of lipids, the rate and nature of their deposition, storage, and circulation in the bloodstream determine a whole host of diseases. Potentially life-threatening and in most cases “silent”, not manifesting themselves in any way until the moment they become threatening. These include, for example, atherosclerosis.
Hypercholesterolemia is accompanied by pronounced disorders of the cardiac structures and brain, although not immediately.
Changes require mandatory medical intervention. Without the help of doctors there is no chance of spontaneous recovery. Diet and the use of drugs without prescription are not practiced.