You have had heart surgery - either coronary artery stenting, bypass surgery, or both. What does this mean in the grand scheme of things? This means that modern medical technologies have given you a second chance to find a healthy heart, you again have good blood supply to the myocardium, you can again live without heart pain, not be afraid of physical activity, and our goal is to preserve this second chance given to you for a healthy heart!
Despite surgical treatment and improved blood supply to the heart muscle, which should create favorable conditions for the effective restoration of the patients’ quality of life, expectations are not met - their ability to work and social activity continue to remain low. Many experts recognize the insufficient preparedness of outpatient medical institutions for the rehabilitation of cardiovascular patients. According to one of the leading cardiologists in St. Petersburg, after hospitalization such patients often end up in a network of outpatient institutions that are simply not ready to treat them.
If a patient after heart surgery does not take care of his health and does not visit a cardiologist, then a very high percentage of such patients end up on the operating table again after a few years, because heart disease is chronic and requires constant prevention of relapse!
For example, for 2010-2012 cardiovascular mortality among men 35-74 years old in Germany, Great Britain, Sweden, Belgium, Austria, Italy, Denmark and many other European countries was 100-200 people per 100,000 population. In Russia there are more than 1000 people (Circulation, Heart Disease and Stroke Statistics, 2015), which emphasizes the need for rehabilitation and secondary prevention in cardiac patients.
What is rehabilitation and how should it be carried out?
Rehabilitation - “rehabilis” - lat. restoration of ability.
Who is suitable for cardiac rehabilitation?
- patients with myocardial infarction
- after operations CABG, MCS
- after stenting
- after valve replacement
- after surgical treatment of arrhythmias
Rehabilitation after heart surgery is a set of medical and psychological measures aimed at:
- prevention of further development of the disease
- disability prevention
- improving quality of life
- maintaining the patient's ability to work
- returning him to social activity
Rehabilitation assistance is provided:
- regardless of the duration of the disease
- subject to the stability of the patient’s clinical condition
- in the presence of rehabilitation potential, i.e. physical, psychological, social resources of a person that will help him regain strength
- in the absence of contraindications to various techniques
- based on established diagnosis
Research and specialist consultations required to perform cardiac surgery
Coronary artery bypass grafting
- Coronary angiography, ventriculography (if necessary)
- Transthoracic echocardiography
- Treadmill test
- ECG
- Laboratory research methods
- X-ray of the chest organs
- External respiration function
- Doppler examination of brachiocephalic vessels
Heart valve surgery
- Transthoracic echocardiography
- Transesophageal echocardiography
- Coronary angiography
- ECG
- Laboratory research methods
- X-ray of the chest organs
- External respiration function
- Doppler examination of brachiocephalic vessels
- Consultation with an ENT doctor
- Dentist consultation
In complicated cases, other examinations may be needed, for example, radionuclide scintigraphy of the myocardium, computed tomography of the brain, computed tomography of the lungs, nuclear magnetic resonance, etc.
Stages of cardiac rehabilitation
There are three stages of rehabilitation after heart surgery and myocardial infarction:
- Stage I – hospital, where stenting/bypass surgery is performed according to indications
- Stage II – sanatorium-resort treatment
- Stage III – outpatient follow-up of the patient after heart surgery or heart attack
is especially important, since it is the longest in time, and, ultimately, determines the further development of the disease.
And if everything is clear with the first and second stages of rehabilitation - a hospital, where the patient is taken by ambulance, and, if possible, a sanatorium, then the third stage of rehabilitation, outpatient, the most important for maintaining health in the future, remains at the patient’s choice.
At the EXPERT Clinic you will be able to undergo the third stage of rehabilitation under the supervision of experienced specialists. In rehabilitation, a multidisciplinary approach is always used, i.e. interaction of specialists of various profiles, namely:
- cardiologist-rehabilitologist
- neurologist
- psychotherapist
- nutritionist
This provides various types of assistance to overcome the consequences of the disease, change lifestyle, reduce the impact of risk factors; assessment of the need and sufficiency, duration, consistency and effectiveness of the participation of each specialist at each specific point in time during the rehabilitation period.
If necessary, at the EXPERT Clinic you will be advised by a council of doctors of various profiles.
Third (outpatient) stage
The “Third Stage of Cardiac Rehabilitation” program at the EXPERT Clinic includes:
- appointment with a cardiologist
- Patient School – group classes with a cardiologist, which discusses the problems patients face and their solutions
- performing ECG, Echo-CG, 24-hour ECG and blood pressure monitoring according to indications
- general blood test, biochemical blood test (lipidogram, coagulogram, electrolytes, homocysteine, CRP, etc.)
- psychological testing
- consultation with a psychotherapist
- consultation with a neurologist
- nutritionist consultation
- genetic analysis of all cardiac markers, including the risk of sudden death, for the patient and his relatives
- genetic analysis of drug doses in the treatment of cardiovascular diseases
Methods for diagnosing heart defects
In order to establish a diagnosis of heart disease, an anamnesis is collected, the presence of diseases that could lead to deformation of the heart valve is revealed: rheumatic diseases, infectious, inflammatory processes, autoimmune diseases, injuries.
- The patient must be examined to identify the presence of shortness of breath, cyanosis, edema, and pulsation of peripheral veins. Using percussion, the boundaries of the heart are identified and sounds and murmurs in the heart are listened to. The size of the liver and spleen is determined.
- The main method for diagnosing valve pathology is echocardiography
, which allows you to identify the defect, determine the area of the opening between the atrium and the ventricle, the size of the valves, cardiac fraction, pressure in the pulmonary artery.
More accurate information about the condition of the valves can be obtained by performing transesophageal echocardiography. - Electrocardiography is also used in diagnostics, which allows one to assess the presence of atrial and ventricular hypertrophy and identify signs of overload of the heart. Daily Holter ECG monitoring allows you to identify rhythm and conduction disturbances.
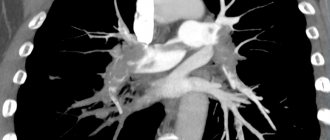
- Highly informative methods for diagnosing heart defects are cardiac MRI or cardiac MSCT. Computed tomography scans provide precise and numerous sections, which can be used to accurately diagnose the defect and its type.
- Laboratory tests play an important role in diagnosis, including urine and blood tests, determination of blood sugar, cholesterol levels, and rheumatoid tests. Laboratory tests allow us to identify the cause of the disease, which plays an important role in subsequent treatment and patient behavior.
Cardiac rehabilitation results
The positive effects of cardiac rehabilitation at the EXPERT Clinic include:
- eliminating risk factors for coronary heart disease and reducing risk in general
- increasing physical activity
- smoking cessation
- normalization of blood pressure numbers
- weight loss
- improvement of lipid profile
- improving carbohydrate metabolism
- improvement of endothelial function
- slowing down the development of atherosclerosis and its clinical consequences
- improvement of psychophysical condition
- mobilization of patients to cooperate in the process of cardiac rehabilitation.
Dynamic (dispensary) observation is the main form of support for patients with chronic diseases in an outpatient setting. And this does not mean monitoring the natural development of the disease, as, unfortunately, often happens, but carrying out a set of secondary prevention and rehabilitation measures!
After surgical treatment, the patient is recommended to visit a cardiologist in the first days after discharge!
During the first year, visits to the doctor should be made every 4 months. Further, it is recommended to visit a cardiologist at least 2 times a year.
The goal of rehabilitation after cardiovascular accidents is to restore the patient’s physical and psychological health. Rehabilitation is indicated for all patients after surgery, regardless of the severity of the condition, both to gain self-confidence and strength, and to minimize the risk of re-exacerbation. Therefore, do not neglect your health and do not allow the disease to develop! Then you will get a chance to extend your life and improve its quality.
Other recommendations
There are a few other mandatory tips that patients undergoing valve replacement surgery must follow.
- If you experience symptoms of cardiac problems (chest pain, a feeling of interruptions in the heart), signs of circulatory problems (swelling in the legs, shortness of breath) and other unexpected symptoms, you should immediately consult a doctor.
- Patients who have had a biological valve installed are not recommended to take calcium supplements. In their diet, it is advisable for them not to overuse products containing it: milk and dairy products, sesame seeds, nuts (almonds, Brazilian), sunflower seeds, soy.
- All doctors, including the dentist, need to warn the patient that he has an artificial valve installed.
Following the necessary recommendations will help the patient maintain excellent health for a long time and live a full life.
FAQ
How long does rehabilitation take after heart surgery?
How long it will take to restore body functions depends on several factors: the severity of the initial condition, age, and motivation of the patient.
However, it is necessary to understand that, in fact, rehabilitation lasts for life, because the whole range of measures is aimed not only at restoring physical and psychological strength, but also at preventing repeated exacerbations of the situation. Without constant prevention, diseases of the cardiovascular system most often worsen.
How to help yourself with heart pain? What medications should you carry with you at all times?
If an attack of angina occurs (pain or burning behind the sternum, shortness of breath during physical and emotional stress, attacks last several minutes), then it is necessary:
- stop physical activity, sit down, calm down
- use nitroglycerin in the form of a spray (Isoket, Nitromint-spray), two or three doses under the tongue
- if the pain does not stop, then after 3-5 minutes you should repeat taking the drug
- If the pain does not go away within 15 minutes, you should chew 1 aspirin tablet with water and call an ambulance.
At what level should blood pressure numbers be maintained?
It is necessary to maintain blood pressure at a level less than 130/80 mmHg. High blood pressure – more than 140/90 mmHg. Art. - indicates the presence of hypertension. More than 180/110 mmHg. Art. indicates severe hypertension.
In order not to lose control of your blood pressure, you must take the medications prescribed by your doctor on time! For this:
- use alarm clock, beep on phone to remind
- Keep the tablets near your toothbrush, razor, or other items you use daily
- Place the tablets in jars indicating the time of administration; for this, you can purchase a special box with compartments at the pharmacy.
What physical activities are possible?
The amount of physical activity can be increased gradually.
6 weeks after surgery , moderate exercise is possible, such as vacuuming, walking the dog, morning exercises, hiking and fishing.
After 3 months, you can increase your activity - swimming, cycling, bowling, tennis, football. Snow removal or gardening at the dacha is allowed.
To maintain good health, moderate-intensity outdoor exercise for 30 minutes 3 times a week is recommended, and those patients who lead a sedentary lifestyle should begin with light exercise programs.
to sexual activity after 9-14 weeks. An exercise test must be performed under the supervision of a physician. If the doctor does not detect any symptoms of overload, then sexual activity is permitted.
How to eat properly if you have heart and vascular diseases?
The main goal of dietary nutrition is to reduce the level of atherogenic lipids in the blood to stop the development of atherosclerosis. Recommended levels of total cholesterol after heart surgery are less than 4.0 mmol/l, LDL - less than 1.8 mmol/l, TG less than 1.7 mmol/l, HDL for women more than 1.2; for men more than 1.0 mmol/l.
It is recommended to eat fruits and vegetables every day, sometimes lean meat, fish, olive and other oils. We allow alcohol in a dose of no more than 2 glasses of red wine per day for men, 1 glass for women. A nutritionist will help you create a detailed nutrition program.
Introduction
Despite a well-developed surgical technique for cardiac injuries, the level of postoperative complications remains very high, reaching 57% [2]. The purpose of this study is to systematize complications of wounds of the heart and pericardium using large statistical material,
accumulated in one medical institution, identifying the most significant factors contributing to the development of complications and determining measures to prevent complications.
Material and methods
With wounds of the heart and pericardium at the Research Institute of Emergency Medicine named after. N.V. Sklifosovsky from 1980 to 2010, 936 victims were admitted: with cardiac injuries - 760 (81.2%), with isolated pericardial injuries - 176 (18.8%). The average age of the victims was 35.6±10.6 years. There were 90.7% men, 9.3% women.
The main mechanism of injury was stab wounds with cold weapons (97.8%), gunshot wounds occurred in 2.2% of victims. 23.5% of patients were injured as a result of a suicide attempt, 48.8% were under the influence of alcohol or drugs. Combined wounds of the chest and abdomen were present in 235 (25.1%) patients. 97 (10.4%) patients died during surgery (90 with cardiac injuries, 7 with pericardial injuries). An analysis of complications was carried out in 839 patients who underwent surgery. Statistical processing was carried out to evaluate groups of patients according to the ISS, RTS, TRISS scales, age, volume of blood loss, and time from the moment of injury to surgery. The postoperative period proceeded without complications in 537 wounded, which was 64.0%. The remaining 302 (36.0%) victims had from 1 to 8 complications within a period of 2 to 79 days.
To compare the results of prevention and treatment of complications, two periods were identified: 1980-1995. (267 patients) and 1996-2010. (572 patients). Both groups are comparable in terms of main baseline indicators (Table 1).
In the postoperative period, to assess the condition of the heart and pericardium and timely diagnosis of complications, all victims underwent a dynamic instrumental examination, including electrocardiography, chest radiography and two-dimensional ultrasound (EchoCG and ultrasound of the pleural cavities). In the presence of ultrasound signs of valve and septal defects, ventriculography was performed; in the case of coronary vessel injury and myocardial infarction, coronary angiography was performed.
Results and discussion
Analysis of basic statistical data showed that the likelihood of developing complications was determined by the age of the patients, the amount of blood loss, the severity of the injuries, and the condition of the victim at the time of admission (Table 2).
For convenience of presentation and analysis, we used a classification by organs and systems, separating purulent-septic complications and postoperative bleeding into separate groups (Table 3).
Cardiopericardial complications were most frequently observed.
Myocardial infarction (MI) was diagnosed in 24 (2.9%) patients. The most common cause of its development was certain damage to the coronary vessels (Table 4).
According to the literature, injuries to the coronary arteries (CA) occur in 2.8-8.0% of cases [3, 4]. In case of damage to vessels in the proximal part, restoration of the integrity of the vessel or bypass is considered optimal, while in case of distal damage, one can limit ourselves to suturing and ligation of the vessels [7, 8, 10].
Numerous manuals on the surgery of cardiac wounds describe in detail the technique of suturing wounds of the heart located in close proximity to the coronary vessels, however, in 8 victims who underwent surgery, when multiple sutures were applied to the wound of the heart, the anterior interventricular branch (LAD) of the left was caught in the suture CA, poorly visualized in fatty tissue. Subsequently, 7 of them developed MI, which was the cause of death in 1 case.
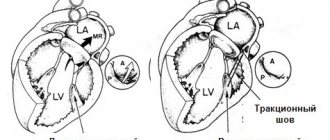
In 2 young patients (29 and 36 years old), the development of MI (taking into account coronary angiography data) was associated with stenosis of the LAD as a result of vessel involvement in the scar in the area of suturing the cardiac wound. Unlike MI that developed due to coronary heart disease, with MI due to involvement of the coronary artery in a suture or scar, dilatation and stenting of the vessel are technically impossible. Both patients underwent delayed coronary artery bypass grafting several months after discharge.
It should be emphasized that in 4 elderly wounded patients, MI developed in the absence of damage to the coronary vessels. 3 of them had severe coronary sclerosis, diagnosed in 2 by pathological examination and in 1 by coronary angiography. In one victim, the infarction was actually an area of myocardial contusion due to a gunshot wound.
In 6 victims who suffered an MI, a cardiac aneurysm formed. In total, 2 people died with a cardiac aneurysm, one of them from its rupture. One of these patients underwent surgery: on the 3rd day after suturing the heart wound, he underwent myocardial revascularization by mammary coronary bypass (with the LAD distal to the site of injury), and 8 months later - resection of the aneurysm and plastic surgery of the left ventricular wall. The remaining 3 patients were discharged after stabilization of their condition; their further fate could not be traced.
Trauma to intracardiac structures (IC) when the heart is wounded sharply aggravates the condition of the victims; most of these wounded die at the scene of the incident and on the operating table. These injuries are usually detected during postmortem examination [3], while the frequency of injuries detected in the hospital ranges from 1 to 4% [1, 5]. Perhaps such injuries occur more often, but remain undiagnosed in some surviving patients. Currently, surgical treatment in two stages is considered optimal, with the best results observed after operations performed within 2-3 months after injury [5]. In case of significant hemodynamic disturbances, primary repair is suggested [7].
In our observations, only 2 (0.2%) patients were diagnosed with a ventricular septal defect in the postoperative period; both of them were successfully operated on. In 18 of the deceased, VC injuries were detected only at autopsy, 10 of them died during surgery, the rest within 1 hour to 10 days after surgery.
Persistent heart rhythm disturbances were observed in 3 (0.4%) victims. They were caused by damage to the conduction system of the heart due to injury to the high parts of the interventricular septum, injury to the interatrial septum, and injury to the left ventricle posteriorly in the projection of the sinoatrial node.
Foreign bodies of the heart and pericardium were observed in 2 (0.1%) victims admitted in a stable condition after suicide attempts. They were operated on in a delayed manner after additional examination and clarification of the localization of foreign bodies: a sewing needle in one observation, a piece of glass in another.
A rare complication of cardiac injuries is vascular embolism from foreign bodies trapped in the chambers of the heart [9]. We have one such observation: in a 34-year-old patient with a gunshot wound to the left ventricle of the heart, no foreign body was found during thoracotomy, but on the 8th day after the operation an embolism of the right femoral artery occurred with a bullet. An arteriotomy was performed and the foreign body was removed.
The most common postoperative complication is pericarditis, the clinical and instrumental signs of which are Yu.L. Shevchenko, A.D. Kucherenko was noted in 33.3% of the wounded [6]. We observed pericarditis in 146 (17.4%) patients.
The main predisposing factors for the development of pericarditis: exposure for more than 8 hours from the moment of injury to surgery due to late admission or late diagnosis - 10 (6.8%) cases, technical difficulties when suturing a cardiac wound - 6 (4.1%), open cardiac massage - 4 (2.7%), inadequate drainage of the pericardial cavity after pericardiotomy - 49 (33.6%), inadequate drug prevention - 36 (24.7%) cases. In addition, pericarditis developed in 8 wounded patients who, due to postoperative bleeding, underwent rethoracotomy with repeated revision of the heart (5.5%), as well as in 10 victims with thoracoabdominal and abdominal-thoracic wounds with damage to hollow organs (6.8%).
Isolated pericarditis was observed in 72 (49.3%) of the wounded, 74 (50.7%) of the victims had a combination of pericarditis in various combinations with other complications that could play a role in its development. Most often, pericarditis was combined with pneumonia (35), pleurisy (27), and MI (9).
The timing of the onset of pericarditis varied depending on the leading etiological factors and ranged from 1 to 48 days. Early (from 1-3 days) appearance of effusion in the pericardium was observed in the absence of adequate drainage. Primary isolated pericarditis developed by 4-9 days. Later development of pericarditis was associated with other purulent-septic complications.
Serous-fibrinous pericarditis is most often observed after pericardiotomy (112), serous pericarditis was diagnosed in 27 wounded, purulent pericarditis developed in 7 patients in the presence of other severe purulent-septic complications. To prevent pericarditis, we perform thorough sanitation of the pericardial cavity, before suturing the pericardiotomy incision, we form a window on the posterior wall of the pericardium with a diameter of at least 2-2.5 cm, and in the postoperative period for 5-7 days we carry out drug prevention of pericarditis with non-steroidal anti-inflammatory drugs under the cover of gastric blockers secretion with regular ultrasound monitoring. This made it possible to reduce the incidence of postoperative pericarditis from 27.1 to 13.9%.
Treatment of pericarditis consisted of a course of anti-inflammatory therapy with non-steroidal drugs, if ineffective - with corticosteroids, while other complications were also eliminated. Puncture and drainage of the pericardium were performed in 4 cases; in another 1 case, subxiphoid pericardiotomy was performed with subsequent drainage of the pericardium. The indication for drainage in 3 patients was the progression of hydropericardium, and in 2 patients it was the development of purulent pericarditis. One patient experienced progression of the process with the formation of constrictive pericarditis, which required surgical treatment.
Pulmonary-pleural complications
are not specific for cardiac injuries and in a certain percentage of cases are observed after thoracotomy for any penetrating chest wounds.
Postoperative pneumonia developed in 88 (10.5%) patients. In most cases, pneumonia was observed on the side of the thoracotomy, only in 2 cases - on the contralateral side, and in 26 cases it was bilateral. In 82 victims, hypostatic segmental lower lobe pneumonia developed, in 6 deaths - subtotal and total pneumonia in the presence of other complications.
The likelihood of developing this complication was significantly higher in cases of suicidal and auto-aggressive actions (43), in patients who suffered alcoholic delirium (13) and prolonged (over 10 hours) artificial ventilation (16) in the postoperative period, as well as in the presence of combined penetrating chest wounds and abdomen (17). 32 victims had lung wounds; these were superficial wounds of the peripheral parts, which did not affect the development of pneumonia, with the exception of 3 wounded with deep wounds with the formation of intrapulmonary hematoma and hemoaspiration.
Predisposing factors for the development of pneumonia were hypoventilation of lung segments (48 observations), venous congestion (31), segmental and lobar atelectasis (30), intrapulmonary hematomas (3). X-ray signs of pneumonia in most patients (44.4%) appeared on days 4-6 after surgery, in 17.7% on days 1-3, in 14.4% on days 7-9 . In 5 victims, pneumonia was detected at autopsy within 2 to 8 days after surgery.
Prevention of pneumonia was aimed primarily at preventing hypoventilation. Treatment of pneumonia was carried out according to the generally accepted scheme: antibacterial therapy with the use of broad-spectrum antibiotics, mucolytics, inhalations, exercise therapy, and for persistent atelectasis - sanitary fibrobronchoscopy.
Pleurisy was observed in 68 (8.1%) victims. It was manifested by the constant accumulation of aseptic exudate in the pleural cavity for a long time. Predisposing factors for the development of pleurisy were mediastinal hematoma due to parasternal wounds (28), lung injury (25), pneumonia (14), coagulated hemothorax (5), and long-term pneumothorax (5). Treatment of pleurisy in most cases consisted of repeated pleural punctures under ultrasound guidance and a course of therapy with non-steroidal anti-inflammatory drugs.
Purulent-septic complications
were observed in 13.0% of victims.
Pleural empyema was diagnosed in 21 (2.5%) patients, including 6 who died, within 6 to 15 days after surgery. In 7 patients it was localized in the anterior parts of the pleural cavity and was limited, associated with a suppurating thoracotomy wound. The development of pleural empyema was promoted by parasternal localization of wounds with subsequent suppuration (10 observations), massive blood loss (6), injury to hollow organs due to thoracoabdominal wounds (3), rethoracotomy (3), and prolonged pneumothorax (2).
Mediastinitis developed in 4 (0.5%) wounded, 2 of them died. 3 victims had parasternal wounds with damage to the internal thoracic vessels and mediastinal hematoma, another 1 had multiple wounds to the neck, chest, and abdomen with damage to hollow and parenchymal organs.
Treatment of pleural empyema and mediastinitis consisted of drainage of the pleural cavity and mediastinum with TMMK-24 tubes, followed by constant lavage with aspiration, and complex antibacterial and immunocorrective therapy.
Suppuration of the thoracotomy wound occurred in 69 (8.2%) patients. In most cases (40), wound suppuration developed in parasternal wounds, which is explained by damage to the cartilaginous parts of the ribs and the difficulty of hermetically suturing the medial angle of the thoracotomy wound. When the wound is localized in this area with a known infection of the wound channel, additional conditions are created for suppuration, which was observed in 25 patients after suicide attempts and in the presence of multiple chest wounds, regardless of their location.
Rare complications of cardiac injuries are sepsis and osteomyelitis of the ribs and sternum.
Sepsis was diagnosed in 5 (0.6%) victims in the presence of other complications (pneumonia - 5, pericarditis - 4, pleural empyema - 3, wound suppuration - 2, septic thrombophlebitis - 2). Three patients died. The most significant factor in the development of sepsis was blood loss in combination with infection of the chest wall, pleural cavity and pericardial cavity with prolonged exposure from the moment of injury and multiple wounds.
Chronic osteomyelitis of the ribs and sternum developed in 2 (0.2%) patients in the presence of suppuration of the thoracotomy wound and pleural empyema. After sanitation of the wound and pleural cavity, both patients underwent radical surgery 2 months after receiving the injury.
Vascular complications
noted in 8 (1.0%) victims. These were complications associated with thrombosis of large veins (superior vena cava - 2, brachiocephalic vein - 1) and deep veins of the lower extremities (4), in 3 cases there was, in addition, thromboembolism of the branches of the pulmonary artery. In all these observations, the course of the postoperative period was accompanied by the development of severe purulent-septic complications due to massive blood loss. 6 victims died, including a 75-year-old patient, whose cause of death was a rupture of a previously diagnosed abdominal aortic aneurysm.
Abdominal complications
developed in 13 (1.5%) patients, 8 of them with combined wounds of the chest and abdomen. These were adhesive intestinal obstruction (3), acute pancreatitis (2), gastrointestinal bleeding from acute and chronic ulcers (3), peritonitis (2), as well as biliohematoma, intestinal fistula, and volvulus of the small intestine. In one patient with an injury to the interventricular septum, the course of the postoperative period due to hemodynamic disorders was complicated by the development of a non-occlusive disorder of the mesenteric circulation with necrosis of the small and large intestine, leading to death.
Neurological complications
were in 7 (0.8%) wounded: acute cerebrovascular accident due to hemodynamic disorders and coagulopathy - in 5 patients with cerebral atherosclerosis, meningoencephalitis - in 1 patient with simultaneous penetrating injury to the skull, cerebral edema and ischemia - in 1 patient .
Postoperative bleeding
observed in 32 (3.8%) patients. In 18 wounded, the source of bleeding was small vessels of the chest wall as a result of insufficient hemostasis against the background of hypotension and coagulation disorders due to massive blood loss.
In 2 victims, a wound to the aorta was missed, in another 1, a cardiac wound was not found during inspection, in 7 cases bleeding was noted from a sutured myocardial wound due to the cutting of sutures, in another 1 case there was bleeding from a missed second wound due to a through wound of the heart, in 3 cases - from a wound pericardium.
For postoperative bleeding, rethoracotomy was performed in 21 cases; 13 out of 32 patients died. In surviving patients, bleeding after surgery was the cause of the development of complications such as coagulated hemothorax (9), pleurisy (8), and pleural empyema (4).
Thus, the main objective factors contributing to the development of complications after cardiac injuries are the volume of blood loss, the age of the victims, the severity of associated injuries, the patient’s condition at the time of admission, long periods from the moment of injury to surgery, as well as technical errors during surgery. Features of postoperative management and early diagnosis of complications are of great importance. To identify complications, all patients in the postoperative period need to undergo a comprehensive instrumental examination over time. Studying the causes of various types of complications made it possible to develop appropriate preventive measures and reduce the frequency of complications over the past 15 years from 43.8 to 32.3%, and postoperative mortality from 13.8 to 6.8%.
Indications for coronary artery bypass grafting
Indications for CABG are determined by varying degrees of arterial damage and manifestations of coronary heart disease:
As a rule, CABG is not performed:
- severe multiple organ failure;
- during the first months after cerebrovascular accident;
- malignant neoplasms.
Heart transplantation. Implantation of circulatory support devices.
At the present stage of medical development, the possibilities for treating patients with end-stage heart failure are almost limitless. Heart transplantation, when a donor organ is implanted in place of a muscle sac that has exhausted its functional reserves, has already been mastered and has become a routine method of surgical treatment. With the advent of new materials and modern techniques, methods of artificial assisted circulation, including the artificial heart, are being actively developed.