To the Telemedicine Department of the Scientific Center for Cardiovascular Surgery named after. A.N. Bakulev received a discharge from patient K., 58 years old from Izhevsk, with a diagnosis of:
Atherosclerosis of the aorta, aortic valve; critical aortic stenosis (maximum gradient - 100 mmHg) with 2nd degree regurgitation; calcification 2-3 degrees; relative mitral valve insufficiency of 1-2 degrees, tricuspid valve insufficiency of 1 degree; atriomegaly; pulmonary hypertension; expansion of the ascending aorta; permanent form of atrial fibrillation (normotachysystolic form); history of syncope; chronic heart failure degree 2a, functional class 3; cardiac ischemia; stable angina pectoris grade 3-2; hypertension stage 3, degree 3, risk 4; encephalopathy of mixed origin, moderate vestibulopathy, cephalgic syndrome; cholelithiasis; chronic calculous cholecystitis, remission stage.
Residential survey
Upon admission to the hospital, the patient complained of general weakness; fatigue; shortness of breath when walking at a calm pace after 300 meters, when climbing two floors of stairs; discomfort and heaviness behind the sternum, which arise in the morning and go away on their own after 10-15 minutes; interruptions in heart function; pulsation in the head; swelling in the legs in the evening.
The heart defect was first discovered at the age of 50; general weakness and shortness of breath were a concern. The woman was seen by a rheumatologist and refused the proposed surgical treatment. Regularly underwent inpatient treatment.
The real deterioration began at the age of 57 years in the form of the development of heart rhythm disturbances (atrial fibrillation) after exercise. Hospitalized at the local hospital for examination and treatment.
From an objective examination
The general condition is satisfactory, the skin is pale, peripheral lymph nodes and the thyroid gland are not enlarged. Breathing in the lungs is vesicular, with a hard tint in the lower sections. The respiratory rate is 18 per minute. The heart area is not changed. Apex impulse in the 5th intercostal space. The heart sounds are arrhythmic, weakened at the apex, there is a systolic murmur in the aorta with conduction to the neck with a weakened second sound. Heart rate (HR) is irregular, 64 beats/min, blood pressure (BP) = 130/80 mm. Hg Art. The abdomen on palpation is soft, painless, and increased in volume. Liver - along the edge of the costal arch. There is no swelling.
Instrumental studies
Echocardiography (EchoCG):
According to an echocardiographic study, a diagnosis was made: critical aortic stenosis; aortic valve calcification grade 2-3; aortic valve insufficiency of 2-3 degrees; left atrium dilatation; concentric hypertrophy of the left ventricle; mitral valve insufficiency grade 2; tricuspid valve insufficiency 1st degree; global contractility of the left ventricle is preserved; signs of moderate pulmonary hypertension; atherosclerosis of the aorta; the ascending aorta is expanded.
X-ray of the chest organs
Aortic heart disease: aortic stenosis plus aortic valve insufficiency. Moderate central venous stasis. The ascending aorta and aortic arch are dilated. Peribronchial fibrosis.
Holter monitoring
Atrial fibrillation with heart rate 43-177 beats/min with maximum asystole 2480 MSK. Single ventricular extrasystole.
Ultrasound examination of the abdominal organs:
Cholelithiasis. Gallbladder calculus. Fatty infiltration of the liver. Pancreatic steatosis.
To resolve the issue of further treatment tactics and the possibility of surgical treatment, documents were sent to the Scientific Center for Surgery named after. A. N. Bakulev for a telemedicine consultation.
1.Heart valve replacement
Heart Valve Replacement
– currently this is a very effective procedure with a low risk of complications. It is indicated for patients with symptoms of aortic valve stenosis. For some patients, refusing this advanced surgical technology means a significant reduction in life expectancy or the risk of sudden death. If there are no obvious contraindications to surgery (for example, coronary heart disease, previous heart attack), then this operation is usually prescribed and recommended for all patients with a degree of stenosis above average. With severe symptoms (chest pain, fainting, breathing problems), the life expectancy of many patients without heart surgery does not exceed 5 years, since the disease progresses over time.
Heart valve replacement surgery can be performed using an open procedure.
or
minimally invasive.
Although this is a rather complex procedure, extensive experience with such surgical treatment has now significantly reduced the possible risks. All stages are worked out to the smallest detail. During valve replacement, the possibility of complications and emergency situations is taken into account, therefore the operating room and medical staff are prepared taking into account the different developments of the situation during the operation.
Heart valve replacement occurs in eight stages.
Before this, the patient undergoes
preparation for the operation
(outpatient or in a hospital), following certain instructions and taking a number of medications. In some cases, it is necessary, on the contrary, to discontinue regularly taken medications.
A must read! Help with treatment and hospitalization!
Publications in the media
MECHANICAL PROSTHETICS
• Types of mechanical prostheses •• Ball (not currently used): Magovern-Cromie, Smeloff-Cutter, Cross-Jones, AKCh, MKCH •• Disc: Bjork-Shiley, Sorin Monocast, Medtronic-Hall, Lillehei-Kaster, Omniscience , Bicer, MIX, LIX •• Bivalve: St. Jude Medical, Sorin Bi Carbon, Carbomedics, ATS, Duromedics, MedEng.
• Advantage •• Durability—averaging over 30 years (excluding cases of prosthetic infective endocarditis [IE]) •• Exceptions include obturator strut failure in some Bjork–Shiley valve models.
• Disadvantages •• Thrombogenicity (the least with the St. Jude Medical valve) •• The need for constant anticoagulant therapy •• Relative stenosis in disc and ball prostheses •• Post-prosthetic aneurysms in disc prostheses with a small opening angle of the obturator element.
• Anticoagulant therapy •• Begin 2 days after surgery, despite therapy with indirect anticoagulants (INR 3.0–4.5) •• The risk of thromboembolism is high (0.2% of fatal and 2% of non-fatal complications per year) •• Thrombosis after mitral valve replacement occurs much more often due to aortic valve replacement •• Ambiguous attitude towards mechanical valves in the tricuspid position (as a rule, St. Jude Medical prostheses are used) is caused by frequent thrombus formation in the right side of the heart ••• Such thrombus formation is due to apparently a low concentration of PgI2, which has an antithrombotic effect. This Pg is synthesized in the lungs and enters the bloodstream into the left side of the heart •• If thromboembolism caused by the presence of a prosthesis has occurred at least once, then the risk of repeated embolisms is increased •• Constant anticoagulant therapy, even with a moderate increase in INR (up to 3.0) , significantly increases the risk of bleeding.
BIOLOGICAL XENOPROSTHESES (Hancock, Carpentier-Edwards, KemKor) and allografts . In terms of hemodynamic characteristics, both valves are comparable to low-profile mechanical prostheses (bicuspid and disc).
• Advantages •• Thrombogenicity is significantly lower than that of mechanical prostheses •• Anticoagulant therapy is necessary only for 2–3 months after surgery (until endothelialization of the sewing ring occurs).
• Disadvantages •• Short life due to degenerative changes and IE, usually appearing 4-5 years after surgery and further progressing •• Probability of dysfunction 10 years after surgery - 20%, after 15 years - 50% •• Durability of allografts is slightly higher; than other biological prostheses.
• Factors influencing longevity •• Patient age—the likelihood of graft dysfunction is inversely proportional to age at the time of surgery •• Position—the likelihood of graft dysfunction in the mitral position is lower than in the aortic position •• CRF and hypercalcemia in hyperparathyroidism—increases the risk of dysfunction and the rate of its progression •• Pregnancy—shortened service life due to greater hemodynamic load (volume).
Prosthesis selection • Mechanical prostheses •• Aortic position or the need for simultaneous mitral and aortic valve replacement •• IE or prosthesis reimplantation due to IE •• Hypercalcemia •• Renal failure • Biological prostheses •• High risk of thrombosis (see below) •• Contraindications to anticoagulant therapy (hemorrhagic diathesis, repeated gastrointestinal bleeding, alcoholism, unwillingness or inability to follow the treatment regimen), planned pregnancy, age over 65-70 years, TC replacement (even with simultaneous implantation of a mechanical prosthesis in the mitral or aortic position).
Complications • Relative stenosis of the prosthesis (acceptable pressure gradients on the prostheses are indicated in the technical documentation for them) • Obstruction of the prosthesis due to thrombosis, fibrosis, proliferation of vegetations • Valvular (thrombosis of the prosthesis or vegetation) or perivalvular (ring abscess, prosthesis separation) regurgitation • IE • • Prosthetic IE ••• Prevalence - 1–4% per year ••• Early (before 90 days after surgery) and late infective endocarditis can be caused by different pathogens ••• IE is distinguished by its clinical course and complications ••• With infection In mechanical prostheses, damage to the valve itself rarely occurs, but there is a tendency for the biological material covering the sewing ring to be involved in the process. ••• When a biological prosthesis becomes infected, damage to both the leaflets and the valve ring occurs. Vegetations may not be visualized by echocardiography ••• Regurgitation occurs due to destruction or perforation of the leaflets of a biological prosthesis, a mechanical obstruction to the normal movement of a ball or disk created by vegetations •••• Perivalvular regurgitation occurs due to abscess of the valve ring and failure of the sutures ••• Valve obstruction occurs more often due to massive vegetations (caused by fungi, Haemophilus parainfluenzae) •••• Obstruction of a biological prosthesis by vegetations more often occurs in the mitral than in the aortic position ••• Infection of prostheses is relatively difficult to respond to antibiotic therapy, most often re-prosthetics is necessary ••• Treatment of IE - see Infectious endocarditis.
Assessing the condition of the prostheses • On auscultation, opening (usually quieter) and closing clicks (usually louder) of mechanical prostheses are heard; their disappearance or decrease in intensity is a sign of thrombosis • A gentle mesosystolic murmur can be heard over disc prostheses • Biological prostheses do not give a specific auscultatory picture • X-ray examination is currently practically not used specifically to study the condition of prostheses • With EchoCG, the type of prosthesis is determined, the diameter and amplitude are measured opening of the obturator element of the mechanical prosthesis, measure the pressure gradient on the prosthesis and diagnose the presence of pathological flows, vegetations, thrombosis, fibrosis • Transesophageal echocardiography to visualize blood clots and vegetations is carried out if prosthetic dysfunction is suspected or in case of atrial fibrillation/flutter • Invasive diagnostic methods are indicated only in case of difficulties in diagnostics.
Anticoagulant therapy • For non-cardiac operations that are fraught with large blood loss, anticoagulants are discontinued 2-4 days before the intervention, INR is determined once every 2 days • One day before surgery (or earlier, if the INR decreases significantly), heparin is started intravenously • For several hours before surgery, heparin is discontinued • After heparin is discontinued, low molecular weight dextran is prescribed, its infusion is continued in the postoperative period until therapy with heparin and warfarin is resumed • Therapy with heparin and indirect anticoagulants is resumed 1–2 days after surgery.
DOSAGE RECOMMENDATIONS FOR INDIRECT ANTICOAGULANTS FOR ANTITHROMBOTIC THERAPY in patients with prosthetic heart valves.
• Indications •• The first 3 months after implantation - warfarin, MHO=2.5–3.5 •• More than 3 months after implantation ••• Mechanical valves •••• Aortic implantation without risk factors: bicuspid valves (warfarin, MHO= 2.0–3.0); disc valves (warfarin, IHO=2.5–3.5); aortic implantation in combination with risk factors (warfarin, MHO=2.5–3.5) •••• Mitral implantation (warfarin, MHO=2.5–3.5) ••• Biological valves •••• Aortic implantation without risk factors (acetylsalicylic acid 80–100 mg/day) •••• Aortic implantation in combination with risk factors (warfarin, MHO=2.0–3.0) •••• Mitral implantation without risk factors (acetylsalicylic acid 80–100 mg/day) •••• Mitral implantation in combination with risk factors (warfarin, MHO=2.5–3.5) ••• Simultaneous coronary bypass surgery - addition of acetylsalicylic acid 80–100 mg/day •• • Warfarin, MHO=3.5-4.5 in high-risk patients when acetylsalicylic acid cannot be prescribed.
• If a thromboembolic episode occurs in a patient on adequate anticoagulant therapy, the dosage of drugs should be adjusted according to the following scheme •• Warfarin, MHO=2.0–3.0 - the dose of warfarin is increased until MHO=2.5–3.5 is reached •• Warfarin , MHO=2.5-3.5 - the dose can be increased until MHO=3.5-4.5 is reached.
• Proven drug interactions with warfarin •• Drugs that enhance the effect of warfarin: amiodarone, ciprofloxacin, co-trimoxazole, disulfiram, fluconazole, cimetidine, clofibrate, erythromycin, metronidazole, sulfinpyrazone •• Drugs that reduce the effect of warfarin: barbiturates, carbamazepine, griseofulvin, rifampicin , menadione sodium bisulfite.
Complications • Embolism of the arteries of the great circle • Thrombosis of the prosthesis •• In case of thrombosis of a mechanical prosthesis, the use of thrombolytics and heparin in most cases eliminates the obstruction, at least partially •• The effectiveness of thrombolysis is monitored using echocardiography •• With a high risk of bleeding and severe hemodynamic disturbances, it is preferable surgical treatment (thrombectomy or valve replacement) •• If a thrombus forms on vegetations or overgrown connective tissue, thrombolysis is ineffective or not at all effective •• Definitive recommendations for the use of thrombolysis as an alternative to surgical treatment have not yet been developed • Severe bleeding •• Occur frequently, even with carefully controlled, therapeutic level of hypocoagulation •• With long-term anticoagulant therapy, a temporary dose reduction or complete elimination of hypocoagulation is usually well tolerated by patients •• To actively eliminate hypocoagulation, menadione sodium bisulfite (5-10 mg IV), fresh frozen plasma (1-2 doses) are administered ), eliminate the cause of bleeding (using endoscopic, endovascular or surgical intervention) and resume anticoagulant therapy.
Abbreviations • IE—infective endocarditis
2.Stages of operation
At the first stage
the patient is connected to cardiac monitors, the chest is processed, breathing tubes are inserted from an artificial respiration apparatus, which is connected only after the anesthesia begins to take effect (i.e., the only discomfort for the patient may be some soreness and soreness in the throat after the operation).
The anesthesiologist puts the patient under general anesthesia. From this moment on, the patient does not feel anything.
An ultrasound device is placed through the esophagus into the heart area, transmitting an image of the heart to a monitor throughout the operation.
Second phase
- This is the opening of the chest. After marking, the heart surgeon makes an incision on the chest from the top of the rib cage to the navel. With the minimally invasive method, the incision length is two-thirds shorter.
The purpose of the third stage
is connection to a machine that provides artificial blood circulation. During the operation, the blood is enriched with oxygen outside the lungs, then it returns to the aorta and moves through the systemic circulation.
At this stage, the surgeon stops the heart, washes it and places it in a special solution that maintains its viability outside the circulation.
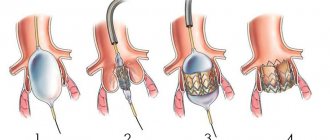
Fourth and fifth stages
- This is actually replacing the valve. The aorta is cut and the diseased valve is removed. If part of the aorta is also affected, it is also removed and a graft is placed. The valve hole is measured to select a new valve of the required size. The new valve is sewn on, then it is necessary to check that there are no leaks through it.
Sixth stage
- this is a disconnection from the artificial blood circulation machine. The aorta is sutured, and the trapped air is removed from the heart cavity. The heart begins to beat under the current of its own blood. If an uneven rhythm is observed, an electric shock is applied, which restores an even pulse.
Seventh stage
- chest closure. The bones and tissues are stitched together, and the sternum is closed with a suture that remains visible for life.
The entire operation usually lasts from 2 to 5 hours.
is important for the outcome of treatment .
It starts in the intensive care ward. Discharge from the hospital occurs 5-9 days after surgery. Postoperative rehabilitation continues on an outpatient basis.
Visit our Cardiology page
Prevention of thromboembolism
To prevent such a complication from developing, the doctor prescribes constant use of anticoagulants. If the operation went without problems, then therapy is prescribed on the second day, most often it is heparin, which is administered 4 to 6 times a day.
On day 5, the dose of heparin is reduced and indirect anticoagulants are administered. Once the desired prothrombin index is reached, heparin is discontinued altogether.
The doctor is obliged to tell the patient in detail about anticoagulant drugs, since they must be properly combined with the food consumed. These medications may not be combined with others or their effect may be reduced. This also needs to be taken into account. For any abnormalities in the patient's condition, the help of a doctor is necessary.
4. Lifespan of heart valves
Today, two types of heart valve implants are used in heart surgery: artificial and biological.
The first ones are durable, but their installation is associated with lifelong use of a number of drugs to eliminate the risk of blood clots. Biological valves are closest to living tissues, but wear out faster. Cardiologists are constantly working to develop and introduce into medical practice new types of valves that combine the best properties of both types - durability and maximum acceptability for the body. The service life of artificial valves is 10-15 years. Newer materials are still being studied. Widespread practice of their use in the near future will provide cardiologists with more accurate information about their service life.
Heart valve replacement: mitral, aortic - surgery, before and after
Have you been struggling with HYPERTENSION for many years without success?
Head of the Institute: “You will be amazed at how easy it is to cure hypertension by taking it every day.
Heart valves are the basis of the internal frame of the heart, which are folds of connective tissue. Their functions boil down to delineating the volumes of blood in the atria and ventricles, allowing these chambers to alternately relax after pushing out blood at the time of contraction.