What is atherosclerosis and what is its danger to human health?
At the beginning of the 21st century, cardiovascular diseases are the leading cause of death in the world.
In Russia, more than 50% of deaths occur due to heart and vascular disease. Of course, most cardiovascular diseases, in both men and women, occur after the age of 65 years. However, in recent years, heart disease has been steadily getting younger. And it is no longer uncommon to have a thirty-year-old “hypertensive” patient or a patient who suffered a heart attack at the age of 40-45.
What is the reason?
The answer is quite simple: atherosclerosis.
Atherosclerosis is a chronic, systemic, long-term disease that affects elastic (aorta) and muscular-elastic (arteries of the heart, brain) arteries. It has a wave-like course with phases of progression, stabilization and even reverse development of the disease.
But over the past 50 years, people have experienced a significant acceleration in the rate of development of atherosclerosis. If in the first half of the twentieth century such complications of atherosclerosis as heart attack and angina pectoris were not socially significant, today atherosclerosis is considered an epidemic.
The main element that determines the danger of atherosclerosis is the atherosclerotic plaque, which, protruding into the lumen of the vessel, causes its narrowing and impedes blood flow. An atherosclerotic plaque is a complex formation in its structure, consisting of an accumulation of lipids (fats), smooth muscle cells, and connective tissue. Atherosclerotic plaques can increase in size, rupture, and ulcers and blood clots can form on their surface. The result of the development of an atherosclerotic plaque will be a disruption of the free flow of blood through the vessel, up to its complete cessation.
Degrees of atherosclerosis
I degree – preclinical period of the disease
II degree – mild atherosclerosis
III degree – significantly pronounced atherosclerosis
IV degree – pronounced atherosclerosis
The clinical picture varies depending on the predominant localization and extent of the process and is determined by the consequences of ischemia of the tissue or organ.
In the twentieth century, several dozen theories were proposed to explain the origin and progression of atherosclerosis. But to date, none of them has been conclusively proven.
Let's try to figure out what leads to the formation of atherosclerotic plaques in blood vessels, and what reasons cause them to grow, rupture and lead to death.
One of the first theories of the development of atherosclerosis was the theory of excess cholesterol consumption, which was put forward by the famous Russian scientist N.N. Anichkov. “Without cholesterol there is no atherosclerosis.” This postulate has determined the tactics of treating patients for many years, and today has not lost its relevance. However, now we know very well: atherosclerosis is a complex disease, which is based on various disorders in the biochemical, genetic and immune processes of the body. And now it has become clear why a person with normal cholesterol levels can develop serious atherosclerosis.
Information for those who consider themselves completely healthy
Atherosclerosis itself, especially in the initial stages, may not manifest itself in any way.
This period is called the preclinical stage. It is very important to identify the disease at this stage, since the appearance of symptoms usually indicates the irreversibility of the process. Atherosclerosis is the main cause of the development of coronary heart disease, which is characterized by the appearance of chest pain during physical activity, the development of heart attack and heart failure, and serious heart rhythm disturbances. Sometimes the first clinical manifestation of atherosclerosis is a stroke or sudden death. Even this information is enough to make you think: “Do I have atherosclerosis or the risk of developing it?”
Currently, there are more than 200 risk factors for the development of atherosclerosis, but the main ones are arterial hypertension, smoking and disorders of lipid (cholesterol) metabolism. At the same time, smoking increases the risk of heart attack or stroke by 1.6 times, high blood pressure (BP) by 3 times, lipid metabolism disorders by 4 times, and the combination of these three factors increases the risk of vascular accidents by 16 times. Other significant risk factors for the development of atherosclerosis include: male gender, obesity, carbohydrate metabolism disorders (diabetes mellitus), age (over 60 years), the onset of menopause in women, unfavorable heredity for early cardiovascular pathology (relatives fell ill before 50-55 years of age) ), chronic stress. In addition, recently, in light of changing ideas about the causes of atherosclerosis, much attention has been paid to the presence of a chronic inflammatory process in the body, diseases of the liver and stomach (especially in the presence of Helicobacter pylori), and excessive levels of homocysteine in the blood.
It has been proven that almost all risk factors for atherosclerosis have an adverse effect on the endothelial cells that form the inner surface of the vascular wall. Damage to these cells and disruption of their function is a key point in the development of atherosclerosis.
So, the risk of developing atherosclerosis increases if:
- Do you smoke
- have arterial hypertension
- increased cholesterol levels were detected
- overweight
- diagnosed with diabetes
- you have unfavorable heredity (close relatives suffered from cardiovascular diseases before the age of 50)
- there is a pathology of the gastrointestinal tract (fatty hepatosis, chronic gastritis or peptic ulcer)
- menopause has arrived.
Atherosclerosis is dangerous due to its complications. It is necessary to identify it as early as possible in order to prevent the development of complications and begin timely treatment.
Obesity
Obesity
- excessive accumulation of adipose tissue in the body. Obesity is a multifactorial disease that is associated with numerous cardiac and metabolic risks. Body mass index (BMI) allows you to make a judgment about the content of adipose tissue. This indicator is calculated using the formula: BMI = Body weight (kg) / Height (m2).
The indicator is not informative for athletes, as well as for older people, since in the first case the muscles are overdeveloped, and in the second, on the contrary, they are atrophied.
The normal level of adipose tissue in men is 15–20% of body weight, in women – 25–30%.
Classification
There are several classifications of obesity. One of them takes into account BMI and the risk of cardiometabolic disorders.
Obesity level:
1) Normal weight, BMI < 25. 2) Overweight, BMI 25–29.9. 3) Obesity I degree, BMI 30–34.9. 4) Obesity II degree, BMI 35–39.9. 5) Stage III obesity, BMI >40.
Each group contains individuals with a metabolically healthy phenotype: WC in men ≤ 0.9; WC in women ≤ 0.85 and metabolically unhealthy phenotype: WC in men > 0.9; WC in women > 0.85, since not all obese people have metabolic disorders and, conversely, some people with normal body weight have disorders of carbohydrate and lipid metabolism. The group of “metabolically healthy obesity” includes those who, in addition to obesity, have one or less additional pathological factors against the background of normal tissue sensitivity to insulin.
According to the nature of the course, obesity can be progressive, stable and residual. The latter reflects residual effects after persistent weight loss.
Metabolism in adipose tissue and the pathogenesis of obesity
Adipose tissue is a type of connective tissue in the body. The main function of adipose tissue is to create an energy depot in the form of triglyceride reserves, provide thermal insulation, produce hormones and biologically active substances (adiponectin, leptin, etc.).
Adipose tissue is represented by a collection of fat cells - adipocytes. The number and size of adipocytes is a strictly individual indicator that varies from person to person. Under the influence of hormones such as insulin, glucocorticoids, T3, the number of adipocytes can increase.
The constancy of body mass and structure is ensured through the interaction of nervous and humoral mechanisms regulating food intake, consumption and storage in the form of energy.
The hypothalamus is the most important regulator of eating behavior, since it contains “. The hypothalamus controls the functioning of centers that control eating behavior and energy expenditure.
The hypothalamus receives signals:
- from the gastrointestinal tract about the filling of the stomach and other organs;
- about the chemical composition of blood - based on the content of glucose, amino acids, fatty acids;
- gastrointestinal hormones;
- adipose tissue hormones;
- signals from the cerebral cortex about the sight, taste and smell of food.
Some signals and substances stimulate feeding behavior, while others have an inhibitory effect. Factors regulating the amount of food consumed
In order for the amount of food eaten to actually correspond to the needs of the body, there are certain factors for the short-term and long-term regulation of food intake.
Mechanisms of short-term or rapid regulation:
1) Stomach fullness inhibits food consumption. 2) Eating stimulates the production of gastrointestinal hormones - cholecystokinin, peptide YY, glucagon-like peptide, which create a feeling of fullness. 3) The presence of food in the oral cavity, salivation, and swallowing inhibit the activity of the “hunger center” of the hypothalamus. 4) Level of ghrelin - a stomach hormone. After eating, its level decreases quickly, peak concentrations are observed before eating.
Mechanisms of long-term regulation:
1) A decrease in the concentration of glucose, amino acids, some fatty acids and keto acids leads to food motivation. When eating food, the concentration of insulin in the blood also increases. Insulin suppresses the activity of the “hunger center.”
2) Interaction with the “thermoregulation center”. Food consumption increases in cold conditions and decreases in hot conditions.
3) Signals from leptin - a hormone in adipose tissue that transmits a signal from adipose tissue about the body’s energy reserves. The increase in leptin levels is proportional to the increase in the amount of adipose tissue. An increase in the concentration of leptin in the blood promotes the development of a feeling of satiety and leads to a decrease in food consumption. In the hypothalamus, leptin initiates several responses at once, the essence of which is to reduce fat stores. Leptin inhibits the release of neuropeptide Y, which causes hunger; increases the activity of the sympathetic nervous system, increasing metabolic activity and energy expenditure; reduces insulin secretion by pancreatic b-cells.
Pathogenesis of obesity
If more energy contained in food enters the body than is consumed, then body weight increases.
The way to store energy is by storing fat. Therefore, the reason for the excess amount of adipose tissue is the excess of the intake of energy sources over its consumption. It does not matter what substances were supplied in excess quantities - proteins, fats or carbohydrates. Carbohydrates are a preferable source of energy than fats. When available, carbohydrates perform a fat-saving function. Excess carbohydrates that are not used for energy resources are converted into fats and stored. The same thing happens with excess proteins. Every 9.3 kcal of excess energy intake leads to the deposition of 1 gram of fat in the body. Fats accumulate under the skin, mainly in the thighs, buttocks and in the visceral spaces - in the omentum, mesentery. The liver and other organs also store small amounts of fat, but in smaller quantities. Recent studies have shown that new adipocytes can differentiate from progenitor cells at any period of life, and the development of obesity in adults is associated with an increase not only in the size of fat cells, but also in their number. Hormonal regulation of fat use 7 hormones have a strong regulatory effect on fat metabolism:
1) Adrenaline and norepinephrine are two hormones that work in stress reactions. Short-term and severe stress, heavy physical activity cause the mobilization of fats from the depot.
2) ACTH. The release of the hormone also increases under stress, while under the influence of ACTH the release of cortisol increases. Cortisol is a hormone of planned stress, unlike adrenaline and norepinephrine. Cortisol has a ketogenic effect on fat mobilization. If stress is long-term, then a prolonged and persistent increase in cortisol leads to obesity, which is accompanied by Cushing's syndrome/disease.
3) Growth hormone. Activates lipolysis and thereby increases the breakdown of fats. In obesity, the concentration of the hormone decreases due to an increase in the concentration of free fatty acids and insulin.
4) Thyroid hormones. They stimulate the mobilization of fats because they increase basal metabolism in cells. With a deficiency of triiodothyronine, thyroxine, hypothyroidism, obesity is observed, as the level of basal metabolism in cells decreases.
5) Insulin. Activates the process of synthesis and storage of fat - lipolysis.
Causes of obesity
There are a complex of reasons leading to obesity. There is a genetic determination of the intensity of energy metabolism and food consumption, but sometimes environmental factors and lifestyle play a dominant role in the development of obesity. 1) Reduced energy expenditure, including insufficient physical activity. In obese people, little physical activity is associated with weight loss and increased body fat. About 25–30% of daily energy expenditure comes from energy expenditure associated with muscle function. Therefore, regular physical activity and training increases muscle mass and reduces the amount of fat tissue. Even a single bout of exercise increases basal energy expenditure for several hours after cessation of exercise.
2) Eating disorder. Despite the presence of physiological mechanisms in the body that regulate food consumption, many harmful eating habits can cause the development of obesity. It has been proven that fat-rich foods predominate in the diet of obese people. Such products stretch the walls of the stomach to a lesser extent, have excessive calorie content, and do not require long chewing. Foods rich in fat taste better because they contain fat-soluble aromatic molecules that determine its taste. Additionally, the body requires less energy to store fats than carbohydrates. 3) Psychogenic factors. Some people develop obesity due to psychological factors. A sharp increase in body weight is observed during or after stress, as the sensitivity of the “saturation center” decreases. For example, the loss of a close relative, dismissal, serious illness and depression often cause overeating. For such a person, food becomes a means of reducing emotional stress.
4) Overfeeding children. The rate of formation of new fat cells is especially high in the first years of life. The higher the rate, the more adipocytes will differentiate in the body, the higher the risk of obesity.
5) Leptin resistance. In obese people, leptin levels are high, but the hypothalamic receptors become insensitive to its signals or the signal transmission process is disrupted. As a result, the sensitivity of the “satiety center” decreases, and a tendency to overeat appears. This condition is called leptin resistance. It is fraught with the fact that it contributes to the development of insulin resistance. Both conditions are risk factors for developing cardiovascular disease and type 2 diabetes. 6) Neurogenic disorders. Conditions such as tumors and injuries to the pituitary gland and hypothalamus can disrupt the regulatory systems that control eating behavior. 7) Genetic predisposition. Obesity often occurs as a family disease. The likelihood of developing overweight if your parents are obese is 70–80%. Concomitant diseases
Complications and diseases associated with obesity include:
- impaired glucose tolerance (IGT), impaired fasting glucose (IFG), or a combination thereof (any of the three positions characterizes the state of prediabetes);
- diabetes mellitus type 2;
- arterial hypertension;
- hypertriglyceridemia/dyslipidemia;
- obstructive apnea syndrome (syndrome of temporary cessation of breathing during sleep);
- non-alcoholic fatty liver disease;
- polycystic ovary syndrome;
- osteoarthritis;
- stress urinary incontinence;
- gastroesophageal reflux disease (GERD);
- limitation of mobility and social adaptation;
- psychoemotional disorders and/or stigmatization.
There is still no clear understanding of whether these conditions are a consequence or a cause of obesity, so it is customary to classify them as associated. Diagnosis of obesity
The diagnosis of obesity and further management of the patient are based on anamnestic data and data obtained as a result of an external examination, laboratory and instrumental examination.
When collecting anamnesis, the doctor clarifies the time of onset of obesity, is interested in the dynamics of weight changes, whether relatives have obesity, what kind of lifestyle, physical activity, and nutrition the patient has.
During the examination, the waist size, hip size must be measured, and the WC/TB ratio and body mass index are calculated.
Depending on the type of distribution of adipose tissue, obesity is:
- Visceral. Deposition of adipose tissue in the chest and abdomen, like an “apron”. Associated with a high risk of developing cardiovascular disease and type 2 diabetes. Waist to hip ratio >1.0.
- Peripheral. Deposition of adipose tissue in the buttocks and thighs. Associated with diseases of the spine and joints. Waist to hip ratio <1.0.
- Mixed. Characterized by an even distribution of adipose tissue.
If there is a need to evaluate in more detail the nature of the distribution of adipose tissue, the doctor will refer you to perform CT, MRI and ultrasound.
Standard for minimum laboratory examination for diagnosing metabolic disorders in obesity:
- Determination of the blood lipid spectrum (TC, HDL, LDL, ).
- Determination of carbohydrate metabolism indicators (fasting blood glucose, GTT, HbAC).
- Leptin, adiponectin.
- Indicators of liver and kidney function: ALT, AST, GGT, uric acid, creatinine.
- ECG.
Obesity caused by excess supply of energy resources must be distinguished from secondary or symptomatic obesity.
As a rule, it is associated with hereditary, endocrine and other somatic pathologies. Therefore, making a final diagnosis often requires the help of several specialists - a cardiologist, endocrinologist, neurologist, nutritionist, psychotherapist. To carry out differential diagnosis of various forms of obesity, special diagnostic algorithms are used: To exclude the hypothalamic genesis of obesity:
- examination by an endocrinologist, examination by a neurologist.
To exclude hypercortisolism:
- examination by an endocrinologist;
- dexamethasone test;
- laboratory tests: cortisol in 24-hour urine, ACTH.
To rule out PCOS:
- examination by a gynecologist;
- Ultrasound of the pelvic organs;
- blood hormones: , FSH, prolactin, testosterone, estradiol, DHEA-S, 17-hydroxyprogesterone (17-OP), SHBG;
- biochemical blood test: fasting plasma glucose, lipid spectrum, HOMA-IR.
To rule out hypothyroidism:
- examination by an endocrinologist;
- blood pressure measurement;
- laboratory tests: TSH, BC, lipid profile.
To exclude hyperprolactinemia:
- examination by an endocrinologist, examination by an ophthalmologist;
- laboratory tests: prolactin, lipid profile;
- MRI of the brain.
Diagnostics
The main tests for diagnosing atherosclerosis are:
- lipid profile
- angiography
- Dopplerography (ultrasound screening for atherosclerosis).
The very first step that needs to be taken towards identifying atherosclerosis is to take a simple blood test for the lipid spectrum. In this case, a detailed lipid profile is required, and not just a blood test for cholesterol. After all, it is known that atherosclerosis can develop even with a normal level of total cholesterol, and the low level of so-called “good cholesterol” is to blame for this.
A blood test for the lipid spectrum is taken from a vein, on an empty stomach (after a 12-14 hour fast).
What indicators of lipid metabolism are currently accepted as the norm?
The lipid profile will show the following indicators:
- total cholesterol level – should be less than 5.2 mmol/l
- the level of low-density lipoproteins (LDL, beta lipoproteins, “bad cholesterol”) should be less than 3.0 mmol/l
- the level of high-density lipoproteins (HDL, alpha lipoproteins, “good cholesterol”) – should be more than 1.2 mmol/l
- triglyceride (TG) level – less than 1.7 mmol/l
- atherogenic coefficient (AC) – should not exceed 4.0 c.u.
- in some cases chylomicrons (CM) and very low density lipoproteins (VLDL) will be indicated
If the lipid profile data differs from the given standards, even in one of the parameters, this is a reason to seek advice from a cardiologist.
What methods can be used to confirm the presence of atherosclerosis or to identify impaired function of the vascular wall, which is the initial stage of the development of atherosclerosis?
The EXPERT Clinic provides ultrasound screening for atherosclerosis. Using an ultrasound machine, the carotid (sometimes femoral) arteries are examined to identify changes in the vascular wall or identify asymptomatic atherosclerotic plaques. Since atherosclerosis is a disease that affects all blood vessels, the condition of the carotid arteries can indirectly judge the condition of all vascular areas of the body.
To identify impaired endothelial function, a special test is performed under ultrasound control, the so-called “Reactive Hyperemia Test”. This is a highly sensitive method that allows you to identify disorders at very early stages and predict the risks of developing cardiovascular pathology in people without any complaints, as well as monitor the treatment process in patients with proven pathology. The EXPERT clinic is one of the few institutions in the city where this research is performed.
What will happen if you don’t pay attention to your health and ignore the “first signs”? Atherosclerosis will develop, progress and will inevitably lead to serious complications associated with impaired blood flow in vital organs.
Atherosclerosis is a serious disease that is easier to prevent than to treat.
An atherosclerotic plaque is a kind of patch on the vascular wall. It is no longer possible to “dispute” it; one can only prevent its further growth.
Now there is a lot of popular scientific literature devoted to atherosclerosis, and many patients say, we know that cholesterol has nothing to do with it. At the very beginning of the article, we also mentioned this: not only cholesterol is to blame for the development of atherosclerosis. There are about 200 other factors!
Let's look at one of them in a little more detail: homocysteine.
Homocysteine is an amino acid that is not found in food, but is formed in the body from another amino acid, methionine. Animal products (meat, dairy products, eggs) are rich in methionine. Excessive accumulation of homocysteine inside cells can cause irreparable harm to them, including cell death. Homocysteine has a direct toxic effect on endothelial cells, damages them (patch-plaques are formed in places of damage), increases cholesterol levels in the blood, enhances blood clotting and accelerates the growth of existing atherosclerotic plaques.
The metabolism (destruction) of homocysteine in the body occurs with the participation of vitamins B6, B12 and folic acid. Homocysteine is excreted from the body by the kidneys.
Reasons for the development of elevated homocysteine levels:
- age and gender (over 55 years old, men, menopausal status in women)
- nutrition and lifestyle (smoking, lack of folic acid and vitamins B6, B12 in food, excessive consumption of meat products and foods rich in methionine, drinking coffee more than 6 cups a day, excessive alcohol consumption, cholesterol-rich diet)
- diseases (diabetes mellitus, renal failure, hypothyroidism, various tumors)
- medications (anticonvulsants, long-term use of hormonal contraceptives, etc.)
Today it has become clear that without controlling homocysteine levels it is impossible to effectively prevent and treat diseases of the cardiovascular system.
How can you reduce the negative impact of homocysthenia?
There is only one way - to compensate for the deficiency in the body, first of all, of folic acid, as well as vitamins B6 and B12. Taking vitamins in the required dosages (which can only be determined by a doctor) helps reduce homocysteine levels in the blood.
What level of homocysteine is dangerous?
A homocystenine level of 10 µmol/l or lower is considered normal.
An increase of more than 20 µmol/l leads to a 4-fold increase in mortality from cardiovascular complications.
At the EXPERT Clinic, you can check the level of homocystenine, along with the lipid spectrum of the blood, especially if you are in a risk group.
What to do if atherosclerosis is detected late and its complications already exist?
Do not panic!
In any case, treatment is necessary to prevent further progression of the disease. But more aggressive therapy using various groups of drugs will be required.
What are the complications of atherosclerosis?
When the heart vessels are damaged, a malnutrition of the heart muscle develops; this, as a rule, leads to pain in the chest during physical activity, but sometimes it can be asymptomatic and manifest itself only by the development of myocardial infarction, which, unfortunately, can result in the death of the patient.
If the vessels supplying the brain are damaged, the risk of developing ischemic stroke is very high. A disease that, as a rule, leads to deep disability of the patient and forever changes his life and the lives of his loved ones.
In men, especially smokers, one of the first manifestations of atherosclerosis is damage to the blood vessels of the legs, which first appears as mild fatigue in the legs when walking quickly, then pain in the legs appears and it is no longer possible to walk more than 100 meters without stopping. This could end in gangrene and amputation! But tell me, how many modern men walk at least 2 kilometers a day every day? Many of them are driving, and therefore simply cannot detect the first symptoms of the disease. But it has already been mentioned that male gender is a separate risk factor for the development of cardiovascular diseases.
At this stage of development of atherosclerosis, an extensive instrumental examination is required, the scope of which must be determined by a cardiologist.
Summarizing all of the above, we suggest you think about your future and the future of your loved ones. Contact the specialists of the EXPERT Clinic, undergo a minimal or extensive examination and live long and happily.
If abnormalities are detected in the blood lipid spectrum, or any risk factors for atherosclerosis, you must make an appointment with a cardiologist.
As a result you will receive:
- individual consultation on whether you have a disease or a predisposition to it
- the doctor will draw up a plan for the necessary instrumental or laboratory examination to clarify the diagnosis
- will give recommendations on changes in diet and lifestyle, and also assess the need for drug therapy
- will teach you how to properly monitor parameters such as blood pressure, blood sugar, weight fluctuations
- will recommend the necessary physical activity taking into account your condition
Collaboration between doctor and patient is the key to the success of treating any disease, especially such an insidious one as atherosclerosis. If a diagnosis of atherosclerosis is established, the patient must be under the supervision of a cardiologist at least once every 6 months, and when correcting disorders and identified complications of the disease, the frequency of meetings and the scope of additional examinations are determined individually.
LIPID METABOLISM DISORDERS AND ATHEROSCLEROSIS: relevance of the problem and diagnosis
What is the relationship between markers of systemic inflammation and ischemic heart disease? What are the fractions of lipoproteins?
Diagnosis, treatment and prevention of atherosclerosis remain the most important task of modern medicine, the solution of which largely determines the success of the fight against diseases such as heart attack, stroke and other cardiovascular complications. Proved during the Framingham study conducted in the early 60s, the relationship between lipid metabolism disorders and the development of atherosclerosis, in particular coronary (coronary) heart disease, was confirmed in many subsequent studies.
Currently, a number of risk factors for the development of atherosclerosis and coronary heart disease (CHD) have been identified, which include:
- lipid metabolism disorders;
- arterial hypertension;
- smoking;
- excess body weight;
- heredity;
- impaired carbohydrate tolerance;
- male gender;
- increased levels of markers indicating the presence of inflammatory changes.
One patient most often has two or more risk factors. Moreover, even if each individual indicator is increased slightly, but there are two or three or more risk factors, the likelihood of developing cardiovascular diseases increases exponentially [1].
In practice, to assess this total risk, tables recommended by the European Society of Cardiology are used, which take into account factors such as the patient’s gender, smoking, age, blood pressure, and cholesterol levels. These indicators are expressed as a percentage and indicate the likelihood of developing complications of coronary artery disease or death over ten years. Assessment of this total risk is decisive for determining the tactics of preventive and therapeutic measures. A risk of 20% over ten years was taken as a value indicating the need for active preventive and therapeutic measures. These risk factors are especially important in patients already suffering from coronary artery disease.
Unfortunately, the tables cannot take into account all risk factors. In the presence of these factors in patients with diabetes, the risk of developing complications increases even more. There is still no complete certainty regarding the significance of factors such as physical inactivity and the age of patients. The LA-VA Study (Los Angeles Veteran Administration Dietary Study) involved treatment with enterosorbent cholestyramine in combination with niacin (a slow-release form of niacin) on the background of a strict cholesterol-lowering diet. Over eight years, a reduction in mortality was found in people under 65 years of age, while there was no effect in people over 70 years of age. Many researchers have different assessments of the importance of dyslipidemia as one of the most important risk factors for cardiovascular diseases in patients over 80 years of age. Research into the effectiveness of cholesterol-lowering therapy in this age group is currently underway.
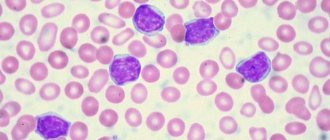
Recently, great importance has been attached to the presence of markers indicating inflammatory changes. Classic pathophysiological studies have demonstrated the presence of inflammatory cells such as monocytes, macrophages and T lymphocytes at all stages of atherosclerosis. These morphological changes precede endothelial cell dysfunction, causing adhesion molecules to interact with inflammatory cells.
In recent years, it has been proven that the appearance of markers of systemic inflammation, such as CRP (C-reactive protein), fibrinogen, etc., precedes the development of cardiovascular complications [6, 7]. These changes can also be detected in patients with unstable angina even before the development of focal changes in the myocardium. Their presence in patients with high levels of total cholesterol (TC) and low-density lipoprotein cholesterol (LDL-C) sharply increases the risk of complications. The ECAT study (European Concerted Action on Thrombosis and Disabilities Angina Pectoris Study) demonstrated an increased risk of cardiovascular complications in patients with stable angina and high CRP levels compared with similar patients with low CRP levels [5]. According to Berk, 90% of patients with unstable angina had an increased level of CRP, and with stable angina this indicator was increased only in 13% of patients [4]. Liuzzo showed that patients with unstable angina and elevated CRP levels were more likely to have ischemic attacks, require surgical treatment, and have a higher percentage of acute myocardial infarction (AMI) than a similar group of patients with unstable angina and low CRP levels. SRB [8]. The SHHS (Scottish Heart Health Study) study conducted in 1998, using an example of almost 10 thousand patients, demonstrated a close relationship between elevated levels of plasma fibrinogen and the development of coronary artery disease and mortality from cardiovascular diseases [10]. Perhaps these changes will help explain the cases of atherosclerosis in patients with normal levels of total cholesterol and LDL cholesterol.
For a more adequate analysis of lipid metabolism disorders, it is important to evaluate not only the level of total cholesterol in the blood, but also the level of LDL-C, high-density lipoprotein cholesterol (HDL-C), their ratio, atherogenic index, triglyceride (TG) level, as well as the level of Apo-C. proteins A and B, on which the transport function of lipoproteins depends. According to their physical properties, blood plasma lipoproteins are divided into the following fractions: chylomicrons, very low density lipoproteins (VLDL), intermediate density lipoproteins (IDL), LDL, HDL.
The atherogenicity index is defined as the ratio of the difference between total cholesterol and HDL-C to HDL-C. Even more important is to determine the level not of lipoproteins, but of the apo-proteins that make up them. However, at present, these methods are just beginning to be introduced into clinical practice. Normal levels of essential lipids are presented in table. 1.
To make it easier to remember normal indicators, you can use the one-two-three-four-five rule, in which:
- less than 5 – total cholesterol level;
- less than 4 - atherogenic index;
- less than 3 - LDL-C level;
- less than 2 - TG level;
- more than 1 – HDL-C level.
These standards, except for the atherogenic index, are presented in mmol/l. Measurements of cholesterol and triglycerides in mg/dL are also found in the literature. To convert mg/dL to mmol/L, the value measured in mg/dL must be divided by 38.7 (for cholesterol) and 88.5 (for triglycerides).
However, in practical medicine, in most patients with ischemic heart disease or with numerous risk factors, a detailed study of the lipid profile is not carried out or is not carried out in full. Thus, the number of patients with coronary artery disease whose lipid profile was studied in the USA in 1999 was only 44% (out of 48,586 patients); the target LDL-C level of less than 100 mmol/L (100 mg/dL), recommended by the American Heart Association, was achieved in only 25% of these patients [9]. Achieving this level in only one quarter of patients demonstrates a lack of alertness and underestimation of the importance of timely correction of these indicators. We do not have similar data for Russia, but it is difficult to imagine that the result would be more encouraging.
In our opinion, the attitude towards standard indicators is extremely important. The tactics described in many guidelines and textbooks, which involve prescribing non-drug treatment for patients with hypercholesterolemia for two months followed by re-examination of the lipid profile, should be followed only in cases where we are talking about the primary prevention of coronary artery disease or patients with coronary artery disease with stable angina. In cases of severe dyslipidemia, combined with a clinical picture of progressive angina and/or changes in functional tests, it is necessary to carry out rapid and fairly aggressive treatment. While agreeing with the importance of providing this group of patients with non-drug treatment in full, we are forced to focus on the need for simultaneous initiation of drug therapy. With severe hypercholesterolemia in such patients, pinning hopes on the effectiveness of non-drug treatment means wasting time and exposing the patient to additional risk. The same can be said about drug treatment with cholesterol-lowering drugs in patients with acute coronary syndrome (unstable angina and Q-non-forming MI) with normal or slightly elevated levels of TC and LDL-C. This is explained by the fact that statins have not only a hypocholesterolemic effect. Thus, in patients with unstable angina, a decrease in TC levels during statin therapy was accompanied by an improvement in vascular endothelial function, observed after six weeks (Dupurs J. et al, 1999) [11].
Depending on the increase in a particular fraction of cholesterol and/or triglycerides, five types of dyslipidemia are distinguished (according to Fridrikson) [2]. The WHO classification with the estimated risk of developing atherosclerosis, based on the Fridrikson classification, is presented in table. 2.
The most atherogenic, dangerous in terms of the development of cardiovascular diseases and widespread are dyslipidemias of type IIA, IIB and IV. If it is impossible to conduct a detailed analysis of the lipid profile, these types of dyslipidemia can be identified by determining only cholesterol and TG.
Data that allows us to identify the type of dyslipidemia by the level of these indicators are presented in Table. 3.
This classification, although quite simple and understandable for clinicians, still has a number of disadvantages. Thus, it did not include HDL-C, the significance of which is extremely important for deciding on treatment tactics and prognosis.
No less important is the determination of the causes of dyslipidemia, which are divided into primary and secondary [3].
Primary hypercholesterolemia is caused by hereditary disorders of lipid metabolism. In familial hypercholesterolemia, “defective” genes responsible for the synthesis of LDL receptors are inherited. In the homozygous form, the synthesis of receptors is completely impaired. This leads to the inability to capture LDL and their rapid accumulation in the blood. This form is characterized by clinical manifestations already in early childhood, it is accompanied by the development of vascular complications and the formation of tendon xanthomas. In the heterozygous form, the number of receptors is significantly reduced, but they are still present, so the disease develops more slowly and atherogenic complications appear by the age of 25-30. This is most often type IIA dyslipidemia with a significant increase in the level of TC, LDL-C and normal TG levels. In the clinical picture in such patients, xanthomas and xanthelasmas are often found. Familial combined and polygenic hypercholesterolemia is also very common in this group. Familial hyperlipidemia type III is much less common. Cases of familial hyperalphacholesterolemia are usually not accompanied by the development of atherosclerotic diseases and do not pose a threat to the patient.
Secondary dyslipidemias are much more common. They are either caused by malnutrition, when there is excessive consumption of food rich in cholesterol, or arise as a result of diseases such as hypothyroidism, nephrotic syndrome, gout, diabetes mellitus, obesity, etc. Lipid metabolism disorders can arise or worsen during the treatment of other diseases drugs such as thiazide diuretics, immunosuppressants. The role of b-blockers is limited to an increase in TG levels and a slight decrease in HDL-C levels. The negative proatherogenic effect is significantly inferior to the positive effect of b-blockers as anti-ischemic, antiarrhythmic and antihypertensive agents [3].
Dyslipidemias are one of the most important causes of the development of atherosclerosis, so their timely diagnosis and proper treatment can slow down the development of atherosclerosis and reduce the risk of cardiovascular complications.
Literature
1. Libov I.A., Cherkesova S.V., Roitman A.P. Modern aspects of dislipoproteinemia and practical approaches to their treatment // Moscow Medical Journal.
No. 3. 1998. pp. 34-37. 2. Thompson G. R. Guide to hyperlipidemia. MSD, 1990. 3. Shpector A.V., Vasilyeva E.Yu. Cardiology: keys to diagnosis. Vidar, 1996, p. 295-309. 4. Berk BC, Weintraub WS, Alexander RW Elevation of C-reactive protein in “activ” coronary artery disease // Am. J. Cardiol. 1990: 98: 2219-2222. 5. Haverkate F, Thompson SG, Pyke SDM et al, for the European Concerted Action on Thrombosis and Disabilities Angina Pectoris Study Group. Prodaction of C-reactive protein and risk of coronary events in stable and unstable angina // Lancet. 1997; 349: 462-466. Table 1. Normal plasma levels of major lipids determined by enzymatic methods
| Indicators | Plasma content |
| Total cholesterol | 3.5-5.2 mmol/l |
| LDL-C | Up to 3.5 mmol/l |
| HDL-C | 0.9-1.9 mmol/l |
| TG | 0.5-2.0 mmol/l |
| Atherogenic index according to Klimov | Up to 4 |
Return
Note!
- The appearance of markers of systemic inflammation (C-reactive protein, fibrinogen) precedes the development of cardiovascular complications
- The most atharogenic, dangerous in terms of the development of cardiovascular diseases and widespread are dyslipidemias of type IIA, IIB, IV
- Primary hypercholesterolemia is caused by hereditary disorders of lipid metabolism
- Secondary dyslipidemia is caused by malnutrition or occurs as a result of diseases such as hypothyroidism, nephrotic syndrome, gout, diabetes mellitus, obesity
Table 2. WHO classification of hyperlipidemias
| Type | HCO | LDL-C | TG | Lipoprotein disorder | Risk of developing atherosclerosis |
| I | Promoted | Decreased or normal | Increased | Excess chylomicrons | Not promoted |
| IIA | Increased or normal | Promoted | Fine | Excess LDL | Sharply elevated, especially in the coronary arteries |
| IIB | Promoted | Promoted | Increased | Excess LDL and VLDL | Same |
| III | Promoted | Decreased or normal | Increased | Excess of chylomicron remnants and DILI | Significantly increased, especially for coronary and peripheral arteries |
| IV | Increased or normal | Fine | Increased | Excess VLDL | Likely elevated for coronary atherosclerosis |
| V | Promoted | Fine | Increased | Excess chylomicrons and VLDL | Dont clear |
Return
Table 3. Diagnosis criteria for the main types of dyslipidemia
| Type of dyslipidemia | HS | TG |
| IIA | > 5.2 mmol/l | < 2.0 mmol/l |
| IIB | > 5.2 mmol/l | > 2.0 mmol/l |
| IV | < 5.2 mmol/l | > 2.0 mmol/l |
Return
Treatment stories
Case No. 1
Alexey, 27 years old. Young specialist, graduate of a medical university. He has no health complaints. Is overweight (grade 1 obesity). Blood pressure was not monitored, blood lipid levels were unknown. He has been smoking for about 10 years. At the request of my colleagues, I took part in one of the medical studies and conducted the “Reactive Hyperemia Test.” As a result of the test, pronounced dysfunction of the endothelium was revealed. Taking into account the data obtained, I began to monitor my blood pressure (BP) numbers and was surprised to find borderline values: my blood pressure averaged 130/90 mm Hg. Art. In the lipid spectrum, all indicators were normal except for a slightly reduced level of “good cholesterol”, which was 1.0 mmol/l. Upon questioning, it turned out that the family has a tendency to develop hypertension and diabetes, and the father suffered a heart attack at the age of 57 years. All this forced the young man to take a very responsible approach to his future. He quit smoking, began to control his weight, and increased physical activity. After 6 months, control tests showed normalization of endothelial function. Blood pressure values assessed using 24-hour Holter monitoring were also within normal limits. A repeated study of the lipid spectrum revealed the level of “good cholesterol” remaining moderately reduced, which indicated its hereditary nature. However, given the absence of other risk factors for the development of atherosclerosis, this deviation is insignificant.
Case No. 2
Margarita, 62 years old. 10 years ago, significantly elevated cholesterol levels (more than 8.0 mmol/l) were detected. After menopause at age 52, my blood pressure began to rise. However, the patient was not overweight and never smoked. The patient did not let things take their course, but promptly contacted a cardiologist at the EXPERT Clinic 4 years ago. An examination was carried out: ultrasound screening for atherosclerosis, which revealed diffuse thickening of the vascular wall of the carotid arteries (intima-media complex), and a single atherosclerotic plaque 2.5 mm high. Taking into account the latest international recommendations, thickening of the intima-media complex of the vascular wall is an indication for drug therapy to lower cholesterol. The patient began to follow a strict diet, limiting animal fats. Medications were prescribed to control blood pressure, and therapy was started on medications aimed at lowering cholesterol levels. The patient has been observed in the clinic for 4 years. Repeated ultrasound screening for atherosclerosis does not reveal any violations of the vascular wall, and the atherosclerotic plaque has decreased in height to 1.8 mm, its structure has become dense (such plaques are not dangerous in terms of the development of complications). Blood pressure figures are within normal limits, lipid metabolism indicators are normal.
Case No. 3
Konstantin, 60 years old. I contacted the EXPERT Clinic. At the reception he claimed that he was absolutely healthy and came only because “his wife ate all her baldness.” A thorough questioning indeed did not reveal any serious complaints, but the patient said that he loves to eat, smoked for more than 20 years, but quit a year ago, does not exercise and generally walks little, but at work he is always “in good shape” and “happy.” During the examination, the pressure was elevated, which surprised him very much, since at home, with rare measurements (“for company”), the numbers, according to him, were normal. He didn't check his cholesterol levels. Taking into account all the data, the patient was prescribed an extensive laboratory and instrumental examination, which included a study of the lipid spectrum and carbohydrate metabolism, 24-hour ECG and blood pressure monitoring, echocardiography and ultrasound screening for atherosclerosis. Data from a comprehensive examination revealed the presence of persistent arterial hypertension, complicated by the development of left ventricular hypertrophy, episodes of silent ischemia of the heart muscle during exercise, pronounced changes in the lipid spectrum in the form of increased levels of cholesterol and triglycerides, as well as low levels of “good cholesterol”. There were borderline levels of glucose in the blood. The most dramatic thing was the detection of atherosclerotic plaques in the carotid arteries, one of which blocked the vessel by more than 80%, which increases the risk of stroke significantly. The patient was prescribed serious multicomponent drug therapy and given recommendations for lifestyle changes. The patient also had a consultation with a vascular surgeon, who insisted on performing coronary angiography. During this study, the patient was diagnosed with critical stenosis of one of the coronary arteries, which required stenting, since the risk of myocardial infarction was very high. The patient continues to be observed at the EXPERT Clinic and very responsibly follows all the recommendations of specialists.
Dyslipidemias are one of the most common metabolic disorders. The connection between dyslipidemia and dermatoses, for example, the connection between psoriasis and dyslipidemia, was discovered relatively recently. Many dermatoses may have a systemic inflammatory component, which explains this association. Chronic inflammatory dermatoses may have other metabolic imbalances that may contribute to dyslipidemia. The presence of such abnormal metabolism may justify routine screening of these diseases for the presence of dyslipidemia and other metabolic disorders, for early treatment of such comorbidities and improvement of the patient's quality of life. Some of the drugs used by dermatologists, such as retinoids, are also likely to cause dyslipidemia. Therefore, it is critical that dermatologists gain scientific knowledge of the underlying mechanisms involved in dyslipidemia and understand when to adjust treatment. This review attempts to list the dermatological diseases associated with dyslipidemia; to simplify understanding of the underlying mechanisms; and give a brief overview of treatment adjustments.
Introduction
Dyslipidemia is a disorder of lipoprotein metabolism, including excess lipoproteins and their deficiency. These disorders may manifest as increased serum concentrations of total cholesterol, low-density lipoprotein (LDL), triglyceride (TG) concentrations, and decreased concentrations of high-density lipoprotein (HDL). [1] Blood lipid changes are a growing health problem worldwide. Studies conducted in India have shown an increase in the prevalence of dyslipidemia, even among the young adult population. [2] Dyslipidemia plays a critical role in the development of cardiovascular diseases, which has become the leading cause of death in most developed and developing countries. [3] It is now known that dermatological diseases such as psoriasis are associated with dyslipidemia. [4] Some dermatological treatments are known to predispose to lipid disorders. A clear understanding of the pathogenesis of such events allows us to provide appropriate advice to patients.
Pathogenesis of dyslipidemia
Dyslipidemia may result from overproduction of lipoproteins or lack of clearance of lipoproteins, may be associated with other defects in apolipoproteins, or there may be a deficiency of metabolic enzymes. The pathways and means of lipid metabolism in the human body reflect the interaction of genetics, complex biochemical processes influenced by diseases, drugs and/or environmental factors. Phenotyping these dyslipidemias is challenging and has been ongoing for many decades. [5]
Primary dyslipidemia (eg, familial hypercholesterolemia) typically refers to a genetic defect in lipid metabolism that causes abnormal lipid levels. Secondary dyslipidemia can be due to various causes, such as environmental factors (diet rich in saturated fat or sedentary lifestyle), diseases (type 2 diabetes, hypothyroidism, jaundice, etc.), and medications (thiazide diuretics, progestins, anabolic steroids, etc.). Secondary dyslipidemias can be corrected or corrected by treating the underlying disease. Dyslipidemia may result from a combination of genetic and secondary causes. [5]
Dyslipidemia and skin
Many dermatological diseases are known to be associated with dyslipidemia. Most of them are chronic inflammatory diseases and the secretion of proinflammatory cytokines may be the basis of their pathogenesis. Studies have shown an increased risk of dyslipidemia in skin diseases such as psoriasis, lichen planus, pemphigus, granuloma annulare, histiocytosis and connective tissue diseases (such as lupus erythematosus). Table 1 shows lipid disorders and associated diseases.
Table 1. Dermatological diseases associated with dyslipidemia
| Disease | Deviations in the lipid spectrum |
| Psoriasis | Low HDL, elevated total cholesterol, TG and LDL |
| Lichen planus | High LDL, total cholesterol, increased ratio of total cholesterol to HDL and LDL to HDL |
| Pemphigus | High levels of total cholesterol and TG |
| Granuloma annulare | Low HDL, elevated total cholesterol, TG and LDL |
| Discoid lupus erythematosus | Low levels of HDL, HDL2, HDL3 subratios |
| Histiocytosis | hypercholesterolemia |
Psoriasis is a chronic inflammatory, immune-mediated skin disease affecting 2-3% of the population, characterized by hyperproliferation and altered differentiation of keratinocytes. [6] The exact etiology of psoriasis is unknown; one theory suggests that the disease has an autoimmune basis with a strong genetic component. Several cardiovascular risk factors are also associated with psoriasis. [4,7] Some studies, although with relatively small patient groups, have shown an atherogenic dyslipidemic profile consisting of increased levels of total cholesterol, triglycerides, LDL, oxidatively modified lipids, and decreased HDL levels. [8,9,10] Recent studies have also shown that the prevalence of metabolic syndrome is significantly higher in patients with psoriasis compared with controls after the age of 40 years and patients with psoriasis have an increased risk for individual components of the metabolic syndrome. [11,12,13] Components of metabolic syndrome include hyperglycemia, obesity, hypertension, and dyslipidemia.
Lichen planus is also a common chronic inflammatory skin disease. There are reports of an association of lichen planus with dyslipidemia [14,15,16]. Chronic inflammation in patients with lichen planus may explain the association with dyslipidemia. Studies have reported that patients with lichen planus have significantly higher levels of various lipids compared to controls [Table 1] [15]. Screening lipid levels in men and women with lichen planus may be useful in identifying those at increased risk so that preventive treatment can be initiated to prevent the development of cardiovascular disease. [16]
Lichen planus. is a common chronic inflammatory disease of the skin and mucous membranes, which is characterized by a wide range of clinical manifestations. Its classic clinical presentation is associated with the appearance of purple, polygonal papules and plaques.
Pemphigus vulgaris is a potentially fatal autoimmune blistering disease affecting the mucous membranes and skin, often requiring long-term, immunosuppressive treatment. [17] The association between pemphigus and dyslipidemia was established in a case-control study conducted at the medical base of a large health care organization in Israel. They observed an association between pemphigus and dyslipidemia by examining serum lipid profiles. Serum total cholesterol and triglyceride levels were elevated in patients with pemphigus compared with controls. Lipid levels were even higher when factors such as obesity, diabetes and hypertension were present; unrelated to corticosteroid use. Neither LDL nor HDL was associated with pemphigus. [18]
Hypercholesterolemia, hypertriglyceridemia, elevated LDL cholesterol, and low HDL cholesterol have been demonstrated in patients with granuloma annulare. More common in generalized forms than in localized ones, the morphology of ring-shaped lesions has been found to be associated with hypercholesterolemia and dyslipidemia. [19]
Patients with discoid lupus erythematosus are known to have lipid abnormalities that aggravate the disease. In addition, there is an increased risk of atherosclerosis due to noted disease-associated dyslipidemia. [20]
Non-Langerhans cell histiocytosis may also be associated with dyslipidemia. Hyperlipidemia can also be one of the manifestations of cutaneous necrobiotic xanthogranuloma. [21,22] Blue histiocytosis is also associated with hyperlipidemia. [23]
Mechanisms involved between skin diseases and dyslipidemia
Numerous mechanisms have been proposed to explain the association between inflammation and dyslipidemia: modulation of lipoprotein lipase (LPL) enzymatic activity by anti-LPL antibodies and reduction of LPL activity due to various proinflammatory cytokines such as tumor necrosis factor TNF-α, IL-1, IL-1 -6, interferon-γ and monocyte chemoattractant protein-1. In addition, atherogenic autoantibody complexes to oxidized LDL and oxidized anticardiolipins are generated in response to oxidative anti-inflammatory effects, which increase the accumulation of LDL in endothelial walls. [24]
Psoriasis is characterized by increased immune activity of Th1 and Th17 cells. Cytokines such as TNF-α, IL-6, IL-17, IL-20, leptin, and vascular endothelial growth factor play a central role in both psoriasis and metabolic syndrome. [25] On the other hand, metabolic syndrome itself may predispose an individual to the development of psoriasis. [26,7] Lichen planus is associated with immunological abnormalities of delayed-type hypersensitivity, in which activated T cells and other inflammatory cells such as dendritic cells are the key components. [27,28] These processes may explain the association between lichen planus and dyslipidemia, and other components of the metabolic syndrome.
Dermatological drugs causing dyslipidemia
Several medications used to treat dermatological diseases can trigger or worsen dyslipidemia. [Table 2] Systemic retinoids and immunosuppressants such as cyclosporine used to treat skin diseases such as psoriasis may worsen dyslipidemia.
Table 2. Effect of drugs used in dermatology on lipid metabolism
| A drug | Effect on lipid profile |
| Systemic retinoids | Elevated levels of TG, LDL and low levels of HDL |
| Cyclosporine | Affect many aspects of lipids and their metabolism |
| Tacrolimus | Increase in TG and decrease in lipoprotein lipase |
| Steroids | Increase in HDL, TG and total cholesterol |
| Stanazol | Increase in LDL and decrease in HDL |
| Antiretroviral drugs | Increase in HDL, TG and total cholesterol |
Hypertriglyceridemia is a metabolic complication of systemic retinoid therapy that may occur in up to 17% of cases. [29] The Apo C-III gene may be a target for retinoids acting through the retinoid X receptor. Increased expression of Apo C-III may contribute to the hypertriglyceridemia and atherogenic lipoprotein profile observed after retinoid therapy. [29] Many of the existing immunosuppressive drugs, such as cyclosporine, tacrolimus and sirolimus, are associated with an increase in one or more risk factors influencing the development of atherosclerosis [30]. Cyclosporine A, an immunosuppressant that is widely used in transplant patients, is also used in dermatology, for example for psoriasis. Long-term treatment with cyclosporine is associated with hyperlipidemia and an increased risk of atherosclerosis. Importantly, hyperlipidemia normalizes after discontinuation of cyclosporine, thereby confirming its role [31]. One possible cause for hyperlipidemia is inhibition of the synthesis of bile acids from cholesterol and the transport of cholesterol into the intestine. Another reason is that cyclosporine binds to the LDL receptor, which increases LDL levels; There is a noticeable decrease in post-heparin lipolytic activity, with an increase in hepatic lipase and a decrease in LPL activity, which leads to impaired clearance of VLDL and LDL. [32,33] Binding of cyclosporine to the LDL receptor by cyclosporine-containing LDL cholesterol particles has also been proposed as a mechanism for the cellular uptake of cyclosporine. [34] Cyclosporine may have a pro-oxidant effect on LDL levels, which may increase the risk of coronary heart disease, including the accelerated development of atherosclerosis that has been observed in recipients. [35]
Tacrolimus significantly increases plasma triglyceride concentrations and decreases LPL concentrations and activity in renal transplant patients, regardless of any lipid-lowering treatment the patients received. Decreased LPL activity, partly due to decreased plasma concentrations following tacrolimus administration, may explain hypertriglyceridemia. [36] Currently, tacrolimus is used by dermatologists only as a topical agent. Its absorption from the skin is minimal; therefore, may not be an important factor in dyslipidemia.
However, with respect to other immunosuppressants such as mycophenolic acid or azathioprine used in dermatology, there is no convincing data to suggest that they cause clinically significant increases in any lipid fractions.
Steroids are also associated with dyslipidemia. Corticosteroids raise all lipoprotein levels.[37] This is due in part to the relative deficiency of adrenocorticotropic hormone (ACTH) caused by long-term steroid use. Corticosteroids are the mainstay of treatment for pemphigus and many other autoimmune and inflammatory diseases. The main explanation for the association between dyslipidemia and pemphigus is long-term treatment with corticosteroids.[18] Corticosteroid-induced dyslipidemia is likely the result of weight gain, which leads to insulin resistance, increased hepatic LDL secretion, and increased total cholesterol and triglyceride levels. [38,39,40] Studies have shown that anabolic androgenic steroids like stanazol can lead to dyslipidemia, leading to an increase in LDL and a decrease in HDL. A noticeable decrease in HDL and HDL2 cholesterol occurs due to an increase in lipase in the liver. [41,42]
Antiretroviral therapy (ART) may also contribute to dyslipidemia. However, dyslipidemia does not develop in everyone who takes these drugs, suggesting that host factors play a role. Protease inhibitors lead to atherogenic changes in their lipoprotein profile, consisting of increased TG, LDL and total cholesterol and increase the risk of coronary artery disease. [43,44] Nonnucleoside reverse transcriptase inhibitors show, in general, the best lipid profile of all ART drugs because they are associated with an increase in HDL. [44]
Biologics used in the treatment of skin diseases are also associated with dyslipidemia. TNF inhibitors used to treat psoriasis may have varying effects on lipids. Long-term infliximab therapy may be proatherogenic, whereas etanercept and adalimumab may have beneficial effects on lipids. [45]
Dermatological manifestations of dyslipidemia
Xanthomas are dermatological manifestations associated with lipid disorders. They arise as a result of the absorption of lipids by macrophages. Clinically, xanthomas are classified as tendinous, tuberous, eruptive and flat. They may be associated with familial or acquired hyperlipidemia, lipoproliferation of malignancies, or may not have an underlying disease. [46] Xanthomas can be found in ligaments and tendons, although they can also be found in the periosteum and fascia. [47] Tendon xanthomas are located along the tendons of the arms and the Achilles tendon. Tuberous xanthomas appear as yellow nodules; often associated with hypertriglyceridemia and sometimes hypercholesterolemia. [48] Flat xanthomas are patchy or slightly raised features that can occur anywhere and can involve large areas of the body. Common flat xanthomas can cover large areas of the body, including the face and neck. Xanthelasma is a flat xanthoma in the form of a yellowish plaque located on the skin of the eyelids or periorbital area. [49] The development of a xanthoma on the palmar crease is usually called striatum palmare xanthoma and is an important sign of type III hyperlipoproteinemia. [50] Eruptive xanthomas are orange-yellow papules in hyperglyceridemia and uncontrolled diabetes. [51]
Prevention of dyslipidemia
The basic principles of correction of dyslipidemia include: treatment of secondary or associated causes such as diabetes, discontinuation of offending medications (in this case, consider an alternative route of treatment or reduce the dosage, if possible). Regardless of the underlying dermatologic disease, smoking cessation and reduction of other modifiable risk factors are important aspects of coronary artery disease prevention. [1]
With steroid therapy given in the morning at a minimal dose, lifestyle changes including exercise, weight control, [52] avoidance of fatty foods, and treatment of diabetes mellitus, if present, can all help, complementing or even supplanting drug therapy. Studies related to cyclosporine dyslipidemia are probably best derived from experience and evidence in renal transplant patients. There has been conflicting data on whether dyslipidemia is dose dependent on cyclosporine and one large study did not show a relationship. [53] In addition, dermatological conditions such as psoriasis, for which cyclosporine is used, have an independent association with metabolic syndrome. Therefore, it is prudent to be more proactive in the treatment of these patients, including pharmacotherapy for dyslipidemia and dysglycemia in these patients.
Hypertriglyceridemia remains the most common lipid disorder among patients with human immunodeficiency virus (HIV). Fenofibrate is the fibrate of choice for HIV-infected patients who have hypertriglyceridemia due to the lack of serious drug interactions and evidence of better cardiovascular effects. Dual therapy with the addition of statins may be necessary if LDL is elevated. Due to the multifactorial nature of HIV infection and associated dyslipidemia, changes in treatment may not achieve the expected results. [54]
Eruptive xanthomas caused by hypertriglyceridemia respond well to lifestyle changes and lowering lipid levels with fibrates. It has been noted that eruptive xanthomas usually disappear within a few weeks after systemic treatment, tuberous xanthomas after a few months, but the disappearance of tendon xanthomas may take years or they may persist indefinitely. [55]
Lifestyle changes
Lifestyle approaches including dietary changes are the main approach to treating children and young people. Physical activity offers many benefits such as weight loss, decreased insulin resistance, decreased triglyceride levels, increased HDL, and improved cardiovascular function. Dietary approaches include: consuming low-fat and low-fat dairy products, avoiding trans fats and animal fats, using vegetable fats, limiting egg yolk intake, and avoiding meats and foods high in saturated fat (eg, liver) [56] For elevated triglycerides , you need to avoid sugar, sweetened drinks, juices and refined carbohydrates.
Drug treatment
Statins, drugs that reduce the risk of cardiovascular disease and cardiovascular mortality, have significantly replaced bile acid resin drugs due to their side effects. Statins primarily lower LDL levels. Rosuvastatin is a more powerful drug than atorvastatin or pravastatin and is also more effective at lowering triglyceride levels. Statins reduce endogenous cholesterol production by inhibiting the key enzyme 3-hydroxy-3-methylglutaryl coenzyme. They are generally well tolerated, but you need to be aware of possible adverse reactions such as liver damage, muscle cramps and rhabdomyolysis. They also cause skin side effects such as: autoimmune reactions, dry skin, severe reactions such as drug hypersensitivity syndrome (DRESS) and allergic reactions. [57] Statins should be avoided during actual or possible pregnancy, as they have a teratogenic effect. Ezetimibe may be a useful adjunct in severe cases. Fibrates are a lifeline for the treatment of hypertriglyceridemia and may be chosen over niacin, which is poorly tolerated by many patients. Omega-3 fatty acids may be used additionally or alternatively when fibrates cannot be used, for example during pregnancy.
The evidence base for pharmacological intervention for dyslipidemia in childhood is limited. Lipid-lowering therapy is intended for high-risk groups, that is, children at least 10 years of age who have an LDL level of 190 mg/dL or higher or 160 mg/dL or higher and who have other risk factors such as diabetes mellitus, etc. d.
Drugs that affect chylomicron production, such as orlistat, are also effective for patients with hypertriglyceridemia. [58]
Conclusion
Dyslipidemia in dermatoses appears to be a more common problem than expected. Many dermatoses are discussed in this article, but more diseases may be added to this list in the future. Their treatment may include lifestyle modifications and pharmacotherapy. Dietary counseling can help control underlying disease and may provide an opportunity to reduce the risk of cardiovascular and metabolic diseases. Dermatologists treating these dermatoses must have comprehensive knowledge on this issue and treat them comprehensively.