15.06.2021
Heart valve replacement surgery is a very complex process that requires close attention and high precision. Fortunately, modern medicine allows us not only to perform operations on such an important organ, but also to do it with high efficiency and minimal risk for the patient. Not only older people, but also younger people may need heart valve replacement.
Anatomy of the heart and reasons for replacing its valve
Our heart has four valves - aortic, mitral, tricuspid and pulmonary valve. They ensure the correct passage of blood through the four chambers of the heart during the heartbeat.
Disturbances in structure and, as a consequence, functioning can occur at birth, as birth defects that will affect later life. Also, destruction of valve tissue can result from certain diseases, for example, rheumatic fever or infective endocarditis.
Unfortunately, like the rest of the body, heart valves are also subject to aging. Regardless of the reason, the valve can either weaken (begin to let blood flow in the opposite direction), or vice versa - heal and become more rigid. This will cause the valve to not open completely. Incomplete, incorrect opening of the valve is called "stenosis". When the valve is weakened or stretched, it is called regurgitation or regurgitation.
4. Lifespan of heart valves
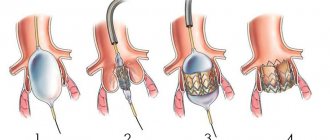
Today, two types of heart valve implants are used in heart surgery: artificial and biological.
The first ones are durable, but their installation is associated with lifelong use of a number of drugs to eliminate the risk of blood clots. Biological valves are closest to living tissues, but wear out faster. Cardiologists are constantly working to develop and introduce into medical practice new types of valves that combine the best properties of both types - durability and maximum acceptability for the body. The service life of artificial valves is 10-15 years. Newer materials are still being studied. Widespread practice of their use in the near future will provide cardiologists with more accurate information about their service life.
How is open heart valve replacement surgery performed?
If you have been scheduled for surgery on one of your heart valves, you should go to the hospital at least one day before the operation. During this time, the medical staff will carry out all the necessary procedures (CT, ECG) and collect the necessary tests. You will also have time to meet and talk with your doctor. He will tell you all the details of the upcoming operation and also answer any questions you may have.
It's normal to feel nervous before heart surgery, so don't be afraid to express your concerns to your doctor. Be sure to describe exactly what medications you take on an ongoing basis, this may be important.
About an hour before surgery you will be given the first pain medications. The operation itself is performed under general anesthesia, which guarantees deep sleep and absence of pain. As a rule, surgery lasts 3-3.5 hours.
Your relatives may be in a special room waiting for you. When the surgery is completed, the doctor will tell them the results. For all people, depending on age, body weight and gender, anesthesia takes place over different periods of time, which is usually limited to a few hours.
The first hours after heart surgery
Typically, after heart surgery, a person spends about a week in the hospital. During this time you will be in the intensive care unit (ICU). Family members will be allowed into your room approximately 60 minutes after surgery. Subsequent visits can be arranged in accordance with the rules of the medical institution.
When you wake up, you will be connected to many tubes, catheters and electrodes. Specifically, you will have a breathing tube in your mouth, which will interfere with your ability to speak. Don't worry, there will be a nurse nearby who will understand what you need.
The breathing tube will be removed a couple of hours after surgery. Also, thin tubes will be connected to your arms or neck, through which medications and nutrients will be introduced into your body. These tubes are needed to take blood samples and monitor your blood pressure. Thin wires may protrude from the chest. They are attached to the heart and, if necessary, allow you to quickly connect a temporary pacemaker. There will also be several tubes coming out of your chest that pump out fluid from the tissues surrounding the heart. A tube in the bladder is needed to remove urine, and various electrodes taped to the chest are used to monitor the heart rhythm.
After surgery, you may experience discomfort and soreness in your chest muscles where the incision was made. Don't worry, the wound is stitched up securely, there is no danger. You will be given painkillers for the first few days. As you recover, the need for them will disappear.
“Scientific medical schools are a great achievement of medicine”
B.V. Petrovsky
The progress of medical science over the past decades is inextricably linked with scientific and technological achievements, which have had a huge impact on its main directions. Being a part of clinical medicine, surgery is developing as a large complex science, based on the results of biology, physiology, biochemistry, mathematics, physics and other fundamental branches [1]. It was at the junction of many disciplines in the late 50s and early 60s of the twentieth century that a new direction arose - cardiac surgery. Developing various methods of surgical correction of congenital and acquired heart defects, cardiac surgery placed increased demands on operations, which contributed to the progress of such disciplines as anesthesiology, perfusionology, and resuscitation.
In 1958, S. Lillehei, for the first time in the world, performed implantation of a valve prosthesis into the aortic ostium in a patient with aortic heart disease under artificial circulation [1–2].
The first successful operation to replace the mitral valve (MV) with a ball prosthesis at the Russian Scientific Center for Surgery named after. acad. B.V. Petrovsky (RNTsH) was performed in November 1963 by prof. G.M. Solovyov, and already in 1966 the publishing house “Medicine” published a monograph by B.V. Petrovsky, G.M. Solovyov and V.I. Shumakov “Heart valve replacement”, in which the authors summarized the world and their own experience in heart valve replacement [2]. Since the early days of cardiac surgery, a large number of artificial heart valves (AHVs), especially leaf ones (one-, two-, three- and four-leaf) have been proposed. Another group consisted of valve-type prostheses, the most striking representative of which is the ball prosthesis. It is ball prostheses - Starr-Edwards abroad, AKCh and MKCh in the USSR - for several decades that remained the prosthesis of choice in both the aortic and mitral positions.
The development of heart surgery has developed in several directions. Firstly, the imperfection of ICS stimulated surgeons to search for and develop reconstructive valve-sparing operations. Secondly, the improvement and development of new models of mechanical prostheses and the introduction of prostheses made from biological tissues into clinical practice continued. Thirdly, methods of implanting prostheses, not only aimed at normalizing intracardiac hemodynamics, but also promoting reverse remodeling of the ventricles and improving their pumping function, have begun to play a major role in improving the results of heart valve replacement.
RSCH took an active part in the creation of the ICS: developed by Center employee V.I. Shumakov together with two groups of engineers headed by B.P. Zverev and E.A. Ivanov, ball (AKCh and MKCh) prostheses were used in our country until 1992. In just 25 years, about 55,000 AKCh and MKCh ball valves were implanted [2].
Petal prostheses, due to their low efficiency, have not found use in clinical practice. The biggest disadvantage of ball prostheses, especially for the mitral position, was their size and dimensions. With small sizes of the left ventricular (LV) cavity, low cardiac output syndrome often developed. The use of a biconvex (Hufnagel prosthesis), a convex-concave lens (Cruz-Kaster prosthesis), or a hemisphere (MKCh-27) as a locking element made it possible to reduce the weight and height of the prosthesis, but, as their clinical use has shown, it increased thrombogenicity.
Ball prostheses were replaced by prostheses with a rotating disk, which were most in demand in the 70–80s of the twentieth century. The design of the valve, in which the locking element, made in the form of a disk, rotated around an eccentric axis, opening and closing the passage hole, solved many problems, the hemodynamic characteristics also improved, and the injury to blood cells was sharply reduced. The introduction of this type of prosthesis was facilitated by the creation of isotropic pyrolytic carbon, which has unique wear resistance and biocompatibility (J. Bokros, 1966). Finally, after testing many valve designs with various combinations of materials, solving the problems of reliability and durability of prostheses led to the emergence of the “gold standard” - the Bjork-Shiley Monostrut valves and then the Medtronic-Hall valves. Since 1981, the single-leaf low-profile EMICS prosthesis for both mitral and aortic positions has become available to domestic cardiac surgeons, and since 1985, LICS-2 valves.
In 1991, the development of the MICS prosthesis appeared. Its distinctive feature is its high durability with good hemodynamic efficiency. High reliability and durability of the valve are achieved through the use of special titanium for the body and the main design feature - rotation of the locking element of the convex-concave disk in the valve body during operation, which significantly reduces the risk of wear of materials due to distributed contact of the elements [3].
The desire to achieve central blood flow in the prosthesis led to the invention of bicuspid prostheses. The first and most prominent representative of this group of prostheses is St. Jude Medical, whose first clinical implantation was performed in 1977. Its two semicircular doors open to 85°. Among the cohort of bicuspid prostheses that have found widespread use in clinical practice, it is worth noting foreign prostheses Carbomedics, ATS, On-X, and domestic ones - Carbonics, Roscardix, Medinge. In total, since the founding of the Russian Research Center for Surgery, 5362 units of prostheses have been implanted, including 4012 in the mitral position, 2265 in the aortic position, and 85 in the tricuspid position.
Reliable mechanical properties, low profile, and more favorable hydrodynamic properties of bicuspid prostheses have contributed to the displacement of rotary-disc structures. Almost central blood flow is observed in tricuspid prostheses and in the so-called bicuspid “full-flow” prostheses, but their production has not been put into production.
Positive factors include the variety of cuff types, which allows valves to be implanted in different positions relative to the fibrous ring. For example, reduced cuffs allow the implantation of larger diameter prostheses, which is especially important in aortic valve surgery.
In December 1964, academician B.V. Petrovsky was the first to perform a successful operation of mitral valve replacement with an artificial prosthesis with a device for sutureless fixation. The idea of seamless fixation is embodied in modern self-fixing prostheses.
In his monograph B.V. Petrovsky et al. [2] described the classic version of mitral valve replacement (MVR): after opening the left atrium (LA), they begin to remove the MV, trying to remove the entire MV - leaflets, chords and papillary muscles - as a single block. In this case, it is important to leave a sufficient and uniform belt of leaflet tissue at the fibrous ring with a width of 3–4 mm. It is necessary for suturing or attaching needles of the device for seamless mechanical fixation and creating a seal around the prosthesis, facilitating a more reliable sealing of the ICS attachment line. This technique was used by all cardiac surgeons in the world, which is valid to this day. The differences concerned only the suture material used and the method of fixation of the prosthesis: separate 8-shaped sutures, U-shaped sutures with or without gaskets, the location of the gaskets on the ventricular or atrial side, continuous wrapping suture. These sutures have their advantages and disadvantages, and the surgeon chooses the preferred option in each specific case.
Back in the 60s of the last century, S. Lillehei performed MV replacement operations without excision with good clinical results. At the time, this idea did not find widespread support, primarily due to the lack of low-profile prosthetics. It should also be noted that after reconstructive valve-sparing operations, immediate and long-term clinical results were significantly better than after prosthetics. This was associated primarily with the preservation of fibropapillary contact.
Anatomical studies carried out in the department of acquired heart defects showed that the trabecular apparatus, together with the papillary muscles, forms the internal frame of the heart, which changes in various diseases. Papillary muscles are a continuation of the muscle fibers of the LV, and when cut off from the chordae, the fulcrum is lost, and the entire muscle bundle falls out of the contraction process (see Fig. 1).
Rice. 1. Inner surface of the left ventricle. Circumflex artery - red marker; trunk of the left coronary artery - black marker; papillary muscles and trabecular muscle network - yellow marker.
It is well known that with an ellipsoidal shape of the LV cavity, in contrast to a spherical one, the pumping function of the heart is more effective. Taking this into account, operations have been proposed aimed at changing the shape and size of the heart when exposed to it from the outside (formation of a fold of the left ventricle of the heart, myosplinth, various types of mesh). However, practice has shown the inconsistency of these surgical interventions.
The choice of a prosthesis in the mitral position is based on the measurement of the fibrous ring. Matching the size of the fibrous ring to the seat diameter of the prosthesis provides the most favorable conditions for its fixation. Traditionally, it was believed that the larger the size of the prosthesis and, accordingly, the larger the effective opening, the better the hemodynamic parameters (systolic and mean gradients between the LA and LV). Setting the goal of changing the shape of the left ventricle of the heart, prostheses are implanted in a size that corresponds to the patient’s physiological norm. These are, as a rule, dentures of 27–29 sizes. If the seat diameter of the prosthesis is significantly smaller than the fibrous ring, the following techniques are used: U-shaped sutures with spacers are placed along the entire perimeter of the fibrous ring, placing the latter on the side of the atrium. The pitch between the seams is from 2 to 5 mm (the greater the discrepancy between the sizes of the cuff and the fibrous ring, the greater the distance between the seams), while the seams are evenly distributed on the prosthesis cuff and the prosthesis is fixed, taking into account that the seam pitch on the fibrous ring and the cuff is significant The degree varies. In order to avoid the formation of paravalvular fistulas, additional fixation of the prosthesis is performed with a wrapping suture. At the first stages, only the posterior leaflet was preserved and the operation of rapprochement of the papillary muscles was used. This is the so-called Sling, proposed in 1998 by R. Nair et al. [5]. The essence of the method is that the preserved subvalvular apparatus of the posterior leaflet becomes a support for fixing the papillary muscles of the anterior leaflet. After excision of the anterior leaflet with the chordal apparatus, a vascular prosthesis with a diameter of 4 mm is placed under the bases of the papillary muscles. Bringing the bases of the papillary muscles closer together, the prosthesis is fixed with a suture. Approaching the base of the papillary muscles can also be done using a U-shaped suture on large spacers (see Fig. 2).
Rice. 2. Stages of left ventricular remodeling surgery. a - the anterior leaflet of the mitral valve with chords has been removed, the papillary muscles are completely preserved. U-shaped sutures are placed on the fibrous ring and the posterior leaflet of the mitral valve; a massive group of papillary muscles and interpapillary chords are clearly visible; b - a suture is placed, bringing the bases of the papillary muscles closer together, the fibrous ring is prepared for implantation of the prosthesis.
Preserving the fibropapillary contact of both leaflets is a more effective operation. In addition, when the anterior leaflet moves to the posterior annulus fibrosus, the papillary muscles come closer together, and there is no need for their fixation (see Fig. 3).
Rice. 3. The severed anterior leaflet of the mitral valve is fixed to the fibrous ring of the posterior leaflet.
Comparing two groups of patients with mitral regurgitation, who respectively underwent classical prosthetics and with preservation of the fibropapillary contact, more significant positive echocardiographic indicators were achieved in patients with preserved fibropapillary contact (see table)
Comparative analysis of the main volumetric and linear parameters of the left ventricle within the study groups before and after surgery Note. MVR - mitral valve replacement; LV EDV—left ventricular end-diastolic volume; LV ESV—left ventricular end-systolic volume; HC—impact ejection; LVEF—ejection fraction; LV ESD—end systolic size of the left ventricle; LV EDR is the end diastolic size of the left ventricle. [4].
In cases where there is valve calcification, the affected areas are excised and a fibropapillary contact is formed from the remaining areas. If there is a significant deficiency of your own tissue, PTF threads can be used.
Thus, the development of surgical interventions on the MV has made it possible to significantly expand the indications for surgery, including patients with reduced contractile function of the heart, and to significantly improve functional results.
The authors declare no conflict of interest.
e-mail: moon.
Postoperative period
After 1-2 days, depending on how the recovery goes, you will be able to sit up in bed. Then get up and move short distances with the help of others. After a few days you will be able to wash yourself, but under the supervision of a nurse. Once the air tube is removed, you can drink. You may not have an appetite, but adequate nutrition is essential for a speedy recovery. Your doctor will tell you when you can switch from liquid to solid foods.
Every day you will get better and better, however, fatigue and emotional downturns are possible. These are normal consequences of the operation. When the doctor is completely sure that you have recovered sufficiently, you will be discharged from the hospital to go home. It is advisable for one of your relatives to meet you and take you. As a last resort, take a taxi. Taking public transport or driving a week after open heart surgery is not a good idea. Please note that during the first days you should be under the supervision of loved ones or a caregiver.
Visit to a cardiologist
Valve replacement improves heart function, but requires lifestyle changes and constant monitoring of coagulation levels. The first visit to the cardiologist is a month after the operation. Necessary:
- take a blood test;
- urine;
- take an ECG.
If the results are good, the next visit is made in a year. You need to focus on how you feel; you may need to consult a doctor more often. If the monthly PTI analysis is unsatisfactory, there are deviations up or down, only a cardiologist can make an adjustment.
Recovery after heart surgery
When you find yourself at home, try to quickly return to your usual sleep and wakefulness routine. It is advisable to find time for a short nap after lunch. You should weigh yourself regularly for several weeks and record your weight. You most likely lost weight while you were in the hospital. You will gain weight, but be sure to tell your doctor if you are gaining weight quickly. Accelerated weight gain may indicate that fluid is accumulating in the body, and this is dangerous!
The rest is normal rehabilitation. If your doctor allows it, take short walks, preferably accompanied by loved ones or a caregiver. You can also do low-intensity exercise on an exercise bike. Try to do a little more every day than you did yesterday. However, don't overdo it. If you are tired, rest, if you are rested, exercise.
Within six months you will feel better almost every day. Regarding daily activities, you should not lift or move objects weighing more than 2.5 kg. You can do simple housework, go to the movies, cafes, and attend social events. If you drive a car, you can move around in it. It will be useful to climb the stairs, but you need to start small, preferably under the supervision of loved ones.
Nutrition and medications during the rehabilitation period after heart surgery
During your stay at the facility, you will be given detailed information about the diet you will be following. In short, nutrition should be healthy. Most likely, you should limit salt, sugar, and try to reduce the amount of trans fats and saturated fatty acids.
In addition, you will have to change your drug therapy. You should only take medications that your doctor prescribes. Without consulting a specialist, do not take medications that were taken before surgery. If you have been prescribed anticoagulants, then approach this very responsibly. Don’t miss a dose, and if you still couldn’t drink it on time, consult your doctor. No need to take a double dose next time!