The aorta is the largest unpaired arterial vessel of the systemic circulation, coming from the heart and feeding all internal organs and systems, except the lungs. Throughout its entire length, the aorta has a uniform thickness and the same structure. Under the influence of unfavorable exogenous and endogenous factors, its structure is disrupted: atherosclerotic plaques or fibrous growths appear on the walls, disrupting normal blood flow.
Aortic compaction can be detected using various diagnostic methods: radiographic, fluorographic or ultrasound examination. Having discovered such a defect, specialists must find the main causes of the pathology and prescribe the correct treatment. Otherwise, the disease can lead to serious consequences: dissection of the aortic walls and rupture of the blood vessel. These complications are accompanied by large blood loss and often result in the death of the patient.
Depending on the location of the lesion, the following forms of pathology are distinguished:
- Compaction of the aortic root,
- Consolidation of the aortic arch,
- Consolidation of the ascending aorta,
- Consolidation of the descending aorta.
Causes
Arterial hypertension
Chronic increase in pressure leads to loss of elasticity of the vascular walls. Compensatoryly, the vascular endothelium becomes rigid and thickens due to fibrous growths.
Aortocardiosclerosis
Provoking environmental factors (poor nutrition, obesity, physical inactivity) lead to an increase in cholesterol levels in the blood. It can deposit on the wall of the aorta and heart valves. Over time, portal plaques thicken and significantly narrow the space for blood circulation.
Atherosclerosis is one of the main causes of thickening of the aortic walls
Rheumatism
Acute rheumatic fever has many manifestations, one of which is bacterial carditis and valvulitis with subsequent thickening of the mitral or aortic valve.
Endocarditis and myocarditis
Inflammation of the muscular or inner epithelial layer of the heart also leads to scarring at the level of the valves and aortic ring.
The cause of fibrosis and how to diagnose it
An important role in the functioning of the valvular apparatus of the heart is played by the valves, which are represented by loose connective tissue consisting of dense collagen and continuously extending into the chordae tendineae (according to Wikipedia).
Under a number of circumstances, the number of blood vessels supplying the structure of the valves is reduced. As a result, elastic fibers are replaced by dense fibrous tissue, which is characterized by sufficient strength. Having lost lability, the valves lose the ability to provide physiological hemodynamics. Most often, the mitral valve is affected by pathology, less often – the aortic valve. Classification of pathology:
- focal. There is moderate damage to the structure of the valve apparatus;
- diffuse. The affected area covers the leaflets and subvalvular space;
- cystic. It is characteristic of an advanced stage and is considered a separate pathology with the formation of cavity formations.
Fibrosis of the aortic and mitral valve leaflets is explained by the following reasons:
- age-related changes with loss of natural collagen potential;
- rheumatic attack (especially repeated), for example, after oropharyngeal infections. The damage is attributed to antibody formation and cross-reactivity between group A streptococcal carbohydrates and heart valve glycoprotein. According to research, almost every five-year-old child has a history of a throat infection. It is possible to develop chronic rheumatic heart disease with damage in the form of post-inflammatory marginal fibrosis;
- Marfan syndrome, dysplasia, in which the anatomical and functional features of the connective tissue are genetically abnormal;
- atherosclerosis of the aorta. Calcification of plaques and subsequent thickening of its wall;
- foci of necrosis (with a heart attack) or inflammation (with myocarditis) near the valve ring.
Diagnosing fibrosis is not very difficult. Initially, clinical blood and urine tests are prescribed to detect the possible presence of inflammation. Biochemical research indicates changes in the levels of cholesterol, sugar, uric acid, total protein, and creatinine.
Ultrasound of the heart reveals the degree of narrowing, valve insufficiency, evaluates the contractile function of the myocardium, blood volume during systole.
X-ray examination reveals myocardial hypertrophy, pulmonary congestion, and calcification of valve fragments.
CT, MRI, CAG are performed if surgical intervention for prosthetic structures is necessary.
Symptoms
Narrowing of the lumen between the left ventricle and the aorta leads to the following clinical picture:
- attacks of dizziness, even fainting, associated with minor physical activity;
- shortness of breath, attacks of suffocation;
- fast fatiguability,
- attacks of angina pectoris (pain behind the sternum of aching or burning nature).
Hardening of the aorta often causes angina attacks
For a long time, aortic stenosis is asymptomatic; severe symptoms appear when the opening narrows by more than 70%.
Symptoms of the disease are associated with the localization of the pathological process:
- when the lumen of the aortic root narrows, insufficient blood supply to the heart muscle occurs, this is manifested by the development of typical angina pectoris, including acute myocardial infarction;
- if the ascending part and arch of the aorta are compacted, neurological symptoms appear (headache, dizziness, weakness, fatigue, etc.);
- thickening of the descending aorta leads to malnutrition of the lower body and the development of intermittent claudication, acute abdominal pain, etc.
Diagnostics
If one or more of the complaints listed above occur, you should consult a doctor for further examination.
Visual inspection
During inspection, pay attention to the following:
- characteristic pallor (also called “aortic”): due to a decrease in cardiac output, peripheral capillaries narrow to redistribute blood to the central channel;
- shortness of breath with minimal physical activity – with severe disruption of blood flow;
- acrocyanosis (blueness of the tip of the nose, lips) - not always;
- rarely swelling of the lower extremities.
Physical examination methods
Additionally, the doctor assesses the state of the cardiovascular system using the following diagnostic measures:
- palpation – intensification and displacement of the apex impulse down and to the left (V-Vl intercostal space along the midclavicular line);
- percussion – displacement of the relative dullness of the heart to the left;
- Auscultation – the appearance of a rough noise in the systole phase, weakening of the ll tone over the aorta, moist rales are possible over the surface of the lungs due to left ventricular failure;
- blood pressure measurement - hypotension.
Instrumental diagnostic methods
Additional examination methods are used:
- R-graph – an increase in the size of the heart due to its left parts, expansion of the aortic root;
- electrocardiography – deviation of the electrical axis to the left;
- echocardiography (this examination is also called ultrasound of the heart) - an increase in the thickness of the vascular wall, marginal compaction of the aortic valve leaflets, possible regurgitation (the flow of blood splashed into the aorta back into the heart). EchoCG allows you to assess the degree of destructive changes.
Ultrasound is a modern and highly informative method for studying the heart and large vessels
Aortic valve defects in adults: modern pathology and indications for surgery
S.L. Dzemeshkevich
Dr. honey. Sciences, Professor, Cardiac Surgeon, Department of Cardiovascular Surgery, RKNPK
In developed countries, calcified aortic disease is the third most common nosological form after arterial hypertension and coronary heart disease [1].
Knowledge of the etiology of the process that led to aortic disease can significantly influence both surgical tactics and the postoperative treatment protocol for patients and, ultimately, the long-term prognosis. Therefore, at all stages of treatment, one should strive to answer the question of the etiology of the primary process that caused valve dysfunction. Sometimes this answer can only be given by a surgeon who visually assesses the nature of the valve damage already during surgery. In any case, elucidation of the etiology, even with a presumptive conclusion, is extremely important.
Etiology
Assessing our own experience and published data from colleagues from other Russian clinics, it is necessary to emphasize that even today aortic malformations of rheumatic etiology dominate in cardiac surgery hospitals, although not as clearly as in the statistics half a century ago. This figure does not exceed 30-40%. However, if we take into account that only during the period from 1993 to 1998 in Russia the frequency of the cardiac form of rheumatism increased 7 times [2], then in the future we should again expect an increase in the number of patients with rheumatic valve defects.
The increase in surgical interventions on the aortic valve in the group of patients over 60 years of age has significantly increased the number of atherosclerotic “degenerative” (age-related) aortic valve defects. If aortic disease is moderately expressed and combined with widespread atherosclerosis of the coronary arteries, aorta and its branches in combination with distinct specific disorders in lipid metabolism (total cholesterol, low-density lipoproteins, triglycerides), then the atherosclerotic origin of the process on the valve is beyond doubt. This is a special and prognostically most severe group of patients. It is to this category of patients that the point of view of some authors extends that aortic stenosis is a special form of manifestation of atherosclerosis with risk factors identical to this systemic disease.
In a real clinical situation, no more than 50% of elderly patients with signs of aortic stenosis have changes in the coronary vessels [3-5]. Such patients have another degenerative process in the valve with a reduced level of metabolic reactions due to age-related changes: atherosclerosis as such can only play the role of an accelerating factor, especially if it is accompanied by inflammatory changes in the aortic valve leaflets, specific to many atheromas, due to the invasion of Chlamydia pneumoniae [6, 7 ]. Age-related involutional calcium degeneration is, in our opinion, the most appropriate definition for this pathology of the aortic valve. As a special form, it is often found in elderly patients and, as a rule, when analyzed, falls into the group of atherosclerotic defects. The diagnostic line between these two groups of patients (atherosclerosis and age-related dystrophy) is very thin, but it is quite possible to draw it with a certain amount of experience. The practical significance of such a diagnosis can be expressed not only in a different prognosis, but also in the amount of drug therapy after surgery (use of antiplatelet agents, lipid-lowering drugs).
The same type of “degenerative” defects with severe calcification includes a group of patients with a congenital bicuspid aortic valve configuration. This was unexpected for us, but the number of such patients increases as the number of elderly patients operated on increases.
Actually, the three main causes of aortic heart defects that we have already noted together account for at least 90% of the causes of aortic valve stenosis [5, 8-13]. All these reasons lead to different pathomorphological, but similar functional changes in the aortic valve leaflets, limiting their mobility. This process (fibrosis, thickening, formation of adhesions in the commissure area, calcification) always takes a long time - years, or even decades. Other, more rare causes of aortic stenosis include previous and active infective endocarditis, systemic lupus erythematosus (verrucous aseptic endocarditis of Libman-Sachs), hereditary metabolic disorders such as homozygous hyperlipoproteinemia type II and alkaptonuria (ochronosis), metastatic calcification of the aortic valve in patients with chronic renal failure [14-16].
Pure or dominant aortic insufficiency is much less common than stenosis. With combined lesions, the most common cause is rheumatic valvulitis, which leads to wrinkling and shortening of the aortic valve leaflets. Infectious endocarditis plays a significant role, forming aortic insufficiency either on the native valve or by altering the natural history of such anomalies as a bicuspid or prolapsed aortic valve. And yet, despite the fact that rheumatism is the most common cause of aortic insufficiency and in this nosology is not an absolutely dominant process, other causes of aortic insufficiency in the aggregate are much more diverse than with aortic stenosis. All this diversity can be divided into three pathomorphological groups:
• aortic insufficiency with changes only in the semilunar cusps (rheumatism, infective endocarditis, bicuspid valve, cusp prolapse);
• aortic insufficiency as a result of pathology of the ascending aorta with anatomically unchanged leaflets (Marfan syndrome, Ehlers-Danlos syndrome, syphilitic aortitis, ankylosing spondylitis, dissecting aneurysm of the ascending aorta);
• aortic insufficiency with anatomically preserved aorta and aortic cusps (secondary prolapse with a ventricular septal defect, hypertension).
Indications for surgery
The symptom complexes characteristic of a particular valve defect determine modern treatment tactics to a much greater extent than the actual nature of the damage to the aortic valves. Therefore, any attempt to identify a diagnosis of the condition, justify indications for surgical intervention and surgical tactics only on topical diagnostic data (orifice diameter, the amount of valve prolapse, the amount of pressure drop across the valve, the presence or absence of signs of calcification, etc.) does not indicate the benefit of a comprehensive clinical analysis of the condition of a particular patient.
Cardiologists today reliably diagnose this pathology and promptly send such patients to cardiac surgeons. And yet, when deciding on surgery in patients over 70 years of age, we sometimes encounter some resistance from our fellow cardiologists. Their doubts are based on both an objective factor - the higher risk of surgery, and a subjective one - the unknown of the individually “programmed” life expectancy of such elderly patients.
Therefore, in this publication we specifically report data from O'Keefe et al., [17] who were able to follow a group of 50 patients awaiting balloon dilatation of a stenotic aortic valve. The average age of patients exceeded 70 years, survival without surgery by the 3rd year of observation was only 25%. At the same time, in the randomized group of patients without aortic pathology, the survival rate was 77%. Considering that today mortality in aortic replacement is minimal, then these data should convincingly prove to cardiologists the need for surgical treatment of such patients.
In classic situations, the question “when to operate?” does not present any difficulties: digital radiography from the screen of an electron-optical converter, ECG, echocardiography, MRI with contrast are sufficient methods for making a topical diagnosis and assessing the condition of the left ventricle of the heart. Performing sounding of the heart cavities in patients with aortic defects in order to determine the pressure drop, the volume of regurgitation, end-diastolic pressure in the left ventricle or pulmonary capillary wedge pressure today can already be regarded as a diagnostic anachronism.
In our practice, we are naturally especially wary of choosing a solution in patients with “minor” symptoms and, even more so, in asymptomatic patients. It is known that clinical manifestations and complaints may be absent even with severe severe aortic stenosis with an orifice area of less than 0.8 cm3 and with a decrease in the ejection fraction to 25-30% [18].
Enlargement of the left ventricle of the heart to 6 cm or more (in patients with aortic insufficiency), as well as hypertrophy with overload of the left ventricle (in patients with aortic stenosis), are sufficient instrumental criteria for the need for surgery in the presence of a topical diagnosis.
Doppler echocardiography makes it possible to determine the magnitude of the pressure drop with almost the same accuracy as probing of the left ventricle. Understanding the conventions and multifactorial dependence of this indicator, we consider its value to be 40-50 mm Hg. Art. sufficient grounds for a more detailed examination of the patient and search for arguments in favor of surgery.
Calculation of the size of the effective opening is less dependent on the characteristics of blood flow through the section “left ventricle-aortic valve-ascending aorta”, but this indicator is quite conditional and “semi-quantitative”. And yet, we definitely take into account the instructions of ultrasound diagnostic specialists to limit the opening of the valve leaflets to less than 1.5 cm, and when the opening size is less than 1 cm, the indications for surgery are almost absolute. An even more accurate expression of the degree of stenosis is the ratio of the size of the stenosis to the total body surface area - a value of less than 0.6 cm/m2 is critical [19]. If there is information about valve calcification, then you should not postpone the operation, since progression of the process is inevitable.
If the arguments in favor of the operation are not absolute, then for aortic stenosis we calculate the pressure loss across the valve (mm Hg/ml stroke volume) - the value is 1 mm Hg. Art./ml and more significant and weighty. If necessary, repeat these calculations under load. In aortic insufficiency, a decrease in the ejection fraction of less than 55% and its further decrease (or unchanged) under stress test conditions also indicate the limit of compensatory reserves of the left ventricular myocardium and serve as a more than convincing criterion in favor of surgery.
In the presence of concomitant coronary pathology requiring surgical correction, or concomitant mitral valve defects, the criteria for revision and intervention on the aortic valve can be much more liberal and are often determined by the individual decision of the operating surgeon.
It should be remembered that aortic stenosis progresses regardless of any patterns. However, with degenerative defects this process occurs faster than with rheumatic defects or in the presence of a bicuspid valve. With slow progression, the opening of the aortic valve narrows by 0.02 cm2 per year, and with rapid progression - more than 0.3 cm2 per year. When the peak velocity of blood flow through the valve reaches about 4 m/s, the two-year survival rate without surgery is only 21%. Thus, calcification, the rapid progression of stenosis over the course of a year and positive stress tests (a slight increase or even a decrease in blood pressure during exercise) are real factors for deciding on surgery for asymptomatic aortic stenosis.
In asymptomatic aortic insufficiency, the prognosis is based on assessment of left ventricular function and the degree of dilatation of the ascending aorta. Threatening signs are an increase in end-diastolic pressure of the left ventricle more than 70 mm, end-systolic pressure more than 50 mm (index more than 25 mm/m2 of the patient’s body surface), a decrease in the ejection fraction to 50%. If the ascending aorta is dilated more than 55 mm, surgery should be offered regardless of the degree of aortic regurgitation and left ventricular function. In patients with a bicuspid valve or Marfan syndrome, the indications for surgery are even more stringent - the threshold for making a decision is the diameter of the ascending aorta is 50 mm.
Continuous planned monitoring of the condition is necessary for all patients with symptoms of aortic disease and is mandatory every 12 months so as not to miss the time for possible surgical interventions.
Bibliography
1. Jund B. et al. //Eur. Heart J. 2002. V. 23. P. 1253.
2. Diseases of the heart and blood vessels // Pathological anatomy / Ed. Paltse-va M.A., Anichkova N.M. T. 2.Ch. 1. Ch. 11. M., 2001. P. 8.
3. Lindroos M. et al. //J. Amer. Coll. Cardiol. 1993. V. 21. P. 1220.
4. Iivanainen AM et al. // Amer. J. Cardiol. 1996. V. 78. P. 97.
5. Stewart BF et al. //J. Amer. Coll. Cardiol. 1997. V. 29. P. 630.
6. Nystrom-Rosander C et al. // Scand. J. Infect. Dis. 1997. V. 29. P. 361.
7. Juvonen J. et al. // J. Amer. Coll. Cardiol. 1997. V. 29. P. 1054.
8. Passik CS et al. // Mayo Clin. Proc. 1987. V. 62. P. 119.
9. Davies MI Butterworths. L., 1980.
10. Subramanian R. et al. // Mayo Clin. Proc. 1984. V. 59. P. 683.
11. Subramanian R. et al. // Mayo Clin. Proc. 1985. V. 60. P. 247.
12. Peterson MD et al. //Arch. Pathol. Lab. Med. 1985. V. 109. P. 829.
13. David TE//J. Heart Valve Dis. 1999. V. 8. P. 495.
14. Roberts WC et al. // Amer. J. Cardiol. 1973. V. 31. P. 557.
15. Roberts WC et al. // Circulation. 1967. V. 36. P. 449.
16. Pritzker MR et al. //Ann. Intern. Med. 1980. V. 93. P. 434.
17. O'Keefe JH et al. // Mayo Clin. Proc. 1987. V. 62. P. 986.
18. Corabello B. // J. Heart Valve Dis. 1995. V. 4. Suppl. 11. P. 132.
19. Rahimtoola SH //J. Amer. Coll. Cardiol. 1989. V. 14. P. 1.
The article was published in Atmosfera magazine. Cardiology
Treatment
Treatment of the disease is aimed at eliminating its cause, if possible, and correcting hemodynamic disturbances.
If the thickening of the artery walls was caused by increased pressure, drug correction of blood pressure numbers is prescribed. In case of decompensation and development of heart failure, it is supported by the prescription of diuretics and cardiac glycosides. Atherosclerosis and blood cholesterol levels are regulated by prescribing antilipidemic drugs (statins, fibrates), as well as by normalizing nutrition and a healthy lifestyle.
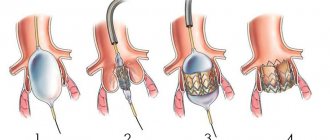
If the narrowing of the valve is significant, surgical correction of the condition is resorted to. In this case, treatment is aimed at restoring blood flow from the left ventricle of the heart to the aorta. A valvuloplasty operation is performed - the aortic valve expands, its valves are adjusted to a normal diameter. In case of severe aortic stenosis at any level, stenting is performed - surgical delivery of a special metal frame for further expansion of the vessel cavity.
Treatment and observation of a patient with fibrosis of the valve apparatus
Often on forums you can read the question of whether fibrosis can be treated using folk remedies. The answer is clear: there are no such recipes. This process is quite difficult in therapy even for modern medicine.
It is important to know that the prescription of medications is indicated only for the clinical picture of heart failure, in which the following are used:
- cardiac glycosides - Celanide, Digoxin, Strophanthin;
- diuretics - Trifas, Indap, Veroshpiron;
- if indicated, antihypertensive and antiarrhythmic drugs.
Medicines only minimize the symptoms caused by fibrosis without affecting the progression of the disease.
Radical treatment consists of the following methods:
valve prosthetics to replace the diseased structure with a mechanical or biological analogue. As a rule, a median sternotomy using a heart-lung machine is used;- mitral commissurotomy, closed or open, with the task of dissecting pathological connections between the valve leaflets;
- coronary artery bypass grafting;
- endovascular prosthetics. The essence of the method is to insert a catheter with an implant through the femoral vessels without general anesthesia. Indicated for patients with severe chronic diseases;
- valve transplantation (a relatively new technique).
Indications for surgical intervention in fibrosis:
- neglect of the process;
- wrinkling of valves, tendon threads;
- the presence of pronounced calcification.
After the operation, the patient should be under medical supervision of a cardiologist. The patient is indicated for annual examinations and treatment in a cardio- or cardio-rheumatological sanatorium.