The term “hypoxia” refers to any oxygen deficiency in tissues and organs. Various reasons cause a decrease in oxygen content, and without it, the body's cells are not able to produce energy for their existence and die.
Some vital organs have an anaerobic (oxygen-free) method of “producing” energy, but it does not meet the full consumption requirements. If this process is not intervened with treatment, a stage of irreversible necrotic changes will occur.
Myocardial hypoxia is a pathological state of “hunger” of the heart muscle. It is possible in two forms:
- local hypoxia - when only the myocardium lacks oxygen;
- as a particular manifestation of general deficiency in the body.
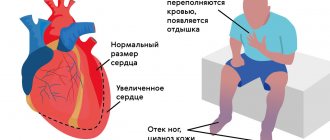
Diseases of the heart muscle reduce its strength, disrupt blood delivery to tissues and transfer pathology from the local to the general level.
Why does hypoxia occur?
The myocardium suffers from oxygen deficiency for the following reasons:
- insufficient oxygen concentration in the environment - occurs in a stuffy room, in a smoky environment, in mountainous areas, in scuba cylinders during underwater travel;
- impaired adaptive reaction - in stressful situations, increased physical activity, the heart requires more oxygen;
- disruption of the proper functioning of the respiratory system - bronchospasm, insufficient area of lung tissue to exchange carbon dioxide for oxygen (with bronchial asthma, emphysema, pneumonia, pulmonary artery thrombosis, respiratory tuberculosis);
- disturbances in the number of red blood cells, a decrease in hemoglobin levels leads to a decrease in the binding of oxygen molecules and its delivery (anemia, severe stage of erythremia, leukemia);
- the effect of poisons, intoxication - cause blocking of enzymes involved in the processes of assimilation of energy-producing substances;
- circulatory hypoxia - for diseases of the heart and blood vessels that cause a decrease in systolic blood output due to myocardial weakness (acute infarction, cardiopathy, ischemia, heart failure due to defects).
X-ray of the lungs of a patient with tuberculosis: dark spots on the left and right indicate the absence of normal lung tissue
In most cases, patients have a mixed form; 2 or more factors are involved in the disease.
In the occurrence of myocardial hypoxia, the main “culprit” is most often a disruption of the neurohumoral regulation of cardiac activity. Changes in the medulla oblongata or hypothalamus, where the control centers of the cardiovascular system are located, should compensate for the needs of the heart muscle. Violation of this connection is fraught with manifestations of energy hunger.
Causes
- Cardiac ischemia. A common cause of cardiac hypoxia. An atherosclerotic plaque appears in the walls of the heart vessels, which partially or completely blocks the lumen of the arteries. The organ does not receive oxygen and nutrition, which leads to hypoxia.
- Thrombus. Formed when atherosclerotic plaques rupture. They block the artery and lead to sudden and severe ischemia of the muscle, threatening a heart attack. Less commonly, a blood clot enters the heart from other organs.
- Spasm of the arteries of the heart. Temporary contraction of the muscles in the wall of the vessel slightly reduces or blocks the flow of blood to the organ. This is a rarer cause of ischemia.
A person experiences unpleasant manifestations of hypoxia when:
- severe emotional stress;
- inadequate physical activity;
- cold ambient temperature.
I had to examine patients who complained of chest pain when going outside in winter, at a temperature of -20ºC.
It is important to know the possible causes of hypoxia in order to avoid the occurrence of severe heart pathologies.
Clinical manifestations
Symptoms of myocardial hypoxia can develop suddenly (acute form) or increase gradually (chronic). The rate of increase in signs of oxygen “hunger” depends on the intensity of the damage factor and the individual characteristics of the body, the ability to accumulate and store energy resources and protect itself.
The acute form can be fatal without treatment within minutes or hours. The chronic process goes on for years. At the same time, symptoms of brain failure appear. Some researchers identify a subacute form, lasting several tens of hours. There are no exact dividing criteria.
For the purpose of constant monitoring, electrodes are applied to a patient with an acute infarction; the information is sent to the staff’s workplace, accompanied by an audible alarm, which allows for a quick response in case of rhythm disruption
Moderate hypoxia is characterized by:
- tachycardia, group extrasystoles, attacks of paroxysmal rhythm disturbances, this is caused by an increase in heart rate to compensate for the blood supply to the internal organs;
- shortness of breath is a physiological mechanism for increasing the ventilatory capacity of the lungs;
- blue lips and fingers;
- pain in the heart area such as angina attacks.
When measuring blood pressure, elevated numbers are possible.
The fulminant form, for example, caused by cardiogenic shock, quickly leads to increasing cardiac weakness and a drop in blood pressure. Arrhythmias are life-threatening - ventricular fibrillation, paroxysmal atrial fibrillation.
Oxygen starvation
When acute oxygen deficiency occurs, excitation of the nervous system often develops, followed by inhibition and increasing depression of its functions. Excitement is accompanied by motor restlessness, euphoria, increased heart rate and breathing, pallor of the skin, and the appearance of cold sweat on the face and limbs. Following a more or less long period of excitement (and often without it), phenomena of depression develop with the appearance of darkening in the eyes (after the previous “flickering” before the eyes), dizziness, drowsiness, general lethargy, stupor, with a gradual depression of consciousness.
Disinhibition and inductive enhancement of the activity of subcortical formations are accompanied by erratic motor activity, convulsive muscle contractions, general tonic and clonic convulsions. This period is usually short-lived. Further spread of inhibition is accompanied by a change in unconditioned reflexes: first, cutaneous reflexes (abdominal, plantar, cremasteric) fall out, then periosteal (carpal-radial, superciliary) and, finally, tendon reflexes, which at first sharply intensify and then fade away, usually first on the upper, and then on the lower extremities. Next, the pupillary and corneal reflexes disappear. However, the sequence of disappearance of reflexes is not always the same; There are cases of long-term preservation of individual reflexes in the absence of others. Movement disorders are characterized by the development of spastic paralysis with increased muscle tone, reflexes, the appearance of pathological and protective reflexes, and then muscle tone decreases, reflexes fade. With the rapid development of deep oxygen starvation, loss of consciousness occurs within a few tens of seconds, and after 1-2 minutes coma develops. Due to brain hypoxia, the following neurological syndromes can develop.
• Comatose states (depending on the prevalence of depression of brain functions and the level of regulation of remaining functions):
a) state of decortication (subcortical coma); b) anterior brainstem (diencephalic-mesencephalic), or “hyperactive” coma;
c) posterior trunk, or “flaccid” coma; d) terminal (transcendental) coma.
• Conditions of partial impairment of consciousness: a) stupor; b) stunning; c) somnolence.
• Syndromes of diffuse organic damage: a) severe posthypoxic encephalopathy (with mnestic, visual, cerebellar, striatal disorders); b) moderately severe posthypoxic encephalopathy.
• Asthenic conditions (posthypoxic asthenia with symptoms of hypo- and hypersthenia). The listed syndromes may be phases of manifestation of the consequences of brain hypoxia.
The most severe degree of comatose state (exorbitant coma) is based on depression of the functions of the central nervous system, clinically manifested by areflexia, muscle hypotonia, lack of electrical activity of the brain (“silence”), and breathing disorders. The activity of the heart and the automatic activity of other organs are preserved due to peripheral autonomic regulation.
When the functions of the caudal sections of the trunk are restored, spontaneous breathing is resumed (sometimes disturbances in its rhythm are noted), corneal reflexes are evoked - this is a “flaccid” or post-trunk coma. Further restoration of the functions of the anterior parts of the trunk can manifest itself as mesencephalic and diencephalic symptoms in the form of tonic convulsions, shudders, pronounced vegetative symptoms - hyperthermia, migratory hyperemia, hyperhidrosis, sharp fluctuations in blood pressure. Such a coma is defined as “hyperactive”, or anterior truncal.
Partial restoration of the functions of the subcortical nodes is associated with the features of subcortical coma, or the state of decortication. Its clinical picture is characterized by pronounced symptoms of oral automatism (sometimes sucking and chewing movements), increased activity of subcortical reflex levels - stem, spinal, peripheral, autonomic. Tendon reflexes are increased, skin reflexes are depressed, foot and wrist pathological reflexes are evoked. The phenomena of irritation are manifested by choreiform and athetoid hyperkinesis, myoclonic twitching in individual muscle groups. The EEG reveals diffuse slow waves.
As consciousness is restored, patients develop a state of stupor. A deeper stupor is defined as stupor; mild degrees of stupor are gradually replaced by somnolence, which corresponds to the restoration of the functions of the cerebral cortex. In this case, signs of recovery are combined with symptoms of loss and irritation. The clinical features are largely determined by the state of the limbic-reticular complex.
In soporotic states there are only the most elementary reactions to external stimuli. The EEG is usually dominated by slow waves. Stunning is accompanied by difficulty for the patient to understand complex phrases, limited ability of voluntary movements, and difficulty memorizing. Patients usually lie motionless. Against the background of stunning, dream-like (oneiric) states sometimes occur. In doubtful states, patients can be easily brought out of a drowsy state; they answer questions adequately, but get tired extremely quickly. Against the background of a state of stunning, mnestic, gnostic, praxic disorders, symptoms of damage to the cerebellum and extrapyramidal system, as well as other organic symptoms are revealed. Such disorders are defined as posthypoxic encephalopathy, which is characterized mainly by pronounced disorders of consciousness, memory, agnosia, apraxia, speech disorders (in the form of aphasia, dysarthria or mutism), cerebellar symptoms, striatal hyperkinesis, diffuse focal organic symptoms. Subsequently, with the restoration of functions (sometimes far from complete), neurasthenia-like symptoms characteristic of posthypoxic asthenia persist for a long time. These conditions are based on a weakening of the inhibitory process with the development of irritable weakness, increased excitability, insomnia, decreased attention and memory (hypersthenic form) or a weakening of both inhibitory and excitatory processes, accompanied by lethargy, drowsiness, and general retardation (hyposthenic form).
Features of chronic hypoxia
The chronic form of myocardial oxygen deficiency develops gradually and depends on:
- the predominant mechanism of pathology development;
- degree of severity and duration of hypoxia;
- environmental conditions in which the patient lives;
- individual sensitivity of a person to lack of energy.
A person with a well-developed immune system is characterized by a high level of metabolic processes in tissues, so adaptive mechanisms remain and work for a long time.
Diagnostics
Myocardial hypoxia in the initial stage is detected:
- according to the composition of blood elements, there is a compensatory increase in the release of red blood cells into the peripheral blood, and accordingly, the level of hemoglobin increases;
- when the functioning of other organs, primarily liver cells, decreases, which affects changes in biochemical tests;
- when determining oxygen in tissues - less than 95% of the normal level.
In case of toxic damage, harmful chemicals (salts of heavy metals, lead, poisons) can be identified.
The further course of the disease leads to:
- a change in the balance to the acidic side (blood pH indicates acidosis) due to the accumulation of toxins and lactic acid;
- increasing the concentration of carbon dioxide in the blood;
- reducing oxygen saturation levels to 60 – 80%.
What is needed for treatment?
Treatment of hypoxia requires eliminating the main factors of the disease:
- it is necessary to saturate the air mixture with oxygen through inhalation; in a serious condition, transfer the patient to artificial ventilation;
- for anemia - transfusion of blood components, administration of iron supplements;
- use of antidotes for poisoning with toxic substances;
- elimination of bronchospasm and therapy of lung diseases;
- removal of accumulated toxins, restoration of normal acid-base balance;
- improving contractility of the heart muscle, eliminating signs of heart failure;
- normalization of blood circulation in arteries and veins, eliminating stagnation and mechanical obstacles;
- improving the rheological (viscosity) properties of blood.
The patient breathes the oxygen mixture supplied by the device through a mask; the doctor can change the oxygen concentration
Kinds
- Ischemic hypoxia (cardiac) – caused by a decrease or disruption of blood flow in the arteries.
- Systemic hypoxia (cardiac) occurs when the body does not receive enough oxygen. For example, in case of obstruction of the respiratory tract or in high altitude conditions.
- Anemic hypoxia is an option when there is enough oxygen, but the ability of the blood to carry it is reduced. For example, with iron deficiency anemia. In such situations, no special treatment for hypoxia is required, in addition to correcting iron levels with the necessary drugs.
- Histotoxic hypoxia is an option when, with normal blood oxygen levels and the intact ability of hemoglobin to carry it, the functions of cardiac muscle cells are impaired and oxygen is not used. For example, in case of potassium cyanide poisoning.
How to saturate the myocardium with oxygen
Chronic patients are advised to spend more time in the fresh air. Walking in parks and squares allows you to breathe cleaner air and increase lung ventilation.
In case of exacerbation, it is recommended to limit motor activity.
In the diet, it is necessary to exclude foods that require oxidation and are difficult to digest (meat, fried and smoked foods, any fats). It is recommended to predominantly eat vegetable dishes and increase the proportion of salads and fresh fruits in the diet. Beets, carrots, dill, onions, and garlic are antihypoxic agents.
Medicines that increase myocardial resistance to oxygen deficiency are called antihypoxants. They are divided into 3 groups:
- having a wide spectrum of action (direct);
- indirect influence;
- mixed.
Group 1
Direct-acting antihypoxants stimulate energy processes in the tissues of the heart muscle due to:
- restoring aerobic and enhancing anaerobic methods of obtaining energy through activation of the respiratory enzymes cytochrome C, ubiquinone;
- disposal of accumulated waste and acid residues;
- reducing the impact of free oxidizing radicals;
- protection of coronary vessels;
- relieving myocardial ischemia;
- existing antiarrhythmic properties;
- restoration of connections with the centers of the brain.
The group includes the following drugs:
- Mildronate,
- Mexidol,
- Actovegin,
- sodium hydroxybutyrate,
- Betimil,
- Neoton,
- Piracetam,
- Preductal,
- Cytomac.
They are used in the treatment of myocardial hypoxia in hospital and outpatient settings. Prescribed by injection in courses with a transition to a tablet maintenance dosage. Especially indicated for acute forms of hypoxia. Equated to first aid.
Group 2
With indirect exposure, the effect is ensured by transferring the heart to a lower level of oxygen consumption. The drugs simultaneously reduce all metabolic processes. They are needed in a short-term emergency to increase tissue survival. Long-term administration is impossible, since the mental functioning of the brain will decrease.
The following have a similar effect:
- sedatives and sleeping pills;
- drugs used for general anesthesia;
- some calcium channel blockers;
- part of α-blockers.
These remedies allow you to survive a difficult period, stimulate adaptive processes in the heart, but do not provide sustainable adaptation to stress.
Group 3
Mixed-action drugs have the properties of both previous groups. These include medicines developed and obtained from plants in combination with vitamin complexes (vitamins E, A, group B, D, C) and microelements necessary for the myocardium (potassium, magnesium, iron, selenium, chromium and others).
Indicated for chronic hypoxia, especially in the treatment of children and the elderly.
A modern direct-acting agent, used for acute and chronic forms of myocardial and brain hypoxia, not indicated during pregnancy and nursing mothers
Risk factors for the development of myocardial hypoxia
- Smoking. Nicotine damages the inner wall of blood vessels. A cholesterol plaque forms in the lumen, which leads to a slowdown in blood flow. This bad habit increases the risk of blood clots in the coronary vessels. Keep in mind that passive smoking also carries risks.
- Studies have shown an association between type 1 and type 2 diabetes and an increased risk of myocardial ischemia.
- Arterial hypertension. Increased pressure in blood vessels aggravates atherosclerosis. Hypertension is often inherited. If your parents or grandparents have had similar episodes, monitor your condition carefully and see a specialist regularly.
- High levels of cholesterol in the blood , which is the main component of atherosclerotic plaque. An increase in the “bad” fraction (low-density lipoproteins, LDL) occurs with inherited metabolic disorders or a diet high in cholesterol and saturated fat (fast food).
- High levels of triglycerides and other fats in the blood. This is a risk factor for the development of atherosclerosis of the heart vessels.
- Obesity. Leads to the development of arterial hypertension, increases the chance of developing diabetes, increases the level of “bad” cholesterol in the blood and leads to myocardial hypoxia.
- Waist circumference. More than 89 cm in women and 102 cm in men is a sign of an increased risk of heart disease.
- Lack of physical activity. The absence or small amount of this component of health has been proven to affect cholesterol and triglyceride levels in the blood. Aerobic exercises (fast walking, running, swimming) are recommended to reduce the risk of myocardial hypoxia and heart attack. Sports activity reduces arterial hypertension.