Small surges in blood pressure happen to everyone from time to time. Everyone knows that high blood pressure needs to be reduced, since it is very dangerous for human health. But how dangerous is pressure with parameters of 90 to 60 and what to do if low blood pressure is observed in a pregnant woman? According to doctors, this level of pressure in the upper systolic and lower diastolic is normal. But it is on the very border of the norm. If these cases are isolated, then there is no threat to pregnant women. However, when hypotension is more permanent and prolonged, this is a reason to think about your health and ask for advice from a specialist. If the pressure remains at 90 to 60 for a long period of time, kidney failure, as well as heart attack and cancer, may occur.
Causes of pressure 90 to 60 in pregnant women
Chronic pressure drops towards lower levels in pregnant women can negatively affect not only the health of the mother, but also affect the condition of the fetus. Low blood pressure does not become pathological so quickly. But if you do not take any action for a long time, you can feel the impact of pressure 90 to 60 during pregnancy. 90 is the lower threshold for upper blood pressure, the last obstacle on the way to a lower reading. For the body, the greatest danger is the upper systolic. Therefore, we will have to fight the normalization of pressure mainly based on the upper indicator.
The reasons why blood pressure decreases during pregnancy may be different, but pregnant women may have their own, different from generally accepted, factors that lead to a decrease in blood pressure. During the first trimester of pregnancy, quite low blood pressure can occur in many women and this is considered a physiological norm. But low blood pressure significantly aggravates the already unpleasant symptoms of pregnancy - early toxicosis, nausea, dizziness, headaches and even periodic fainting. In some cases, the cause of a decrease in blood pressure may be a hidden disease, so a pregnant woman should undergo a comprehensive examination in order to eliminate unwanted manifestations and protect the unborn baby from the consequences of the disease.
During the period of bearing a child, the expectant mother is worried about any, even the most minor, disturbances in well-being. Therefore, low blood pressure during pregnancy can put them in a state of panic. In order for a pregnant woman to understand the nature of this malfunction in the body, let us consider the reasons for its occurrence and how dangerous it is for the expectant mother and her fetus.
Hypertension in pregnant women
High blood pressure during pregnancy
Changes in blood pressure (BP) in women during pregnancy are observed quite often, which can adversely affect the mother and fetus. Blood pressure is one of the most important indicators of the functioning of the circulatory system in the body. During pregnancy, all organs and systems of the mother work under increased stress, especially the cardiovascular system. Therefore, it is necessary to regularly measure blood pressure to prevent the development of severe complications. At the beginning of pregnancy, blood pressure usually decreases slightly, due to the action of hormones. In later stages of pregnancy, as the fetus grows and the blood flow necessary for its nutrition increases, blood pressure may increase relative to physiological indicators before pregnancy. Arterial hypertension is said to exist if a pregnant woman’s blood pressure exceeds 140/90 mmHg. However, in women with low blood pressure before pregnancy, arterial hypertension may be present at blood pressure levels that are usually considered normal. Therefore, it is important to know your normal blood pressure.
Why is high blood pressure dangerous during pregnancy?
High blood pressure during pregnancy poses a great danger to the mother and fetus. Against this background, vasoconstriction occurs and the blood supply to all vital organs, including the placenta, is disrupted. Due to the lack of essential nutrients and oxygen, the growth and development of the fetus slows down. There is a serious danger of placental abruption, which is accompanied by bleeding and threatens the life of the mother and fetus. High blood pressure during pregnancy can cause the development of a dangerous pregnancy complication - preeclampsia. Manifestations of preeclampsia can also include swelling, large weight gain, and the presence of protein in the urine. Very dangerous symptoms of preeclampsia are: headache, blurred vision (“floaters”, “veils” before the eyes), pain in the upper abdomen. Deterioration of the general condition may be accompanied by dizziness, tinnitus, nausea, and vomiting. Preeclampsia can provoke a serious complication - eclampsia. In this condition, the pregnant woman loses consciousness and experiences convulsions.
Register for pregnancy at the antenatal clinic as early as possible!
A very important feature of arterial hypertension during pregnancy is that often even with high blood pressure numbers the patient feels normal. High blood pressure is detected by chance, during the next visit to the antenatal clinic. The absence of clinical manifestations of high blood pressure does not exclude the development of dangerous complications.
In order to promptly identify unwanted abnormalities during pregnancy and prevent the development of complications in the mother and fetus, pregnant women need to regularly monitor their blood pressure. It is very important to register for pregnancy at the antenatal clinic in a timely manner. The doctor will promptly detect changes in blood pressure and prescribe optimal therapy to maintain normal blood pressure. If a woman had high blood pressure before pregnancy and she is taking medications, it is necessary to adjust the treatment and individually select medications that can be taken during pregnancy. To prevent high blood pressure, a pregnant woman should eat a healthy and balanced diet, follow a drinking regime, and monitor weight gain. The antenatal clinic doctor will also give the correct recommendations on these issues. A pregnant woman must follow the recommendations and not violate the prescribed therapy.
What to do if a pregnant woman has high blood pressure?
If a pregnant woman regularly monitors her blood pressure on her own and notices even a slight increase in it while feeling well, she should visit a doctor at the antenatal clinic as soon as possible (before the scheduled next appointment). Self-administration of medications in this case is strictly prohibited. Before visiting a doctor, you can lower your blood pressure by taking a mild sedative based on motherwort or valerian.
If necessary, you can consult with an obstetrician-gynecologist at the remote medical advisory console of the Emergency Medical Care Station named after. A.S. Puchkova, Moscow by phone.
When is it necessary to call an ambulance?
If blood pressure rises suddenly, or you feel unwell, urgent hospitalization is necessary, and it is advisable for the patient to immediately call an emergency medical team. Signs that should alert you are: headache, sensation of flashing dots or “floaters”, blurred vision, pain in the upper abdomen, nausea, vomiting, agitation or depression, along with increased blood pressure. There may be a high level of convulsive readiness, which is manifested by twitching of the muscles of the face, neck, upper limbs, loss of consciousness and convulsions are possible.
What to do before the ambulance arrives?
First of all, go to bed, if possible eliminate all unwanted irritants (turn off all sources of noise, close the curtains), do not leave the pregnant woman alone, as convulsions may occur and help will be needed. Give it a position with the head end raised. You can take blood pressure lowering medications prescribed by your doctor. If a woman has not previously taken antihypertensive drugs, then she should not take drugs on the advice of others.
If an attack of convulsions occurs, the pregnant woman should be laid on a flat surface, her head should be turned to the side (to prevent aspiration of vomit), protected from injury (covered with a blanket), and not physically restrained. After an attack, clean the mouth with a napkin from vomit, blood and mucus. Wait for the ambulance to arrive!
The ambulance will arrive quickly and provide the necessary assistance. Hospitalization for this condition is mandatory. Only in a hospital is it possible to fully monitor the condition of the mother and child, complete therapy and determine a delivery plan.
We wish you health and happy motherhood!
Chief Specialist
in obstetrics and gynecology Arkhipova N.L.
Pathological hypotension. Causes
Pathological hypotension, which results in decreased blood pressure, has many causes:
- dehydration of the body;
- excessive overheating;
- various stresses;
- starvation;
- physical fatigue;
- chronic lack of sleep;
- a sharp transition of the body from a horizontal to a vertical position;
- prolonged standing;
- underweight;
- adynamia;
- colds or infectious diseases;
- large blood loss;
- extragenital pathological changes in the condition of the heart and vascular system, adrenal glands, thyroid gland, digestive organs, allergic manifestations and others.
Pregnant women can influence some of these factors on their own. However, if the pathology is severe, you should undergo an examination and identify the exact cause of the decrease in pressure. For pregnant women, even the most harmless reasons can pose a serious danger. If you feel very tired, weak, and your blood pressure is 90/60 or lower, this is a serious reason to consult a doctor. This may be affected by:
- changes in hormonal levels;
- the formed additional circle of blood circulation;
- increased volume of circulating blood;
- increased load on the cardiovascular system;
- increased heart rate, enlargement of the heart and the thickness of its walls.
When low blood pressure during early pregnancy occurs against the background of toxicosis, it can provoke frequent vomiting. Even if your pregnancy is going well, you will experience low blood pressure in the first and second trimesters. It will return to the original numbers closer to childbirth.
First trimester
Although this period passes without significant changes in the functioning of the cardiovascular system, the hormones progesterone and estrogen already from the first weeks of pregnancy contribute to the dilation of blood vessels. As a result, the pressure tends to decrease.
Special attention! The period from the 4th to the 12th week can become critical if the expectant mother actively exhibits early toxicosis. A decrease in blood pressure along with a deterioration in general health can cause discomfort.
Symptoms of Low Blood Pressure
What are the signs that accompany pregnancy pressure of 90 to 60? 90 in this case is in a borderline position and indicates that there are problems with the intensity of the heart “pump”. If the tonometer drops lower, placental insufficiency may occur due to insufficient blood supply and poor circulation. With poor blood supply, the child experiences a lack of oxygen as well as a lack of nutrients. Failure to take timely measures can lead to miscarriage or premature birth.
Low blood pressure is accompanied by symptoms such as:
- weakness;
- nausea;
- dizziness;
- drowsiness;
- rapid fatigue;
- frequent fainting;
- headache;
- noise in ears;
- the appearance of dark circles under the eyes.
Staying in a stuffy room or standing for a long time will only worsen these symptoms.
Hypotension: symptoms of the disease
Arterial hypotension as an independent disease (it is also called neurocirculatory dystonia of the hypotonic type) is a typical vascular neurosis. The onset of the disease can often be associated with neuropsychic trauma, emotional stress, and fatigue.
In cases where arterial hypotension is manifested only by a decrease in blood pressure, and there are no complaints or discomfort, it is classified as stable
(
compensated
) stage of the disease.
Unstable
(
subcompensated
) stage of the disease, in addition to a decrease in blood pressure, is manifested by other symptoms. Patients usually complain of headache, dizziness, general weakness, palpitations, discomfort in the heart area, sweating, memory loss, decreased ability to work, chilliness of the hands and feet, and meteosensitivity (deterioration when the weather changes). Some women experience so-called orthostatic phenomena: when getting out of bed, they experience dizziness, darkening of the eyes, even fainting. Fainting of a non-orthostatic nature can develop during an exacerbation of the disease or occur against the background of good health. Patients often develop irritability, emotional instability, and a tendency toward low mood.
Decompensated
arterial hypotension is characterized by hypotensive crises, easily occurring fainting, sleep disturbances, the appearance of acrocyanosis (bluish coloration of the fingertips, nose, lips, earlobes), loss of ability to work.
Hypotonic crises can last several minutes. During a crisis, blood pressure drops to 80/50 mmHg and below, headache and dizziness intensify, and vomiting may occur; patients feel severe weakness, a feeling of stuffy ears; A short-term loss of consciousness may occur, the skin and mucous membranes turn pale, and cold sweat appears. Fainting often develops in a stuffy room, in transport, after excitement, or during prolonged standing. Fainting is a fairly common occurrence in pregnant women.
In patients with arterial hypotension, blood pressure does not always remain persistently low: periodically it can reach normal and even elevated numbers - for example, when excited, upon admission to the hospital. However, it is rapidly declining.
Women with hypotension more often have an asthenic build (tall, thin) with pale skin. Almost half of them have varicose veins in their legs. The arms and legs feel cold to the touch, the pulse is somewhat lower than usual (about 60 beats per minute). No changes were detected during cardiac examination, including electrocardiography.
Low blood pressure at different times. Is it normal or not and why do such changes occur?
What to do if your blood pressure during pregnancy is 90 over 60? 90 indicates that your condition is close to the onset of pathological manifestations. However, it is still normal and you can prevent the tonometer from further decreasing. How to do it? First of all, you need to understand what pressure is optimal during pregnancy and when you should start worrying. The well-known generally accepted indicator of 120 to 80, when applied to each individual person, undergoes some changes due to his age, weight, state of health and other components.
Women undergo significant changes in their bodies during pregnancy, as hormonal status changes, fluid volumes increase, and blood characteristics change. All together affects the functioning of the heart. Therefore, up to the 20th week, low blood pressure is considered normal for pregnant women. And this happens as a result of an increase in the production of progesterone, a female hormone that dilates blood vessels. This causes a decrease in blood pressure during pregnancy in the 1st trimester. By the beginning of the third trimester, blood volume increases significantly, which puts additional stress on the vessels and blood pressure rises slightly. So the pressure of 90/60 during pregnancy in the 3rd trimester can level out and return to normal.
The lower threshold of pressure is considered normal at 90 to 60, and the upper threshold at 140 to 90. And they are considered normal when the woman feels well. After all, each person is individual and has his own pressure indicator. However, during pregnancy it is customary to operate with the following indicators:
- norm - from 120/80 to 129/84;
- the most optimal pressure is 100/60 – 119/79;
- with hypotension - below 100/60.
Pressure: norm and pathology
Blood pressure in most healthy people ranges from 140/90 to 90/60 millimeters of mercury. The upper numbers in these fractions characterize systolic pressure (in everyday life it is sometimes called “upper”). It is caused by the activity of the heart, which pumps blood into the aorta and further through the arteries of the whole body. The lower exponents of the fractions determine the diastolic (“lower”) pressure, which characterizes the state of vascular tone. Thus, the value of blood pressure depends on the condition of both the heart and blood vessels. The most common blood pressure level is 120/80-110/70 millimeters of mercury.
Violation of vascular tone is in the nature of arterial hypotension (this term is more correct than the word “hypotension”, which characterizes a decrease not in vascular, but in muscle tone), if blood pressure is below 100/60 millimeters of mercury. Such pressure occurs in 5-7% of people of both sexes aged 20-40 years, and in pregnant women even more often (on average 12%). However, not all of them should be considered sick. Many women do not respond to low blood pressure, remain in good health, have normal ability to work, and do not have any complaints; this is the so-called physiological hypotension. Others feel sick and have difficulty doing normal work.
Hypotension may be one of the symptoms of some other disease (peptic ulcer, infectious diseases, allergic conditions, adrenal or thyroid insufficiency, etc.) or an independent disease.
Proper nutrition and proper daily routine
How to normalize blood pressure during pregnancy? What can you do to prevent low blood pressure during pregnancy from bothering you and causing harm? The first thing you need to do is see a doctor, get examined and get advice that you strictly follow. But there are also recommendations that do not require a doctor to prescribe, and every expectant mother can follow them completely independently, improving the well-being of herself and her fetus. It's not difficult at all, but very effective.
Observe your daily routine carefully - go to bed on time, rest during the day, do not overexert yourself at work or at home, take walks in the air, change your body position more often, eat warm food.
A very important part of improving the physical condition of a pregnant woman is long walks in the fresh air. This is an excellent medicine for hypotension, since the body is saturated with oxygen during a walk and significantly improves the health of both the expectant mother and the unborn child.
Follow your diet and proper diet of foods. Breaks between meals should not exceed three hours. Eat small portions, but more often. Eat more protein foods, as well as fresh vegetables and fruits. Food should be warm and healthy.
Drinking regime and physical activity
Drinking regime is also important. Let your doctor give you recommendations on drinks - how much tea or coffee you can drink so as not to harm your baby. Drinks should be drunk warm, monitoring the body’s reaction to each of them.
Move more, do light fitness, do special exercises for pregnant women, practice swimming, water aerobics or yoga - they will help you tone your blood vessels and eliminate the feeling of weakness. Take a light contrast shower, sit in a warm bath with aromatic oils.
Stay positive!
Try not to change your body position suddenly, move smoothly and calmly so as not to provoke dizziness. Attract good emotions to yourself, listen to pleasant music, watch good, soulful films, delight yourself with meeting pleasant people - in general, more positive things. Don’t be scared or panic if your blood pressure during pregnancy is 90 over 60. 90 is not a pathology, but a completely normal indicator. It’s just that it is critically close to the decline line. To prevent this from happening, take the necessary measures in a timely manner and follow doctors’ orders.
Low blood pressure in the second trimester
If you did not encounter pressure of 90/60 during pregnancy in the 1st trimester, do not think that everything is already behind you and nothing threatens you in the future. This can also happen to you in the second trimester, when the poor health of the pregnant woman leads to poor oxygen access to the fetus and insufficient supply of nutrients to the fetus. Such manifestations slow down the development of the fetus and should be avoided. Symptoms that the pressure of 90/60 during pregnancy in the 2nd trimester is too low for a woman can be considered weakness, tinnitus, pathological drowsiness, rapid heartbeat and unreasonable fatigue.
Carefully monitor your condition, pay attention to the slightest ailments, because a decrease in pressure to a borderline state during this period is very dangerous. After the 12th week, hypotension is very difficult and causes a significant deterioration in the health of the pregnant woman. In general, pressure during pregnancy in the 2nd trimester is observed quite rarely, much less frequently than in the initial period. At this time, the level of progesterone becomes lower and the pressure returns to normal operating condition. The optimal pressure indicator in periods later than the first trimester is limited to 100/60 - at the lower limit and 140/90 at the upper limit.
If blood pressure decreases during pregnancy after the 12th week, this is fraught with a significant deterioration in the physical condition of the pregnant woman. It can also negatively affect the fetus in the womb due to insufficient supply of oxygen and nutrients to the embryo. To normalize blood pressure, you should take the same measures as in the first trimester - move more, take walks outside, eat right and have meals at least 5-6 times a day. By following these simple recommendations, you can bring your blood vessels into good tone and prepare your respiratory system for the future stress of labor.
Is it normal for the blood pressure to be 90/60 during pregnancy in the 3rd trimester? At such a long period of time, low blood pressure occurs in expectant mothers much less frequently than in the two previous periods. The tonometer readings tend to increase, because in the 3rd trimester the woman already gains significant weight, which, naturally, is reflected in the level of pressure. In addition, the volume of blood processed by the heart increases, which also increases blood pressure. The maximum and minimum pressure during pregnancy in the later stages remains the same as in the 2nd trimester.
Increased pressure
In the 3rd trimester of gestation, blood pressure tends to increase - this is explained by the load on the body and cardiovascular system, which now must pump twice as much blood. If blood pressure is recorded above 140/90 mmHg, and regularly, we speak of hypertension in pregnant women. This condition is manifested by a combination of symptoms:
- the appearance of redness on the skin of the face, neck and décolleté;
- vomiting and dizziness;
- numbness of the limbs;
- severe headache accompanied by ringing in the ears;
- severe swelling;
- flickering “flies” before the eyes, blurred vision.
The risk group for increased blood pressure in the later stages includes women who do not follow a diet, eat a lot of salty and spicy foods and lead a sedentary lifestyle. Also, a high chance of developing hypertension is noted in expectant mothers over 35 years of age. The most dangerous increase in blood pressure is for women suffering from diabetes mellitus, thyroid pathologies, renal and liver failure, as well as neurocirculatory dystonia.
It should be clarified that not all women during pregnancy have high blood pressure considered dangerous. The uterus is stuffed with spiral arteries that supply the fetus with nutrients through the bloodstream. The tortuous shape ensures compression of broken capillaries during menstruation and postpartum bleeding.
Normally, during pregnancy, the spiral arteries stop contracting, and their muscle tissue is replaced by dense connective tissue. This is necessary for a complete supply of blood to the fetus in any condition. For women whose spiral arteries have not degenerated into rough connective tissue, pressure surges during pregnancy are especially dangerous.
During hypertensive crises, almost all internal organs suffer:
- Placenta - it provides access of nutrients through the blood to the fetus. With high blood pressure, blood flow decreases and fetal distress develops. The baby's heart beats more than 170 or less than 110 times per minute, which can even cause the death of the fetus.
- Blood vessels – against the background of hormonal imbalances and nervous stress, capillary spasms occur. Due to the simultaneous increase in pressure, toxic breakdown products accumulate, oxygen starvation and signs of ischemia develop.
- Blood - it becomes thicker and more viscous, blood clots form in the capillaries, and the lumen of the vessels may be completely blocked.
- Kidneys - if an artery spasm occurs in one of the parts of the organ, the normal process of urine formation is disrupted. Protein enters the urine, edema develops, and the risk of kidney failure increases.
Such consequences are dangerous for both the expectant mother and the fetus. First of all, doctors warn about the development of preeclampsia and eclampsia.
Preeclampsia
This condition is considered dangerous for a woman during pregnancy. The diagnosis of preeclampsia is made based on the appearance of protein in urine laboratory results, significant swelling on the body, and increased blood pressure. Signs of preeclampsia are recorded in 4–20% of women, and patients at risk include:
- those suffering from diabetes and obesity;
- expectant mothers at a young age;
- patients with multiple pregnancies;
- those suffering from pathologies of the heart and blood vessels;
- women with documented autoimmune diseases and primary hypertension diagnosed before conception.
Preeclampsia is not asymptomatic; it is always accompanied by high blood pressure up to 150/90, swelling, nausea, severe pain in the head and deterioration of visual function. If regular listed symptoms occur, especially against the background of protein found in the urine, the woman is taken under strict medical supervision.
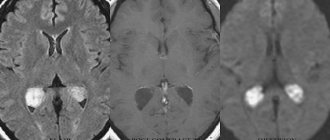
Eclampsia
This is a disease that is diagnosed only in pregnant women and is a form of gestosis. This condition is deadly because it is accompanied by loss of consciousness, convulsions, subsequent amnesia and the risk of coma. Eclampsia also carries the risk of developing pulmonary edema, cerebral hemorrhage and premature placental abruption.
Eclampsia is preceded by severe pregnancy with signs of gestosis, as well as regular surges in blood pressure above 150 mmHg. If this dangerous condition is suspected, the pregnant woman is urgently hospitalized and given intensive care.
Consequences
When a decrease in pressure occurs in later stages of pregnancy, this can lead to disruption of the contractile function of the uterus and become a threat to the labor of the expectant mother. If a woman’s blood pressure becomes 90/60 during pregnancy in the 3rd trimester, this is fraught with serious complications during childbirth and can cause heavy bleeding after the end of the birth process. Pregnant women who have low blood pressure often experience rather weak and sluggish labor. If it is impossible to complete the labor process on their own, obstetricians decide to perform labor stimulation or use a cesarean section.
What to do?
Despite the fact that cases of hypotension are quite rare in the final period, it is still possible to observe low blood pressure during pregnancy in the later stages. Especially if before conception the girl had frequent migraines and unstable blood pressure. In the last trimester, they have frequent ailments: sweating and trembling limbs, memory deteriorates and sudden changes in mood, nausea and dizziness, severe fatigue and general weakness, blood pulsates in the temples and the back of the head, darkness in the eyes and noise in the neck. ears, fainting occurs, and arrhythmia appears and the pulse quickens. At times, vomiting occurs, which is not associated with toxicosis.
These manifestations cannot be ignored. An ultrasound should be done to examine the condition of the fetus, because with hypotension in the milk-placental circle, blood circulation slows down, and this is very dangerous for the child, since it can cause intrauterine hypoxia. This seriously delays the time of labor because the woman cannot push hard. In order to prevent such developments in the later stages of pregnancy, you should worry about your health in the early stages, when symptoms are just forming and are not as severe as before childbirth.
Pregnancy in women with low blood pressure
The effect of pregnancy on blood pressure is observed very often. It can be expressed to varying degrees. More often it is limited to a decrease in systolic and diastolic pressure to values close to the minimum limit of normal fluctuations, but it can fall lower. Therefore, women with arterial hypotension often experience an exacerbation of the disease during this period.
For most women, deterioration occurs in early pregnancy. In 8 out of 10 women, pregnancy occurs with symptoms of early toxicosis, the addition of which aggravates hypotension, because Frequent vomiting, causing a lack of fluid in the body, helps lower blood pressure.
A condition called inferior vena cava syndrome should not be considered a manifestation of hypotension in pregnancy. It develops in the second half of pregnancy. When a woman is positioned on her back, as a result of the pregnant uterus squeezing the inferior vena cava, the blood flow to the heart is disrupted and a fainting state develops with a drop in blood pressure, a weakening of the pulse, and often with loss of consciousness. The condition quickly returns to normal when the woman turns on her side or sits down.
Advice for pregnant women with a predisposition to hypotension
In order to intervene in a timely manner during pregnancy and prevent hypotonic manifestations, you need to be very careful and constantly monitor the slightest deviations in your health. If you notice dangerous trends in your blood pressure, immediately consult a doctor and undergo the necessary examination.
Low blood pressure can manifest itself in the form of severe toxicosis or gestosis. If you ignore these signals from the body, a miscarriage may occur. Do not delay your visits to the doctor, as you are putting your unborn baby at risk.
In the calmer 2nd trimester, do not let your guard down and take your health just as seriously as you did in the 1st trimester. Follow the recommendations for increasing your blood pressure and proper nutrition until the problem is resolved.
Remember that persistently low blood pressure during pregnancy requires a professional approach and serious treatment. Only a specialist can tell whether your fears are groundless or whether there is a specific cause of the pathology.
If the pressure has decreased as a result of the disease, drug treatment is indicated. If it was just an attack of hypotension caused by a stuffy room or a sudden rise, then you should open the window, allowing air to come in, lie down, drink sweet tea, take 30 drops of cordiamine, which can quickly relieve spasms and increase blood pressure.
In the morning, in order to quickly recover, a pregnant woman needs to drink a cup of tea or coffee to increase her blood pressure, but do not overdo it - it is strictly not recommended for pregnant women to drink a lot of these drinks.