Pathogenesis
In accordance with the modern, so-called vascular theory, hypercapnia plays a key role in the pathogenesis of edema syndrome in CLS. Carbon dioxide, being a vasodilator, with an increase in its content in the blood, reduces peripheral vascular resistance and increases the capacity of the arterial bed. Due to the reduction of precapillary tone, the filtration equilibrium point in the capillaries shifts distally, which leads to the movement of fluid outside the vascular bed and loss of plasma volume. Of great importance in the development of edema in CLS is compensatory erythrocytosis in response to hypoxemia, an increase in hematocrit with a violation of the rheological properties of blood, the formation of erythrocyte aggregates, the development of capillary stasis, which causes perfusion disturbances and the movement of the liquid fraction of blood outside the vascular bed. The occurrence of edema is also facilitated by extrathoracic deposition of blood due to increased intrathoracic pressure and prolongation of exhalation, which significantly worsens the conditions for venous return of blood to the heart and creates the preconditions for stagnation in the systems of both the superior and inferior vena cava.
As the resistance load increases due to pulmonary hypertension (PH), hypoxemia, and metabolic disorders in the myocardium, hypertrophy, dilatation and failure of the right ventricle of the heart develop. In patients with diseases that primarily affect the pulmonary vessels (idiopathic PH, postthromboembolic PH, etc.), the leading cause of the development of peripheral edema is right ventricular heart failure (HF) due to hemodynamic overload caused by high PH.
Risk factors for chronic heart failure
The causes of the disease are various factors: from serious heart pathologies to poor diet. Let's highlight the main ones :
- ischemic disease, in which the muscle does not receive the oxygen it needs;
- recent heart attack;
- essential hypertension (high blood pressure);
- diabetes mellitus, which doubles the risk of developing chronic heart failure in men and increases the likelihood of developing the disease in women by 5 times;
- dilated cardiomyopathy - a condition in which the heart becomes larger and wider for no known reason;
- heart valve disease, especially aortic stenosis, when blood cannot pass through one of the heart's main valves;
- mitral and aortic regurgitation, when blood can flow in the opposite direction;
- alcoholic cardiomyopathy - large amounts of alcohol makes the heart larger and less efficient;
- inflammation of the heart muscle or myocarditis (usually of viral origin);
- chronic arrhythmia;
- HIV AIDS.
The causes of the disease are also certain types of medications, endocrine diseases, vitamin deficiency, obesity and other conditions.
Clinical picture
The basis for the clinical diagnosis of CHL is the addition to the clinical symptoms of the underlying disease (cough, wheezing in the lungs, etc.), manifestations of pulmonary insufficiency (shortness of breath, cyanosis), pulmonary hypertension (emphasis of the second tone over the pulmonary artery, Graham-Still noise) signs of blood stagnation in the large circle - peripheral edema and hepatomegaly. Swelling initially occurs on the feet and legs, progressing to the upper parts of the body. In the evening, as a rule, they increase. The liver is enlarged mainly due to the left lobe, has a rounded edge, is sensitive or moderately painful on palpation. In some cases, the liver can protrude from under the edge of the costal arch even if its size is normal, which is often observed with pulmonary emphysema and a low position of the diaphragm.
Swelling of the neck veins is often a consequence of increased intrathoracic pressure, with the veins swelling during exhalation and collapsing during inspiration. With the development of right ventricular failure, the dependence of the filling of the jugular veins on the respiratory phase decreases.
Classifications and examples of diagnosis formulation
The severity of circulatory failure (CI) is assessed according to the classification of the Association of Phthisiologists and Pulmonologists of Ukraine (2003). The classification involves dividing patients into groups according to three stages of NC:
1) NC stage I: the presence of mild signs of blood stagnation in the systemic circulation - swelling in the legs, enlarged liver, which disappear under the influence of therapy only for the underlying disease or in combination with diuretics;
2) NC stage II: the presence of pronounced edema and hepatomegaly, requiring intensive, often combined treatment with diuretics; at this stage, as a rule, disturbances in the contractile function of the myocardium are observed, and therefore complex treatment using drugs to correct vascular tone, inotropic drugs, and antiplatelet agents is advisable;
3) NC stage III: terminal stage, characterized by secondary damage to other organs and systems; the only remedy that can at least slightly prolong the life of these patients is continuous oxygen therapy.
The above division of patients into groups depending on the stage applies only to NK in the systemic circulation, since post-capillary stagnation of blood in the pulmonary circulation (left ventricular failure in the form of cardiac asthma and pulmonary edema) in patients with chronic lung diseases, as a rule, is not observed.
The formulation of the diagnosis consists of four components: the name of the disease (indicating the degree of severity and phase of the course), LN (indicating the degree), chronic pulmonary heart disease, NC (indicating the stage). For example: chronic obstructive pulmonary disease, stage III, exacerbation phase, stage II pulmonary disease, chronic pulmonary heart disease, stage I NC.
Treatment of chronic heart failure
The outlook for the disease depends on the underlying cause of the disease and the severity of the symptoms. The following are used in the treatment of chronic heart failure :
- Lifestyle changes - rational rest, lack of overload, adequate sleep, a healthy diet low in sodium and fat, weight loss, introduction of physical activity.
- Drug therapy - drugs to dilate the walls of blood vessels and support the heart. Among the main drug groups: ACE inhibitors, beta blockers, diuretics, angiotensin receptor blockers
- Surgical operations - coronary artery bypass surgery or angioplasty, installation of internal pacemakers, reconstructive operations, transplantation and much more.
Prevention of chronic heart failure is of paramount importance even after a full course of treatment due to the frequent development of relapses. The goals of the doctors at our clinic are to stop the pathological development of myocardial damage and prevent risk factors that can lead to disability and death. We competently correlate the data obtained as a result of diagnostics in order to develop an effective course of treatment based on them and restore the health of the person who contacts us.
Rate this article
Article rating 4.33 out of 5. Votes: 15.
Latest articles
Sexual transmission of infections
Sexually transmitted infections or STIs are dangerous diseases that can undermine health and lead to dire consequences. Most of the diseases in this group are…
Hormonal disorders
A woman’s well-being largely depends on the endocrine system. Any hormonal imbalance can cause a sharp deterioration in health, weakening the immune system...
Cervical dysplasia
Cervical intraepithelial neoplasia or cervical dysplasia is a precancerous condition expressed by pathological changes in cells. In most...
Diagnostics
The purpose of using laboratory and instrumental research methods is to determine the treatment tactics for patients.
The main tasks of conducting diagnostic studies:
— diagnosis of possible concomitant diseases of the cardiovascular system;
— diagnosis and assessment of the degree of impairment of the contractile function of the right ventricle when determining the feasibility and volume of therapy with inotropic agents;
— assessment of the degree of hemoconcentration when prescribing infusion therapy;
— assessment of the degree of hypoxemia when determining the feasibility and selection of oxygen therapy regimens.
Instrumental and other diagnostic methods
X-ray of the chest organs. In patients with chronic lung diseases, small sizes of the atria and ventricles are usually observed; there may be signs of hypertrophy of the outflow tract from the right ventricle - bulging of the pulmonary cone. In severe cases, the second arch of the pulmonary cone protruding along the left contour can imitate the mitral configuration of the heart. In subsequent stages of development of CHL, a progressive enlargement of the right ventricle due to hypertrophy and dilation is determined. In patients with the vascular form of CHL (idiopathic and chronic post-embolic PH), the trunk and main branches of the pulmonary artery are significantly dilated. A reliable sign of high PH is an increase in the diameter of the right descending branch of the pulmonary artery by more than 18 mm. Sometimes the expansion of the right descending branch becomes aneurysmal in nature, and the aneurysm on the radiograph is mistaken for a neoplastic or tuberculous process. The sizes of the right atrium and right ventricle are sharply increased, while the left parts of the heart may be reduced.
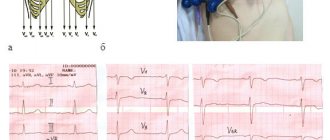
Electrocardiography (ECG) allows you to confidently diagnose right ventricular hypertrophy in patients with the vascular form of CHL (Rv1 > 7 mm, often in combination with complete right bundle branch block, Rv1 + Sv5 > 10.5 mm and other direct signs of hypertrophy). In patients with CLS caused by primary damage to the bronchi and lung parenchyma, an S-type electrocardiogram is usually recorded. However, it should be noted that hypertrophy is a normal reaction of the myocardium to hyperfunction (compensatory increase in cardiac output in response to hypoxemia and resistance load due to PH), which is observed in patients without signs of circulatory decompensation, that is, without CHL. An ECG can be useful if concomitant diseases of the cardiovascular system are suspected, for example, coronary artery disease (depression of the S-T segment, changes in the T wave, etc.), in diagnosing metabolic disorders in the heart muscle, manifested mainly by disorders of myocardial repolarization processes.
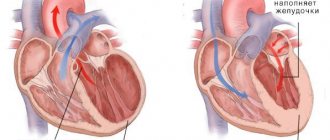
Echocardiography (EchoCG) is the most accurate method for diagnosing hypertrophy, dilatation and failure of the right ventricle of the heart; measurement of the thickness of the anterior wall of the right ventricle is carried out in M-mode using a standard anterior approach. In healthy individuals, this figure usually does not exceed 0.3 cm, in patients with chronic lung diseases, the thickness of the anterior wall ranges from 0.3 to 0.45 cm, in vascular forms of CHL - more than 0.5 cm. Assessment of the degree of dilatation of the right ventricle based on determining the anteroposterior size of its cavity is not reliable enough; a more reliable way is to analyze orthogonal sections from the apical approach based on the Simpson method. The main sign of impaired contractile function of the right ventricle is a decrease in the ejection fraction (normal - 46.8 ± 1.48%).
The study of the gas composition and acid-base state of the blood allows you to diagnose and assess the severity of arterial hypoxemia (PaO2 < 65 mm Hg, SaO2 < 93%), hypercapnia (PaCO2 > 40 mm Hg), and respiratory acidosis. Signs of compensated respiratory acidosis are an increase in PaCO2, bicarbonate content and excess buffer bases at normal blood pH. Signs of uncompensated acidosis are an increase in PaCO2, a decrease in the level of bicarbonates, excess buffer bases and blood pH. In idiopathic and post-embolic PH, right ventricular heart failure often develops against the background of hypocapnia and respiratory alkalosis.
The essence of chronic heart failure
The term is used to describe a condition in which the heart is unable to adequately pump blood throughout the body. The disease forces the organ to work under extreme stress, causing irreparable damage to itself. Partial performance of functions ceases, the efficiency of work is disrupted, up to the complete stop of the organ in particularly critical situations.
CHF makes it impossible for the heart muscle to contract normally and empty its chambers. The myocardium fails when filling the ventricles and atria with blood. This creates an imbalance in systems and provokes a deterioration in well-being. The pathology can begin suddenly due to some important event, for example, a heart attack.
Sometimes chronic heart failure develops slowly. The heart tries to adapt to the overwhelming load, without showing acute signs of the disease for a long time. But then malfunctions appear, for which you should immediately consult a doctor to prescribe effective treatment.