Renal artery stenosis is a pathology caused by hereditary or acquired changes in arterial vessels, which is a narrowing of one or both renal arteries or their branches. This condition causes a disruption in the process of perfusion - the passage of fluid - through the kidneys, leading to a decline in the blood supply to the kidneys and high blood pressure. In addition, renal artery stenosis can lead to heart failure, kidney failure, stroke and myocardial infarction.
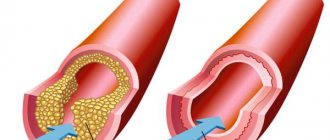
Atherosclerosis
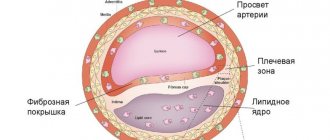
Most often, renal artery stenosis provokes atherosclerosis. This term refers to the process of accumulation of plaque from cholesterol, fats and calcium on the renal arteries, which causes them to narrow. The risk of getting this disease increases with age. At risk are patients with damage to the aorta, arterial hypertension, and damage to the iliac arteries. This pathology is characterized by damage to one group of vessels due to stenosis, sclerosis, obliteration of arteries, and atherothrombotic disorders. Often, stenosis is located in the proximal segments of the renal arteries near the aorta, in the middle segments, at the bifurcation of the arteries, in the distal branches of the renal arteries.
Possible complications
Restenosis is more common in people whose renal vessels were very narrow to begin with, in patients over 65 years of age, women and smokers. Sometimes another stenting procedure may be needed to re-unblock the artery.
Risks of renal artery stenting include:
- Bruising in the area where the catheter was inserted
- Bleeding at or around the injection site,
- Damage to the vessel
- Thrombosis,
- An allergic reaction to the dye used during the procedure,
- Stent displacement
- Kidney failure
- Urinary tract infection.
Nephrological pathologies
Nephrological pathologies are the least likely cause of stenosis. Such pathologies include aneurysms, hypoplasia, occlusion and external compression of the renal arteries, vasculitis, thrombosis, nephroptosis, arteriovenous shunts.
Doctors also identify several risk factors that contribute to the disease. Such predisposing factors include:
- smoking;
- poor nutrition (predominance of foods high in sugar, fat and cholesterol in the diet);
- obesity;
- genetic predisposition;
- chronic kidney disease;
- increased blood glucose and cholesterol;
- elderly age.
Symptoms of renal artery stenosis
Patients who are concerned about the following conditions should undergo a comprehensive examination by a nephrologist:
- Kidney failure - appears due to a malfunction of the kidneys, caused by a slowdown in their blood supply due to a decrease in the diameter of the arteries.
- High blood pressure, which cannot be reduced by prescribing antihypertensive drugs.
- The appearance of noises that can be detected when examining the abdomen with a stethoscope.
- Increased blood pressure (severe or moderate) in patients with a history of stroke or myocardial infarction.
- Increased blood pressure in patients under 30 years of age and over 50 years of age.
- Impaired kidney function after taking antihypertensive medications such as an angiotensin receptor blocker or an angiotensin-converting enzyme inhibitor.
Thus, we can say that renal artery stenosis is found in patients with hypertension and impaired renal function. Common symptoms of renal artery stenosis include: dizziness, sleep disturbances, shortness of breath, rapid heartbeat, muscle weakness, memory loss, lower back pain, emotional instability, spots before the eyes, swelling in the ankles, vomiting and nausea, decreased or increased urination.
Diagnosis of renal artery stenosis
- Laboratory research. An increase in blood urea nitrogen and serum creatine are the first indicators of the disease that the doctor pays attention to. To make a diagnosis, a urine test is also prescribed, which shows, in the presence of the disease, scanty urinary sediment and proteinuria.
- Duplex ultrasound of the renal arteries is the most accessible and accurate method for diagnosing the disease, which allows you to assess the severity of stenosis by assessing the speed of blood flow in the arteries. The presence of pathology will be indicated by accelerated blood flow provoked by narrowing of the arteries. However, it is worth considering that in patients with obesity or flatulence, ultrasound results may be unreliable.
- Renal scintigraphy: is ordered to compare the perfusion of the left and right kidney. This method is also used to measure glomerular filtration rate in the kidneys.
- Magnetic resonance angiography. This technique allows you to obtain images of the renal arteries and aorta. The advantages of MRI for diagnosing stenosis are its non-invasiveness and the ability to obtain a three-dimensional image of the affected part of the artery. However, this technique also has disadvantages: high cost, overestimation of the severity of stenosis, and the inability in some cases to distinguish stenosis from occlusion.
- Selective renal arteriography: allows you to determine the extent and location of arterial damage. It is carried out by introducing radiocontrast agents.
Treatment of renal artery stenosis
Initially, treatment for renal artery stenosis involved removal of the affected organ. But nowadays there are effective surgical and conservative methods for eliminating this disease.
Drug treatment of pathology depends on its stage:
- First stage (moderate hypertension). At this stage of the pathology, the patient feels well and has normal kidney function, the pressure is normal or exceeds its upper limit. To treat stenosis, your doctor may prescribe antihypertensive or diuretic medications.
- Second stage (compensation). The clinical picture of the disease at this stage is more pronounced: persistent hypertension appears, impaired renal function is observed, as well as their decrease. The patient needs complex treatment under the supervision of a doctor.
- Third stage (decompensation). The patient has severe hypertension, which cannot be eliminated with the help of antihypertensive drugs; the kidneys practically stop working and significantly decrease in size. Since the patient’s health condition is rapidly deteriorating, his treatment is carried out exclusively in a hospital setting.
At all stages of the disease, doctors usually prescribe medications from the groups of angiotensin-II receptor blockers and ACE inhibitors. To lower cholesterol in the blood and stabilize atherosclerotic plaques in the arteries, medications from the class of statins are prescribed.
For effective treatment of stenosis, it is recommended to quit smoking and lose weight in case of obesity. In addition, it is necessary to follow a low-carbohydrate diet, which will help lower blood sugar levels and thereby prevent diabetic kidney damage. Such a diet will also help lower blood cholesterol levels, which will slow down the development of both atherosclerosis and stenosis.
Advantages of treatment at the Assuta clinic
- The opportunity to use the services of world-famous nephrologists collaborating with the Assuta clinic.
- Access to advanced technologies and treatment methods not used in most post-Soviet countries.
- Comfortable conditions in the clinic, rooms equipped with everything necessary for a comfortable treatment.
- Affordable prices, no prepayments, the ability to pay for services upon receipt.
If you show signs of illness, seek medical attention as soon as possible. To get a consultation with an Israeli nephrologist, leave your contact information in any of the application forms, call or request a call back.
- 5
- 4
- 3
- 2
- 1
(0 votes, average: 5 out of 5)
Surgery
In difficult cases, it is not possible to cure stenosis using conservative methods, so it is necessary to resort to surgical methods. Typically, surgery is prescribed for the following indications: unstable angina or pulmonary edema in the presence of hemodynamically significant stenosis, chronic renal failure, arterial stenosis in the presence of one working kidney, uncontrolled hypertension, bilateral hemodynamically significant stenosis.
- Bypass surgery is the creation of another path for blood flow (bypassing the affected area of the artery) using shunts.
- Angioplasty is the expansion of a narrowed vessel by inserting an inflating balloon into it.
- Stenting is the expansion of the renal artery using a mesh or springy stent, which is placed inside the vessel, thereby widening it and improving blood flow.
- Arterial section resection—removal of the diseased section of the artery.
- Prosthetics is a reconstructive operation that is usually performed after renal artery resection. It is prescribed to restore normal blood flow by replacing a renal artery implant.
- Nephrectomy is a radical method of treating pathology, which involves complete removal of the affected organ.
Publications in the media
Vasorenal arterial hypertension (AH, renovascular hypertension) is symptomatic (secondary) hypertension caused by ischemia of the kidney(s) due to narrowing of the renal artery or its branches, rarely due to bilateral damage. Statistical data. The prevalence is 1–2% (up to 4–16% according to specialized clinics) among all types of hypertension.
Etiology
• The most common cause of renal artery stenosis is atherosclerosis (reported among all types of renal artery stenosis in 62%). Localization of atheromatous plaques •• Proximal segments of the renal artery near the aorta (74% of cases) •• Middle segments of the renal artery (16% of cases) •• Near the bifurcation of the renal artery (5% of cases) •• Distal branches of the renal artery (5% of cases).
• Less commonly (in 24% of patients), a congenital disease is noted - fibromuscular dysplasia. The lesion is localized in the middle third of the renal artery. The following types of process are distinguished: •• Proliferation of the inner membrane ••• Primary ••• Secondary •• Dysplasia of the middle layer ••• Hyperplasia of the middle layer ••• Perimedial fibrous dysplasia ••• Dysplasia with the formation of microaneurysms ••• Dissection of the middle layer •• Subadventitial fibroplasia.
• Other types of stenotic lesions of the renal arteries are observed in 6% of cases •• Congenital artery stenosis (the most common cause of hypertension in children) •• Renal artery aneurysm •• Traumatic thrombosis and embolism •• Coarctation of the aorta with renal artery stenosis •• Nonspecific aortoarteritis •• Compression of the vascular pedicle of the kidney from the outside by a tumor or foreign body.
Pathogenesis
• Constriction of the renal artery activates the juxtaglomerular apparatus due to a decrease in blood pressure in the poststenotic segment, which leads to the release of renin, and a decrease in sodium concentration in the nephron loop.
• Renin converts angiotensinogen coming from the liver into angiotensin I, which is converted under the influence of ACE into angiotensin II, which directly affects systemic arterioles and sharply increases peripheral resistance.
• Indirectly through the adrenal cortex, angiotensin II leads to hyperaldosteronism, sodium retention in the body and an increase in extracellular fluid volume.
• The results of surgical treatment are largely determined by whether one or both renal arteries are affected •• With unilateral stenosis, the cause of hypertension is the renopressor mechanisms of the ischemic kidney. However, over time, the contralateral intact kidney will switch to a new blood pressure regime and will maintain hypertension even when the original source of hypertension is removed or revascularized •• With bilateral renal artery stenosis, its gradual elimination usually leads to a decrease in blood pressure. The same is observed during revascularization of a single kidney.
Clinical manifestations
• Renal artery stenosis can be suspected when hypertension occurs unexpectedly or when previously benign hypertension suddenly worsens. Arterial hypertension occurs before age 30 or after age 50, usually in the absence of a family history of hypertension. Characterized by rapid progression of hypertension, high blood pressure, rapid target organ damage, and resistance to treatment.
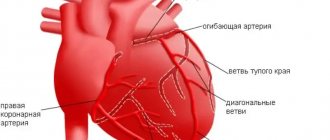
• Complaints •• Characteristic of cerebral hypertension - headaches, a feeling of heaviness in the head, hot flashes, tinnitus, pain in the eyeballs, memory loss, poor sleep, irritability, flashing “floaters” before the eyes •• Associated with overload of the left parts of the heart and relative or true coronary insufficiency - pain in the heart, palpitations, shortness of breath, a feeling of heaviness in the chest •• Caused by urological pathology - a feeling of heaviness, or dull pain in the lumbar region, and in the case of a kidney infarction - hematuria •• Caused by ischemia of others organs, the main arteries of which can be affected simultaneously with the renal arteries ••• Symptoms of ischemia of the gastrointestinal tract ••• Ischemia of the upper or lower extremities ••• Signs of cerebral atherosclerosis •• Signs of an inflammatory reaction (with nonspecific aortoarteritis) •• Complaints typical for secondary hyperaldosteronism - muscle weakness, paresthesia, attacks of tetany, isohyposthenuria, polydipsia, nocturia.
• As with any renal hypertension, high levels of diastolic blood pressure are characteristic, reaching in some cases 170 mm Hg.
• Systolic murmur in the right or left upper quadrant of the abdomen and along the posterior wall of the chest. The murmur is usually low-intensity, in contrast to the murmur heard with arteriovenous fistula of the kidney or atherosclerosis of the abdominal aorta (rough and prolonged).
Laboratory and instrumental data
• Hypokalemia (due to excessive secretion of aldosterone).
• Determination of plasma renin activity, especially in combination with the captopril test (100% sensitivity and 95% specificity): an increase in plasma renin activity after taking captopril by more than 100% of the initial value indicates pathologically high renin secretion, and is a sign of renovascular hypertension
• X-ray contrast angiography is the “gold standard” in the diagnosis of renal artery stenosis. The transfemoral Seldinger method is preferable: stenosis of the renal artery and (distal to it) its fusiform expansion are detected •• With nephroptosis, the renal artery is tense, it departs from the aorta at an acute angle, its diameter is narrowed •• With atherosclerosis of the renal artery, the filling defect is most often located near the mouth renal artery. Often, an angiogram reveals signs of atherosclerosis of the aorta •• With fibromuscular dysplasia, a multifocal narrowing of the renal artery is determined, in most cases starting at a distance of 2 cm distal to the origin of the artery from the aorta •• With nonspecific aortoarteritis, weaselation of the walls of the abdominal aorta is found along with narrowing of the renal artery. Stenotic lesions of other branches of the aorta are often determined •• In case of thrombosis or embolism of the renal artery, the symptom of a “blind ending” of the trunk of the renal artery or one of its main branches is determined •• In case of an aneurysm of the renal artery, its saccular or fusiform expansion is located mainly in the area of the renal hilum. The walls of the aneurysm often become calcified.
• Asymmetry of the kidneys on ultrasound.
• Doppler study of the renal arteries - acceleration of blood flow and its turbulence.
• Renal scintigraphy - decreased drug absorption, decreased drug delivery to the affected kidney, asymmetry of renographic curves. The optimal combination of renal scintigraphy and captopril at a dose of 25–50 mg orally. When taking captopril, the entry of the isotope into the kidney tissue decreases. A normal renal scintigram after taking captopril excludes hemodynamically significant renal artery stenosis.
• Excretory urography: the intensity of concentration of the contrast agent and the time of its appearance on the urogram may be reduced, as well as a decrease in the size of the kidney; however, the excretory urogram may remain normal, so the final diagnosis requires confirmation by aortography.
• MRI of the renal arteries is a modern method for verifying renovascular hypertension.
Differential diagnosis • Primary aldosteronism • Pheochromocytoma • Cushing's syndrome • Coarctation of the aorta • Diseases of the renal parenchyma, leading, for example, to chronic renal failure.
TREATMENT
General tactics. First of all, it is necessary to consider the possibility of radical treatment - percutaneous transluminal renal angioplasty, stenting of a stenotic artery, or radical surgical treatment. If such treatment is impossible or there are contraindications to it, drug therapy is prescribed.
Drug therapy is auxiliary, because a decrease in blood pressure with renal artery stenosis is non-physiological (leads to decompensation of blood circulation in the kidney and its shrinkage).
• Indications for long-term treatment are older age and systemic damage to the arterial bed, including the coronary arteries.
• Drugs of choice are ACE inhibitors, such as captopril. Additionally, other antihypertensive drugs are prescribed (see Arterial hypertension). Treatment begins with minimal doses of short-acting ACE inhibitors (for example, captopril at a dose of 6.25 mg). In the absence of collapse, the dose of captopril is increased or long-acting ACE inhibitors are prescribed. Monitoring of creatinine and GFR levels is necessary. ACE inhibitors are contraindicated in bilateral renal artery stenosis.
Balloon dilatation of the renal arteries
• Opinions about its effectiveness are controversial. In any case, this method is a good prognostic criterion for subsequent surgery: if after adequate dilatation even temporary normalization of blood pressure occurs, we can talk about a direct dependence of hypertension on renal artery stenosis.
• Indications •• Therapy-resistant hypertension in patients over 60 years of age with angiographically detected stenosis of the renal arteries •• Risk factors (stenosis of the carotid, coronary arteries, cardiac and respiratory failure) •• Renal failure caused by stenosis of the renal arteries •• Restenosis of the renal arteries after their revascularization or kidney transplantation •• As a diagnostic procedure to determine the relationship between renal artery stenosis and hypertension.
Surgery
• Organ-sparing operations •• Resection of the renal artery with reimplantation into the aorta •• Resection with end-to-end anastomosis •• Transaortic endarterectomy •• Autoplasty of the renal arteries with free grafts •• Creation of a splenorenal anastomosis •• Plastic surgery of the renal artery with synthetic antithrombogenic prostheses.
• Nephrectomy - if it is impossible to perform reconstructive surgery on the artery (the share of nephrectomies in the total number of operations is 16–20%).
• Contraindications •• Bilateral extended damage to the renal arteries •• Shrinkage of both kidneys •• Myocardial infarction and the period up to 6 months after it •• acute cerebrovascular accident •• End-stage chronic renal failure.
• Postoperative complications •• Internal bleeding •• Thrombosis of vascular anastomoses •• AKI.
• Results of operations •• Mortality is 0–6% •• Positive results with atherosclerosis of the renal artery are noted in 63% of patients, with fibromuscular dysplasia - in 73% •• The period of normalization of blood pressure after surgery can last up to 6 months.
• Postoperative management. Dispensary registration is recommended for patients. For residual hypertension, antihypertensive drugs are prescribed.
Reduction. AH - arterial hypertension.
ICD-10 • I15.0 Renovascular hypertension
Prognosis for renal artery stenosis
Untimely treatment of the disease can provoke consequences such as stroke, kidney and heart failure, and vascular atherosclerosis. In case of timely treatment, when the pathology has not yet reached a severe stage, the prognosis for the patient is favorable. It will take about 4-6 months for complete recovery from stenosis.
To prevent renal artery stenosis you need to:
- Get a medical checkup once a year to make sure your kidney function and blood pressure are normal;
- eat right - give preference to lean meat, fruits, limit the consumption of salt, canned food, sweets, donuts, chips, butter, lard and milk;
- exercise regularly;
- maintain a healthy weight;
- give up alcohol and smoking;
- avoid emotional and physical stress;
- monitor pressure.
Types of vascular kidney diseases
Diseases of the vessels of the kidneys and urinary system are classified into groups:
- atheroembolic disease;
- thrombosis of renal vessels, stenosis;
- arterial blockage;
- cortical necrosis;
- nephrosclerosis;
- vascular tumors of the kidney;
- developmental anomalies.
Congenital anomalies in the development of kidney vessels include an extra, accessory vessel. Changes in the number of arteries interfere with the blood flow necessary for proper functioning.