The brain is the main organ in the body. The functioning of all organ systems, general condition and quality of life depend on its functioning. With the development of certain pathologies, the brain begins to suffer due to lack of oxygen, and this can lead to serious consequences. One of these diseases is grade 2 cerebral ischemia in newborns; the consequences can be disastrous if urgent measures are not taken and therapy is not started. Let's look at what this pathology is and whether it is possible to get rid of it.
Concept of cerebral ischemia
Not everyone understands the name of the disease as “cerebral ischemia of the 2nd degree in newborns.” The doctor can explain this and choose treatment tactics. This pathology is a condition in which the blood supply to the brain is disrupted. In newly born infants, this pathology, as an independent disease, is not often diagnosed.
Most often, newborns are diagnosed with “ischemic encephalopathy,” in which brain cells are damaged due to poor blood supply, that is, lack of oxygen.
If a diagnosis of “grade 2 cerebral ischemia in newborns” is made, how to treat this pathology is determined by the attending physician, depending on the condition of the body and concomitant diseases.
Signs and symptoms of cerebral ischemia in newborns
The disease manifests itself with obvious symptoms that attract attention.
- The child is easily excitable, cries for no reason, sleeps poorly, shudders, and has tremors.
- Muscle tone is reduced, the baby moves little, has difficulty sucking and swallowing.
- The fontanel is enlarged, intracranial pressure is increased due to the fact that fluid accumulates in the brain.
- Convulsions, twitching of the limbs and head, as well as comatose states with loss of coordination of movements and consciousness occur.
- The newborn's skin takes on a marbled hue.
- The functioning of the gastrointestinal tract is disrupted - bloating, constipation, and diarrhea are observed.
Reasons for the development of ischemia
This pathology in newborns can develop for several reasons:
- If during gestation the placental blood flow was disrupted.
- After birth, respiratory distress was observed.
- Respiratory distress syndrome.
- Congenital pneumonia.
- Frequent episodes of respiratory arrest.
- Aspiration.
- Congenital malformations.
Whatever the reasons, grade 2 cerebral ischemia in a newborn can have serious consequences if therapy is not started in a timely manner.
About prevention
To prevent the development of ischemic manifestations in the unborn baby, a woman must:
- Plan your pregnancy carefully.
- Undergo the necessary examination procedures during pregnancy.
- If required, take iron supplements as prescribed by your doctor.
- Completely give up bad habits.
- Do moderate exercise.
- Eat a balanced diet, follow your daily routine, and get plenty of rest.
- If the pregnancy is difficult, you should be treated in a hospital.
This is the only way to minimize the likelihood of cerebral ischemia in the child.
Development of pathology in a child
Oxygen is carried throughout the body along with blood. It is vital for the normal functioning of all organs. If there is a deficiency, a redistribution of blood flow occurs and the heart and brain receive oxygen-rich blood first. It turns out that other organ systems begin to suffer from its deficiency.
If the pathology is not identified in a timely manner and the causes that provoked it are not eliminated, then the lack of oxygen will gradually begin to negatively affect the condition of the nerve cells - they begin to die. This is how grade 2 cerebral ischemia develops in newborns, the consequences depend on the severity of the condition and the quick response of doctors. The prognosis for the baby will also depend on the number of dead cells. If a cerebral hemorrhage occurs, the chances of recovery and survival are significantly reduced.
Development mechanism
Violation of the metabolism of brain cells during ischemia leads to irreversible processes of destruction of nerve structures and disruption of their activity. As a rule, the mechanism of formation of the pathological process is based on a rapid decrease in the level of adenosine triphosphoric acid, which is the main energy source in the body.
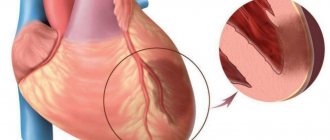
Impaired cerebral circulation creates favorable conditions for the formation of ischemia
For the full functioning of neurons, a balance is required between the concentration of intracellular and extracellular ions penetrating through the membranes. Long-term oxygen deficiency creates an imbalance of transmembrane components of the brain, which subsequently dramatically changes the concentration of potassium and sodium. This leads to a decrease in membrane potentials. In parallel with these processes, there is an increase in calcium levels, which allows the release of the neurotransmitter glutamate, which overstimulates brain receptors, thereby promoting structural and functional changes in the brain.
The body's first response to perinatal oxygen deficiency is to increase blood supply to the main organs. Subsequent arterial hypotension leads to a throughput decrease in cerebral blood flow.
Pathological changes in the brain in a newborn
Thus, the following stages are distinguished in the mechanism of development of pathology:
- Intrauterine oxygen deficiency.
- Decreased oxygen supply to the brain and increased carbon dioxide concentration.
- Increased acid-base environment in the fetus.
- Swelling of intracellular components.
- Increase in brain tissue volume.
- Local decrease in cerebral circulation.
- General cerebral edema.
- Increased level of cranial pressure.
- General blood flow disorders.
- Death of brain cells.
The mechanism of ischemia formation depends on the date of birth of the child, which is associated with age-related characteristics of the structure of the brain.
Provoking factors
Concomitant factors that can lead to the development of ischemia can be grouped into three groups:
- The course of labor. The risk of pathology increases if:
- bleeding occurred during pregnancy or during labor;
- emergency caesarean section;
- high temperature in a woman in labor;
- premature birth;
- low baby weight;
- turbidity of amniotic fluid;
- premature placental abruption;
- rapid labor activity.
2. The mother's condition can cause the development of ischemia in the child, especially when:
- the expectant mother suffers from neurological problems;
- there are pathologies in the functioning of the endocrine system;
- pregnancy at a later age;
- the presence of chronic pathologies in the mother.
3. The course of pregnancy is also very important: if preeclampsia or eclampsia was observed, then there is every chance of developing a pathology such as grade 2 cerebral ischemia in the newborn. The consequences may vary.
These factors are not a 100% guarantee of the development of pathology. Even intrauterine disorders do not always end with cerebral ischemia developing after birth; the consequences can be eliminated if the pathology is detected in time and all measures are taken.
Risk factors
Various vascular and neurological pathologies, problems with blood pressure (especially hereditary) in the mother should alert the doctor who is managing the pregnancy. Also, risk factors for cerebral ischemia in a child are:
- mother's age is more than 35 years;
- endocrine diseases;
- premature, prolonged labor;
- multiple pregnancy;
- late toxicosis;
- failure of the mother to follow a healthy lifestyle;
- exacerbation of chronic or acute diseases in the mother during pregnancy.
How does the disease manifest itself?
This pathology has varying degrees of manifestation. Stage 2 cerebral ischemia in newborns has serious symptoms, and immediate treatment is required. Here's what should alert doctors and mommy:
- Decreased muscle tone.
- Large pauses in breathing.
- Tendon reflexes are poor.
- Sluggish Moro reflexes.
The following syndromes are also noted:
- Syndrome of increased excitability, which manifests itself in crying for no reason, restless and superficial sleep, twitching.
- Hydrocephalic syndrome can be recognized by an increase in the size of the head and a large fontanel.
- Convulsive syndrome is present.
- If there is grade 2 cerebral ischemia in newborns, depression syndrome reduces sucking and swallowing reflexes, muscle tone is weakened, and strabismus may occur.
- The most serious syndrome is comatose. If it is present, the baby’s condition is serious, there are no reflexes, no reaction to external stimuli, low blood pressure, and breathing problems appear.
Symptoms
During diagnosis, attention is paid to the following indicators of the body:
- heartbeat;
- frequency and depth of breathing;
- the presence of conditioned and unconditioned reflexes;
- skin problems;
- muscle tone.
Patients with cerebral depression have disturbances in the listed factors. In the first minutes after the birth of the child, the doctor evaluates the indicated components - based on this, it can be assumed that there is a pathology.
The acute period of the disease includes a number of syndromes. With cerebral excitability syndrome, the patient experiences excessive motor activity, in which movements are chaotic and spontaneous. Tremors are noted in the chin, tongue, arms and legs. In cerebral depressive syndrome, on the contrary, motor activity is excessively suppressed. Unconditioned reflexes are sluggish.
Common symptoms of cerebral depression include noticeable trouble sleeping, startling, frequent crying, and problems with the sucking reflex. In children, the fontanel bulges and loss of coordination occurs. Frequent constipation, bloating, and disruption of the gastrointestinal tract are possible.
When lack of oxygen threatens the baby's life
If this pathology has grade 1, then it is considered a mild lesion, and doctors assess the condition of the newborn on the Apgar scale at 6-7 points. This degree is manifested by stimulation of the nervous system if the child was born at term, and depression in premature infants. This condition can be observed for 5-7 days.
Cerebral ischemia of the 2nd degree in newborns has more serious consequences; clinical convulsions, respiratory arrest, and floating movements of the arms may appear. If laboratory tests are performed, lesions of the brain parenchyma and disturbances in blood flow speed are detected.
If long periods of impaired motor activity, poor appetite, and impaired swallowing are observed, then an urgent consultation with a neurologist is necessary.
A severe degree can result in coma, which is life-threatening for the baby. Increasing symptoms increase the risk of developing hydrocephalus.
Characteristics and detection methods
Cerebral depression is a pathological condition in newborns, accompanied by impaired gas exchange and lack of oxygen.
There are problems with blood circulation in the brain. 70% of cases are associated with the occurrence of a blood clot in one of the vessels transporting blood to the brain. The formation of the disease begins during the period of intrauterine development of the fetus. At risk are premature babies with underdevelopment of the circulatory system. Previously, the diagnosis of “cerebral depression” was called “newborn asphyxia.” The clinical manifestations of the diagnosis are similar to depression in the following factors:
- the central nervous system is depressed;
- breathing and blood circulation are inhibited;
- problems with sleep and digestion.
Laboratory and instrumental research methods are used for diagnosis. After a blood test, patients are found to have an abnormal level of oxygen saturation in the tissues and brain. Thanks to neurosonography, it is possible to confirm or exclude pathological foci in brain tissue. Patients are prescribed an MRI to identify clear boundaries of the lesions. After a computed tomography scan, data on a decrease in tissue density is obtained. Newborn babies also undergo a Doppler encephalogram to establish the exact speed of blood flow in the middle cerebral artery.
How is the disease diagnosed?
Almost always, the manifestation of cerebral ischemia begins immediately after childbirth. If the disease is mild, then the symptoms may go away on their own, but a severe form may slightly weaken its symptoms, but only for a while, and then flare up again with renewed vigor. Therefore, if ischemia is suspected, various diagnostic procedures should be carried out, these include:
- Examination of the child for the presence of reflexes and assessment of the condition using the Apgar scale.
- General blood analysis.
- MRI if moderate or severe is suspected. This study helps to examine the structures of the brain and determine the extent of their damage.
- Ultrasound - allows you to detect cerebral edema or an area of hemorrhage.
- An electroencephalogram is mandatory for newborns with severe disease.
If a diagnosis of grade 2 cerebral ischemia in newborns is suspected, treatment will be prescribed after all studies.
Diagnostics
The disease is usually diagnosed within the first few hours.
The presence of pathology is indicated by deviations in checking reflexes and a general blood test . Typically, the analysis shows an increased level of carbon dioxide in the body.
If obvious symptoms of a serious illness are detected magnetic resonance imaging , as well as electroencephalography , which reveals hidden convulsions and other abnormalities in the functioning of the brain.
Main goals of ischemia therapy
If the diagnosis is confirmed after all the studies, then measures begin to maintain normal temperature, humidity, and protection from external irritants.
Therapy in newborns should be as less aggressive as possible. It pursues the following goals:
- Provide adequate ventilation.
- Support hemodynamics.
- Constantly monitor the biochemical parameters of the tests.
- Prevent seizures.
Diagnosis and treatment of disease in infants
Diagnosis of cerebral ischemia in a newborn is carried out after the following examinations:
- Complete blood count (erythrocyte count and leukocyte formula).
- Urinalysis (protein content, leukocytes).
- Neurosonography is an ultrasound examination of the skull through the fontanelles, searching for asymmetrical parts of the brain, enlarged cavities and spaces, and formations.
- Ultrasound examination of blood vessels using Doppler methods. Additionally, acceleration or deceleration of blood flow through the main vessels is detected.
- EEG, which detects changes in the activity of the brain.
- Magnetic resonance imaging is rarely used due to the need for anesthesia. It is used only in cases of suspected brain developmental defects.
- Computed tomography, which is used if bleeding into the cranial cavity is possible.
The treatment method is chosen by the doctor based on the patient’s condition. In the acute period, methods are aimed at supporting life and include:
- artificial air circulation;
- maintaining blood salt balance;
- drugs against involuntary muscle contractions.
After the end of the acute period, the following groups of drugs are used:
- improving blood flow through vessels and intracellular metabolism.
- diuretics that lower blood pressure;
- restoration of the balance of metal ions;
- nootropics to improve the functioning of the central nervous system.
Also used:
- massage therapy;
- gymnastics;
- hydrotherapy;
- complex of physiotherapeutic measures.
Preventive actions
Methods for preventing cerebral ischemia concern the mother of the child.
Activities include:
- increasing time spent in fresh air;
- getting rid of bad habits;
- avoiding stress and fatigue;
- adherence to the regime and consumption of foods containing vitamins;
- no need to overload the body with loads;
- monitor blood pressure;
- control the level of respiratory pigment;
- prevent obesity;
- prevent infections.
Where is cerebral ischemia treated?
We have already found out that this disease has several degrees, which differ in severity. Therapy will depend entirely on the symptoms.
- If a mild degree is observed, then even in the maternity ward, doctors take the necessary measures and discharge the baby. Subsequently, it is recommended to visit a neurologist and get the necessary advice. Most often, massage and adherence to a daily routine are recommended.
- Cerebral ischemia of the 2nd degree in newborns, what it is has already been found out, requires treatment in the maternity hospital and it continues in the hospital, since the symptoms are more serious.
- In severe cases, the child is immediately placed in intensive care after birth.
Degrees of impairment
The severity of clinical symptoms, the direction of the therapeutic course, as well as the number of complications depend on the degree of brain disorders.
Functional and structural changes of the brain at different stages of the pathological process
There are three degrees of severity of cerebral ischemia, which have different intensity of manifestations:
- Easy. It is temporary, since after stabilization of the nervous system, ischemic disorders occur without neurological consequences. The condition is characterized by a slight increase in the concentration of carbon dioxide and a decrease in the oxygen saturation of the body. The activation of compensatory mechanisms is observed when the oxygen deficiency is replenished by increasing blood flow.
- Moderately heavy. Intrauterine hypoxia provokes an abnormal heart rhythm, leading to the development of asphyxia, which lasts about 60 seconds after birth. The condition manifests itself as periods of excitement, abruptly alternating with depression of the nervous system. Convulsive seizures of a short-term nature are observed.
- Heavy. It is formed as a result of a violation of intrauterine circulation, when an insufficient amount of nutrients and oxygen reaches the fetus. After birth, the child experiences a decrease in brain activity, progressing to a coma. An increase in intracranial pressure leads to inhibition of the respiratory and cardiac systems, as well as to a disorder of metabolic reactions.
Treatment methods for ischemia
This pathology is characterized by the fact that there is no conservative treatment for it, since dead brain cells cannot be replaced with viable ones. But timely prescribed maintenance therapy allows you to stop the progression of the disease and makes it possible to rehabilitate.
If the pathology is severe, it is visible immediately after birth. In such cases, do the following:
- Artificial ventilation is performed to help restore spontaneous breathing. After this, the baby’s condition is constantly monitored.
- Cardiac supportive care is needed to prevent cardiac dysfunction, Dobutamine.
- Phenobarbital and Phenytoin will help prevent seizures.
- One of the new methods is hypothermia. It is believed to reduce the rate of brain cell death. But it must be carried out only under the supervision of a doctor. If the temperature is lowered by several degrees, the child is gradually warmed up.
If the disease is mild, then it is enough to take medications that will improve blood circulation in the brain and prevent further damage to neurons.
If there is a threat of developing hydrocephalus, Furosemide and Manitol are prescribed.
Stages 2 and 3 of the disease threaten more serious consequences, so it is important to take all measures and prescribe therapy that will prevent the development of complications of ischemia. They can manifest themselves as mild, for example, attention deficit, or more serious, up to dementia and disability.
Symptoms
The clinical picture of cerebral ischemia in infants is determined by the intensity of symptoms, the location of neuronal damage and the severity. The first signs of pathology can be determined by assessing reflex activity, taking into account the physiological maturity of the baby.
A characteristic sign of pathology is excitation of the central nervous system
The first degree disease is manifested by the following symptoms:
- muscle tone disorder;
- involuntary contractions of the lower and upper extremities;
- shallow restless sleep;
- constant crying and screaming;
- strengthening reflexes.
In prematurely born children, the course of the disease is dominated by depression of the nervous system, which is manifested by a decrease in basic reflexes, a decrease in motor activity and lethargy.
At the second stage, the following symptoms are distinguished:
- weakness of the baby during feeding;
- frequent regurgitation;
- disturbances in intestinal function;
- interruptions in the functioning of the myocardium;
- stopping breathing during sleep;
- local cyanosis of the skin;
- decreased reaction of the pupils to a light stimulus;
- sluggish sucking reflex;
- decreased muscle tone;
- constant shuddering of the child;
- convulsive seizures.
A newborn's skin takes on a marbled color.
In severe condition of the child, the appearance of nystagmus, strabismus, vomiting, complete cyanosis of the skin, and arrhythmia are observed.
The third stage of the disease is characterized by the following symptoms:
- lack of basic reflexes;
- convulsive seizures, long-term, at frequent intervals;
- cramps are replaced by a decrease in muscle tone;
- state of complete immobilization;
- respiratory dysfunction;
- decreased heart rate;
- pupils are dilated and do not respond to light;
- increased intracranial pressure;
- decreased blood pressure;
- sluggish bowel activity;
- lack of urination.
The extreme degree of brain damage is manifested by severe depression of the central nervous system, up to the development of coma.
Komarovsky's opinion on the disease
If there is grade 2 cerebral ischemia in newborns, Komarovsky believes that drug therapy gives a result, but not what everyone expects. It is very important in the acute period, when the impact of the damaging factor on the brain is observed, but, as a rule, pathology is detected much later, when the so-called recovery period for the brain begins. At this time, massage and physiotherapeutic procedures will be more effective, which will help the brain recovery process. Dr. Komarovsky believes that all neurological manifestations in newborns are associated with brain immaturity, which will gradually disappear if there are no serious chronic pathologies.
-th degree
In this case, there is an implicit appearance of neurological disorders. With grade 1 cerebral ischemia, patients note the appearance of:
- Headaches.
- General weakness, which gradually develops into severe fatigue.
- Decreased concentration.
- Frequent insomnia.
- Memory impairment.
- Emotional instability.
However, these symptoms are not specific. Because of this, it is very difficult to timely diagnose the appearance of grade 1 cerebral ischemia. Many people associate all these symptoms with overwork, so they rarely seek medical help. However, you need to understand that this stage of pathology is amenable to the fastest and most effective treatment.
Consequences of cerebral ischemia
Currently, medicine is at a level of development that makes it possible to avoid the serious consequences of cerebral ischemia, but provided that the diagnosis was identified in a timely manner. Many children who have suffered from this disease experience rapid fatigue, hyperactivity, and problems with remembering, which can affect their performance at school. Even when there are consequences (if a diagnosis of grade 2 cerebral ischemia in newborns is made), reviews from mothers confirm that they can be dealt with if you consult a doctor and take the necessary medications.
With their help, you can significantly influence the child’s excessive activity, improve his memory and attention, and accordingly, his performance at school will also improve. It is very important to find a competent specialist who will help cope with the accompanying symptoms.
The most severe consequences of cerebral ischemia are cerebral palsy and epilepsy. But this most often happens in the most severe cases and when the diagnosis is not made in a timely manner.
Assessing the degree of complications
Ischemic disorders provoked by oxygen deficiency lead to the death of brain cells, which creates conditions for the formation of irreversible neurological disorders, the severity of which depends on the localization of structural changes.
As a rule, cells located in the pyramidal zone, cerebellar cells, ventrolateral neurons, midbrain nuclei, and stem neurons are affected.
With large-scale ischemic damage to brain cells, their complete death occurs, which leads to death.
The most common complications are decreased memory and mental performance
The consequences of ischemic disorder include the development of the following conditions:
- epilepsy;
- one-sided blindness;
- impaired mental function;
- motor function disorder.
Full assessment of complications occurs at the age of 3 years.
What parents can do for their child
Even the 2nd degree of pathology is not a death sentence. After completing a course of drug therapy, the recovery period begins. At this time, parents play a big role; it often depends on them how severe the consequences of the pathology will be. In order for the baby’s development to return to normal, parents must:
- Visit a neurologist regularly with your child.
- Give the baby medications prescribed by the doctor.
- Closely monitor psychomotor development in order to promptly notice deviations.
- Strictly follow the recommendations for your daily routine.
- If the child has increased excitability, then provide him with a calm environment and eliminate sources of noise.
- Get outdoors more often.
- Take massage courses.
- Do exercises with your baby; a set of exercises may be recommended by your doctor.
Any neurological problems can be solved, because the child’s nervous system is not yet fully formed, it is quite flexible and capable of recovery, so one should not give up. Even with a diagnosis of grade 2 cerebral ischemia in newborns, the consequences may not be so dire. The care and love of parents, and, of course, the help of doctors, will certainly work a miracle, and the child will not lag behind his peers.
How to treat
There are no specific measures for the treatment of cerebral ischemia in newborns. Dead brain structures cannot be restored. Treatment is aimed at preventing the progression of hypoxic changes and rehabilitation of the child.
If in the first two minutes the baby does not breathe on his own, then he is resuscitated: an endotracheal tube is inserted and mechanical ventilation is performed. If the lesions are minimal, then under the supervision of a doctor the child breathes alone 2.5-3 minutes after the trachea has been intubated.
In case of prolonged intensive care, the baby is transferred to the appropriate department, where all his vital signs are under the control of medical staff.
Convulsive manifestations are relieved with Phenobarbital, Phenytoin and other means. The doctor selects an individual dose for the patient, and the seizures are stopped.
With the help of Dopamine and Dobutamine, the cardiac activity of a small patient is corrected.
There is evidence that a hypothermic state prevents the death of brain cells, stopping necrotic changes. This therapy is also supervised by specialists, and the patient is then gradually warmed up.
Treatment
Therapy is carried out taking into account the severity of damage to brain structures, leading symptoms, the child’s condition and the results of a diagnostic examination. Main therapeutic measures:
- Control of vital functions.
- Correction and maintenance of adequate body temperature.
- Ensuring sufficient oxygenation of the lungs.
- Creating conditions for sufficient blood circulation and homeostasis.
- Prevention of hemorrhages and infections.
According to indications, the doctor prescribes drugs to correct convulsive syndrome, acid-base status, hypoglycemia (decreased glucose concentration), hypocalcemia (decreased calcium concentration), hypomagnesemia (decreased magnesium concentration). In parallel, treatment is carried out aimed at normalizing cerebrospinal fluid dynamics and eliminating cerebral edema.
The use of pharmaceuticals with vasoactive effects and nootropic drugs is almost always unjustified. Anticonvulsants are indicated if there are at least 3 episodes of seizures or if the duration of a single episode exceeds 3 minutes.
Non-drug treatment methods: laser therapy, dry immersion (simulation of weightlessness conditions to simulate a child being in water), aromatherapy and music therapy, psychosensory stimulation, massage, therapeutic exercises, exercises in water. Massage and exercise therapy as part of complex treatment for cerebral ischemia are prescribed after the end of the acute period to regulate skeletal muscle tone and improve motor function.