The world has known about the disease, which official medicine calls “angina pectoris,” for quite a long time. The average person in our country has long known this disease under the name “angina pectoris”.
A couple of centuries ago, there was a fashion for illness in aristocratic circles. Diseases such as gout, angina pectoris and almost all types of neuroses were considered “aristocratic”. Having reached a certain age, representatives of the wealthy classes once sat down in a chair and naturally played the role of a sick person. It was necessary because it was fashionable. It's fashionable to be healthy these days. All the efforts of modern man are aimed at preventing diseases and their timely treatment. This is due to his desire to succeed in life, to achieve more than others.
The attitude is good, but in the pursuit of ideals and the realization of their own dreams, in exhaustion of strength, it is these people who more often become victims of various diseases .
According to statistics, about 20% of our citizens get angina pectoris (angina pectoris) before they barely overcome the age barrier of 50-55 years. Of these, about 65% are men. Doctors note that over the past decades there has been a trend toward “rejuvenation” of angina pectoris, when it affects younger people and even children.
What kind of disease is this and how is it dangerous?
Angina pectoris is also called “angina pectoris”. This name was first proposed in 1768 by the English physician William Heberden, when he described attacks of angina in his patients: “as if their heart was being squeezed very strongly and suffocated from the inside.”
The most dangerous consequence of long-term angina is myocardial infarction, which ranks first among all causes of death.
Mortality risk for angina pectoris: up to 10% per year.
Pain with angina pectoris develops due to the fact that the heart muscle experiences a sharp lack of oxygen. This is called myocardial ischemia. This occurs due to the narrowing of the blood vessels supplying the heart. In approximately 90-95% of cases, the cause of this is atherosclerosis - the deposition of cholesterol particles on the inner layer of blood vessels and the formation of plaques. The insidiousness of atherosclerosis is that a person’s well-being changes when the lumen of the arteries narrows by more than 50%. Before this he feels quite healthy.
Angina pectoris is a clinical syndrome that is recognized as the most common form of coronary heart disease (CHD). Its prevalence ranges from 30 to 40 thousand per 1,000,000 people. It mainly affects people over 40 years of age, most often men (ratio to women 2.5:1). This division is explained by the fact that female sex hormones have the ability to slow down the development of atherosclerosis. Therefore, the incidence of coronary artery disease among postmenopausal women does not differ from that in men. You can read about gender differences in the course of ischemia here.
Situations that cause the myocardium to require more oxygen than usual predispose to the development of angina. These include high blood pressure (especially hypertensive crisis), rhythm disturbances accompanied by increased heart rate (tachyarrhythmias), various heart defects, diabetes mellitus, anemia, physical inactivity, obesity, bad habits - smoking, alcohol abuse, etc.
High concentrations of cholesterol in the blood are considered one of the main risk factors for coronary artery disease. If your close relatives suffered from coronary heart disease, then the likelihood that you will develop it increases significantly.
In more rare cases, the cause of angina is spasm of the coronary arteries, a congenital anomaly in the structure of the vessels supplying the heart, etc. In ICD-10, angina pectoris is coded I20.0.
Complications
Coronary heart disease and angina pectoris, as a special case, have common features. Chronic heart failure is a clear consequence of fatigue. When the disease occurs, the legs swell, shortness of breath and heaviness in the chest appear.
Changes in pressure are natural; wear and tear of the heart muscle is directly proportional to the increase in pressure. The end point is a heart attack, but it can also occur out of nowhere.
Prerequisites for heart attack
Spasm of the arteries (tubular organs that supply the heart), atherosclerosis, plaques, the result of a clot getting stuck in the coronary arteries. In any case, the result is the same - a heart attack, the heart loses its ability to work adequately.
Also, each attack will entail such serious illnesses as:
- arrhythmia;
- tachycardia;
- ventricular block;
- heart failure;
- shock;
- inflammation of the heart;
- blood clots
If you witness such a condition, immediately call an ambulance and provide assistance to the patient and create conditions of peace.
Symptoms
The main clinical signs of angina pectoris are attacks of pain in the middle of the chest, which are felt as severe squeezing, burning or squeezing. However, this is not the only place where pain occurs. It can radiate to the left arm, neck, shoulder, lower jaw, under the shoulder blade, and upper abdomen. This is a kind of “calling card” of ischemic pain, separating it from all other types. Often these places hurt much more than the heart itself. I have seen patients who were seen by orthopedic traumatologists with a diagnosis of arthrosis of the shoulder joint, although in fact it was angina pectoris.
The duration of the attack varies from 1-2 to 20 minutes. Most often, pain is triggered by physical activity (running, lifting weights, climbing stairs) or emotional stress.
Depending on the degree of stress that causes pain, angina is divided into so-called functional classes (FC) - from 1 (when pain occurs only with very intense muscular work) to 4 (pain can develop even with the slightest movement or at rest).
A distinctive feature of pain during angina pectoris is its disappearance after the person stops exercising or takes Nitroglycerin. In some cases, instead of pain, severe difficulty breathing (shortness of breath) or cough appears.
Forecast
Determined by the stage of the pathological process. The first functional class is curable in 90% of cases.
Starting from the second, total normalization is no longer possible.
Mortality is distributed as follows:
- II - 25%,
- III - 45%,
- IV - 85%, in the future 5 years for the last phase - 100%.
The numbers may change taking into account negative and positive factors: age, gender, general health, lifestyle, heredity and other factors.
How to recognize an angina attack
In most patients, an attack of angina pectoris does not occur “out of the blue.” It must be preceded by some action that increases the myocardial need for oxygen - physical or emotional stress. Pain can also occur when going outside in cold weather, or when the body bends sharply while putting on shoes. Even ordinary overeating leads to the fact that blood flow is redistributed in favor of the digestive system, thereby depleting other organs of blood, incl. and heart.
In my practice, I have met patients in whom the smell of tobacco smoke could cause heart pain.
Often, during an attack, a person becomes covered in cold, sticky sweat, becomes dizzy, and feels nauseous. Some people experience anxiety and fear of death. In such situations, it is very important to distinguish angina pectoris from panic attacks, in which “neurotic symptoms” come first. However, you must always remember that these attacks themselves can cause angina.
If the pain lasts longer than 20 minutes and persists despite taking a nitroglycerin tablet or spray, you should call an ambulance.
You can find out what you need to do during an attack of angina pectoris and how to relieve it at home here.
Features in men
Males are characterized by the so-called typical clinical picture of angina (burning/pressing pain behind the sternum, developing after physical work). However, pain often makes itself felt too late, and its intensity does not correspond to the degree of damage to the coronary arteries. Those. slight discomfort in men occurs against the background of a pronounced decrease in the lumen of blood vessels.
In other words, the appearance of angina in a man indicates advanced atherosclerosis.
I constantly have to diagnose IHD in men only when they are admitted to the cardiac intensive care unit with myocardial infarction.
Risk factors
There are also predisposing factors. Patients with at least one of these are considered to be at increased risk of developing angina pectoris:
- Being male.
- Age 45+. With each subsequent year, the likelihood only gets worse. Changing your lifestyle will help reduce your risks.
- A history of a group of abnormalities: hypertension, diabetes mellitus, hyperthyroidism, myocardial hypertrophy. They are dangerous individually, but in combination they pose an even greater threat.
- Physical nature of the work.
- Frequent stress.
All reasons are evaluated in the system.
Specifics in women
Unlike men, in women, on the contrary, the pain syndrome is more pronounced with completely satisfactory vascular patency.
I also often observe atypical symptoms of an angina attack in women, i.e. Instead of pain in the heart, the patient experiences a sharp lack of air (asthmatic form), or discomfort in the epigastric region (gastralgic version), which makes it much more difficult to recognize angina pectoris. The nature of pain in women also does not always correspond to the classic one - it can be, for example, stabbing.
What types of angina are there?
Depending on the severity, nature of the course, the cause underlying the mechanism of development of pain and the approach to therapy, the following types of angina are distinguished:
- Stable (angina pectoris) is the most common type and is divided into FC.
- Unstable - exacerbation of angina pectoris, or pre-infarction condition. The pain appears even with minimal exertion and does not stop even after taking Nitroglycerin. The process of thrombus formation occurs, but not sufficiently to cause necrosis of the heart muscle. It is considered an emergency condition and its symptoms are indistinguishable from myocardial infarction, but can lead to it. There are the following types of unstable angina:
- For the first time, the appearance of symptoms of angina pectoris in a person who has not previously experienced such pain. Requires special attention, since proper treatment determines whether the pathology will become stable or progress;
- Progressive - attacks become longer and more frequent, Nitroglycerin helps less and less (transition from FC I to III or IV in 2 months);
- Post-infarction – the occurrence of attacks no later than 2 weeks after myocardial infarction. This is the most unfavorable form, as it is characterized by a high probability of death;
- Vasospastic (variant, spontaneous, Prinzmetal's angina) is angina caused not by atherosclerotic stenosis of the coronary arteries, but by their spasm, i.e. strong contraction of vascular muscles. This type usually occurs in young men. Pain can appear at any time and has nothing to do with physical activity. Most often develops at night or early in the morning. A series of attacks (from 2 to 5), following one after another with an interval of 10 minutes to 1 hour, are specific to this type.
Separately, there is a special type of angina pectoris - cardiac X syndrome, or microvascular angina, in which there are typical attacks of pain during physical effort with ECG signs with normal or slightly changed coronary arteries (vascular patency more than 50%). It is observed mainly in women with neurotic disorders during menopause and premenopause (40-50 years). The exact cause of its occurrence is still unknown.
It is assumed that a decrease in the concentration of female sex hormones (estrogens) leads to spasm of microvessels. It is also important to increase the threshold of pain sensitivity in anxiety and depression.
A distinctive feature of the symptoms of cardiac syndrome X is that attacks of angina pectoris disappear after stopping the exercise, resting or taking Nitroglycerin, but this happens much longer than with other types of angina.
Causes
An angina attack begins suddenly and does not stop until an ambulance is called.
There are many reasons for an attack; it can be caused by heavy meals, overeating, obesity, anxiety, temperature changes, stress, drinking alcohol on an empty stomach and smoking.
According to statistics from the health center, the causes of angina are:
- smoking - quit smoking, smoking narrows blood vessels (tubular organs);
- do not overeat, elevated cholesterol levels are a sure sign of beginning changes in blood vessels;
- quit smoking, take measures to lower your blood pressure, reduce high cholesterol levels in your blood. Start with exercise. Diabetes worsens the course of the disease.
IHD (coronary heart disease) and angina pectoris, as its special case, begins with a narrowing of blood vessels. The blood nourishes the heart muscle less effectively, a feeling of general weakness of the body begins, the formation of plaques on the walls of the tubular organ, stress and constant overwork aggravate the situation.
Unpleasant painful sensations arise from the fact that starving pain receptors react to the lack of oxygen with impulses.
This condition is called an attack. Tubular organs lose elasticity, and increased pain begins to occur from normal stress. This condition cannot be corrected and is called chronic heart failure.
Stages of development and progression of the disease
It all starts with a routine state of tension, doctors call this condition angina pectoris, the patient increasingly resorts to pills for heart pain, the person’s loved ones are obliged to measure his blood pressure.
A feeling of heaviness in the chest is a sign that medical help is needed. The condition will not go away, as people say, you cannot expect angina pectoris to go away on its own, this disease is insidious, an attack overtakes a person on the staircase, at work, in transport.
Diagnostics
To diagnose angina pectoris, I use the following research methods:
- blood tests;
- electrocardiography;
- ECG with stress;
- daily (Holter monitoring) ECG;
- echocardiography;
- myocardial scintigraphy;
- coronary angiography.
For all patients with attacks of angina pectoris, I prescribe a biochemical blood test to determine the concentration of total cholesterol and its fractions - low and high density lipoproteins. They are also called “bad” and “good” cholesterol. I also check everyone's glucose levels to check for diabetes.
The further examination algorithm has some nuances for different forms of angina. Let's look at these methods in more detail.
In unstable angina, blood is first taken to determine enzymes that indicate necrosis (death) of an area of the heart muscle. These are so-called cardio-specific enzymes. These include troponins I and T, MB fraction of creatine phosphokinase, myoglobin, lactate dehydrogenase. With unstable angina, they are within the normal range or slightly elevated. Their analysis is necessary to exclude myocardial infarction (MI).
Since clinically unstable angina and heart attack are indistinguishable from each other, in practical medical practice they are united by the term “acute coronary syndrome” (ACS).
Electrocardiography is the main instrumental method for diagnosing angina pectoris:
- Stable - a typical change on the ECG during a painful attack is a decrease in the ST segment by more than 1 mm, sometimes a negative T wave. Since the cardiogram can be normal at rest, to confirm the diagnosis, I prescribe an ECG with a stress test, i.e. during physical exercise - treadmill test (walking or running on a treadmill) and bicycle ergometry (riding an exercise bike).
- Unstable - characterized by a decrease in the ST segment, but its rise is also possible, which in most cases indicates the development of myocardial infarction.
- Vasospastic – a specific sign is ST segment elevation at the time of the attack. Conducting stress tests is pointless, since the pain is in no way related to physical effort and occurs at night or early in the morning. Therefore, if this form is suspected, I prescribe Holter ECG monitoring. If the results are questionable, I use provocative tests that cause spasm of the coronary arteries - ergometrine (intravenous administration of the vasoconstrictor drug Ergometrine), cold (lowering the hand to the middle of the forearm for 5 minutes in water at a temperature of + 4 degrees), hyperventilation (the patient breathes intensely and deeply for 3 -4 minutes). If the result is positive, pain appears along with ST segment elevation on the ECG.
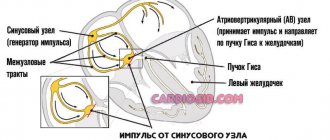
Often the listed changes in the ECG are accompanied by heart rhythm disturbances - supraventricular tachycardia, atrial fibrillation, slowing of atrioventricular conduction, bundle branch block, etc.
Echocardiography (Echo-CG, ultrasound of the heart) allows me to evaluate morphological changes - myocardial contractility, the degree of hypertrophy and expansion of the chambers, check the structure of the valves, the presence of aneurysms and intracardiac thrombi.
Myocardial scintigraphy is a study of the state of blood flow in the myocardium using a radioactive drug (thallium-201 or technetium-99-m). I use this method in patients with stable angina who have severe heart rhythm disturbances that make it impossible to see changes in the ST segment.
The essence of scintigraphy: the patient is injected with a drug, he begins to perform physical activity on a treadmill or bicycle ergometer, and images are obtained using a special gamma tomograph. Areas of impaired blood circulation (ischemia) have a faint glow.
Coronary angiography is the gold standard for diagnosing coronary artery disease, allowing to assess the patency of the coronary arteries. It can also be used to determine whether a given patient needs surgical intervention or whether drug therapy alone can be used.
Stopping an attack
If a person is overtaken by angina pectoris, first aid must be provided urgently. The following will help stop the disease:
- Everyone knows nitroglycerin as a panacea for heart disease, although aspirin can be used with equal success. Yes, it has been proven that it is toxic, but what to do? Validol is ineffective; after taking aspirin, you must take a stationary, horizontal position and be in a room with fresh air.
- Patients are shown a relaxing massage, it helps to quickly recover from an acute attack, sometimes patients do self-massage, they need to massage areas of the face and neck close to the heart, that is, on the left side. Hand massage is also effective, especially if the attack lasts a long time.
- Vasospasm affects the brain, severe pain appears in the head, painkillers are taken according to the doctor’s indications, usually analgin, if the pulse exceeds 120 beats, you need to take anaprilin.
- If aspirin is in powder form, pour it into a glass and fill it with warm water (not cold, cold intensifies the spasm). Severe vasoconstriction, accompanied by pallor and cold sweat, indicates a decrease in blood pressure; in this case, you should not drink nitroglycerin.
- Relief of an attack at rest and in irritation is different, did the attack occur while lying down? Raise the person so that the legs are lower than the head, inversely proportional to the position when fainting.
The role of smoking in the course of the disease is significant - nicotinic acid itself dilates blood vessels, but during smoking the vessels narrow. The mystery lies in the metabolism of cells, nicotine and tar are poisons that clog tubular organs, and nicotinic acid separately is vitamin PP, which has a positive effect on the body.
Of the substances that cause pleasure, namely, harmful fats, psychoactive substances and alcohol, there is not a single substance that has a positive effect on health. Accept the idea that everything that is pleasant is harmful.
If there is a desire to restore the functioning of the heart muscle and the condition of the blood vessels, you need to start cleansing the body of waste and toxins; with an unhealthy diet and an abundance of bad habits, even the smartest and most talented doctor will not help a person; if you are unlucky, even a surgeon will not be able to save a life. It all depends on the patient.
How and with what they are treated
Angina pectoris requires competent and comprehensive treatment, including the use of medications, surgical interventions, and lifestyle correction.
I treat angina pectoris using the following medications:
- beta-blockers (Bisoprolol, Metoprolol) – reduce the myocardial oxygen demand and improve its blood circulation;
- calcium channel blockers (Diltiazem, Verapamil) - have a similar mechanism of action. I resort to them in case of contraindications to beta blockers (for example, with severe bronchial asthma);
- antiplatelet agents (Acetylsalicylic acid, Clopidogrel) – prevent the “gluing” of platelets, thereby preventing the formation of blood clots;
- anticoagulants (unfractionated, low molecular weight heparin) – also suppress the process of blood clot formation by affecting plasma coagulation factors;
- statins (Atorvastatin, Rosuvastatin) - help slow down the growth of atherosclerotic plaques by lowering cholesterol levels in the blood;
- nitrates (Nitroglycerin, Isosorbide dinitrate) and dihydropyridine calcium channel blockers (Amlodipine, Nifedipine) - cause dilation of the coronary arteries, which increases blood flow to the myocardium;
An important point is that nitrate tablets should not be swallowed, but placed under the tongue.
In the hospital
It is almost always worth starting treatment for angina in a hospital, especially for unstable forms. When a person is admitted to the hospital, I use the following drug therapy regimens depending on the type of angina:
- Stable – beta-blocker, antiplatelet agent, statin. Nitrates only during an attack, taking into account that the break between doses should be at least 10-12 hours. With more frequent use, the effectiveness of nitrates decreases several times.
- Unstable - beta-blocker, necessarily 2 antiplatelet drugs, an anticoagulant, a narcotic painkiller, a statin.
- Vasospastic - dihydropyridine calcium channel blocker, nitrate, antiplatelet agent.
Cardiac syndrome X deserves special attention. Standard therapy is effective in only half of patients with this diagnosis. To the treatment of these patients, it is necessary to add antidepressants, sedatives, hormone replacement therapy with estrogen, and aminophylline. Psychotherapy can also help.
If a patient with stable or unstable angina has severe atherosclerotic damage to the coronary vessels, as well as a high cardiovascular risk (old age, diabetes mellitus, rapid progression of the disease, increased cholesterol and blood pressure, etc.), surgical treatment is indicated for him. .
There are two types of operations:
- coronary artery bypass grafting (CABG);
- percutaneous transluminal balloon coronary angioplasty (PTCA), or stenting.
With CABG, a fistula (shunt) is created between the internal mammary and coronary arteries. This method is used in cases of multiple damage to the heart vessels by atherosclerosis.
During PTCA, a metal stent (a spring-shaped frame) is inserted into the artery, which widens the lumen of the vessel. Drug coatings are sometimes used. The rationale for choosing PTCA is a hemodynamically significant decrease in patency (less than 50%) in one artery. Often, stenting is performed in parallel with coronary angiography.
First aid for the development of an attack
Regardless of what episode of angina pectoris occurs, you should call the emergency room. You can never tell in advance how an attack will behave.
Before the doctor arrives, the algorithm is as follows:
- Open a window or window to provide ventilation to the room.
- Remove tight jewelry, loosen the collar of clothing. This is necessary in order not to provoke a reflex drop in heart rate and blood pressure. Otherwise, fainting is possible.
- Calm down, pull yourself together. If you have tranquilizers, take one tablet. If you don't have it, motherwort and valerian will do, but not an alcohol tincture.
- Pain is relieved with Nitroglycerin. At the very least, the intensity of the symptom will decrease significantly.
- Sit down and wait for the team of doctors to arrive.
Next, the moment of hospitalization or on-site assistance is decided. If there is a suspicion of a heart attack, the question of transporting the patient to the cardiology department is not even raised.
Clinical case
I recently saw a classic case of angina. A 62-year-old man was delivered to the emergency cardiology department by an ambulance team. According to the doctor, the patient, in a state of complete rest, developed severe squeezing pain in the heart area, radiating to the left arm. Taking Nitroglycerin did not relieve the pain. The duration of the attack is about 30 minutes. An ambulance was called. The medical staff took an ECG - a decrease in the ST segment was recorded, tablets of Acetylsalicylic acid, Clopidogrel and Metoprolol were given, and low molecular weight heparin was administered intravenously. Upon admission to the hospital, blood was taken for cardiac enzymes. Since the patient was experiencing unbearable pain, I prescribed him a narcotic painkiller - Promedol. Coronary angiography was performed. Conclusion: stenosis of the right coronary artery – 75%. PCI with stenting was performed. Cardiac enzyme results ruled out myocardial infarction. Clinical diagnosis: “IHD. Unstable angina IIIB according to Braunwald." For continuous use, I was prescribed Acetylsalicylic acid, Clopidogrel, Metoprolol, Rosuvastatin and Isosorbide mononitrate for pain.
Treatment
Therapy is carried out in a hospital at an early stage, as soon as the disease is identified. Then on an outpatient basis. The nature of the impact depends on the origin of the condition and the stage of its development.
Angina pectoris of the first functional class requires the use of medications for 3-5 months. Then continuous monitoring is carried out. As necessary, the course is repeated every few years. In other cases, therapy is lifelong.
The list of medications and methods of conservative care are determined by the ABCDE scheme, step by step:
- Antithrombic drugs. Aspirin Cardio. Restores blood fluidity, normalizes its rheological properties.
- Nitroglycerin + beta blocker. The names are determined by the doctor.
- Statins to combat atherosclerosis. Atoris or others.
- Low fat diet.
- Cardioprotectors. Mildronate and analogs.
Antiarrhythmic drugs, such as Hindin, are added as needed.
Surgical treatment is carried out according to indications. As an option, for abnormalities in the development of cardiac structures, heart defects, congenital and acquired, advanced atherosclerosis with occlusion or stenosis of the coronary arteries.
The essence of therapy is always approximately the same: replacing the affected area of the vessel with an artificial prosthesis, stenting, ballooning - that is, expanding the lumen mechanically to ensure blood flow.
For your information:
Advanced forms are almost impossible to correct, so there is no point in starting the pathology.
Treatment of angina pectoris is predominantly medicinal. Makes sense only in the early stages.
It would also be a good idea to change your lifestyle:
- Quitting smoking, alcohol, drugs, and self-administration of medications without consulting a doctor.
- Normalization of sleep patterns. 8 hours per night.
- Minimal physical activity (walking, swimming, no more).
- Diet correction. The patient can create the menu independently; he or she should focus on treatment table No. 10.
- Avoid stress whenever possible.
angina pectoris cannot be eliminated with pills alone. It will require effort from the patient himself.
After discharge
Basically, drug treatment does not change after discharge from the hospital. The patient must take most medications for life. You can read more about medication regimens and dosages here. Some drugs are not indicated for long-term use by the patient, for example, anticoagulants, except when they are necessary for the treatment of concomitant diseases.
If the patient has undergone PCI with stenting, he must take 2 antiplatelet drugs (Acetylsalicylic acid and Clopidogrel) for at least 1 year. Next, he needs to switch to a constant intake of 1 medication - if he does not have a gastric ulcer or duodenal ulcer, then Acetylsalicylic acid, if he does, then Clopidogrel.
To prevent the development of ulcers, I recommend that my patients add drugs that reduce the formation of hydrochloric acid in the stomach - Omeprazole, Pantoprazole.
Folk remedies
You can treat angina with folk remedies. It is necessary to use a mixture of dried apricots, prunes, honey, lemon, walnuts and raisins. A decoction of birch buds, chamomile flowers, St. John's wort and immortelle is useful. They use tricolor violet tea. Use a mixture of ten heads of garlic, 10 lemons and 1 kilogram of honey.
Folk remedies for angina pectoris are effective only with long-term use. The nature of the disease is purely personal and appears only when the vessels are 60% clogged with cholesterol plaques. Therefore, every person should periodically check their cholesterol and maintain it at normal levels. angina pectoris can go away without any complications if its signs are detected in time and treated.
Expert advice: what you can and cannot do for angina pectoris
I always tell my patients: in order for the treatment to be successful and maintain its effect, you need to follow certain rules and adhere to the following recommendations.
- bad habits - you definitely need to quit smoking, because... smoking is one of the main factors in the progression of atherosclerosis. It is also necessary to limit the consumption of alcoholic beverages to 2-3 glasses of wine per week;
- nutrition - it is advisable to reduce in your diet foods high in animal (saturated) fatty acids (lard, fatty fried meat, smoked meats, butter, etc.), while increasing the amount of foods rich in unsaturated (omega-3.6) fatty acids (fish, vegetables, vegetable oil). Also, the patient’s daily menu should contain fruits, nuts, cereals, and grains. Patients with diabetes need to significantly reduce the percentage of easily digestible carbohydrates (sweets, chocolate, pasta, pastries, cakes, buns, etc.). More complete information about nutrition for angina pectoris here;
- blood pressure control - it is achieved by daily measurement of blood pressure, limiting salt to 3 g per day, constantly taking medications to lower it in compliance with the prescribed dosages and frequency;
- combating obesity - this is facilitated by diet and regular exercise (running, cycling, swimming). For severe angina, morning exercises and walking at least 3 km per day are allowed;
- sex - contrary to all myths, sex with angina is allowed, but with certain nuances. You can find out more about them here.
Smoking, intense exercise (weightlifting, extreme sports), and unauthorized discontinuation of prescribed medications are strictly prohibited. All this can lead to a sharp deterioration in the patient’s condition, increasing the risk of myocardial infarction and death.