Today, atherosclerotic cardiosclerosis is rightfully considered one of the most common diseases developing in people who have reached old age. In addition, the pathology is also one of the most dangerous due to the high probability of various complications that can lead not only to a deterioration in the patient’s quality of life, but also to the risk of death.
As you know, preventing any disease is much easier than treating it, so “you need to know the enemy by sight.” To prevent atherosclerotic cardiosclerosis and be able to recognize the early stages of the pathology, you should know in detail about the mechanism of its occurrence, predisposing factors, clinical manifestations and other aspects of the course of the disease.
general characteristics
Initially, it should be said that atherosclerotic cardiosclerosis is not considered an independent disease, but is a type of IHD (coronary heart disease). Therefore, this diagnosis does not appear in international classifications.
Reference! In ICD 10, types of angina pectoris, myocardial infarction and atherosclerotic cardiosclerosis are classified as coronary artery disease, that is, they are combined into one subgroup and recorded under codes 120-125.
Numerous studies confirm that atherosclerotic sclerosis as a phenomenon is present in people who have crossed the forty-year threshold. The pathological process begins at a young age (20-30 years), and reaches its peak by 50-60 years.
The pathogenesis of the disease is based on the diffuse formation of connective scar tissue in the myocardium (heart muscle), caused by damage to the coronary arteries. Translated from Greek, the term “cardiosclerosis” means “kardia” - “heart” and “sklerosis” - “compaction”. The concept of “atherosclerotic” also consists of two Greek words athero, which means “mush,” and sclerosis.
This indicates that the disease develops due to the accumulation of various metabolic products on the inner surface of the coronary arteries, leading to a narrowing of the lumen. As a result, there is a deterioration in the quality of blood supply to areas of the heart muscle, which can cause serious changes in its functioning and thereby cause life-threatening complications.
Development mechanism
Atherosclerosis develops as a result of disruption of two mechanisms that ensure the functionality of tissue blood supply.
1st mechanism
The first mechanism is a metabolic disorder that directly affects lipid (fat) metabolism. This leads to an increase in the concentration of cholesterol, non-esterified (free) fatty acids and triglycerides. At the same time, the content of phospholipids in the blood decreases, and cholesterol is converted into a finely dispersed state:
- alpha lipoproteins - strong compounds with proteins and triglycerides;
- beta lipoproteins are fragile molecules – prebeta lipoproteins.
Once in the walls of blood vessels, lipoproteins quickly break down, releasing triglycerides and cholesterol, and have an atherogenic effect on the arteries, that is, they damage them. In atherosclerosis, due to a decrease in the level of alpha proteins, the concentration of fragile lipoproteins increases. Depending on the nature and characteristics of lipid metabolism, the predominance of certain groups of lipoproteins, there are 5 types of hyperlipidemia (increased fat content in the blood).
The most pronounced pathogenic effect is observed when hyperlipidemia of types 2 and 3 occurs, which develop due to the predominance of beta and prebeta lipoproteins, respectively. In addition, an important factor is the increase in free fatty acids necessary for the production of triglycerides and cholesterol.
Their effect also helps to reduce the sensitivity of body cells to insulin, which reduces the speed and quality of transformation of glucose into glycogen, leading to hyperglycemia (increased blood sugar) and other local disorders of carbohydrate metabolism. In parallel, pathologies of protein metabolism are also observed, which is due to the direct interaction of proteins and lipids.
Cholesterol plaque in the lumen of the artery
2nd mechanism
The second mechanism, interruptions in which occur during atherosclerosis, is a morphological change in the vascular walls, that is, a violation of their permeability. As a rule, the ability to pass certain substances through the walls of blood vessels increases, which is caused by a decrease in the quality of microcirculation and an increase in the level of acidic mucopolysaccharides.
At the same time, the number of pores increases, resulting in increased permeability of the vascular walls. Often the cause of such disorders is a high level of concentration of local hormones, for example, bradykinin, which, in turn, causes an increased formation of catecholamines.
In the pathogenesis of atherosclerosis, a significant role belongs to the growth of enzyme activity directly in the vascular wall itself, and specifically elastase, which causes changes in the vascular framework. An additional aspect of the development of this pathology can also be an increase in blood pressure (blood pressure), which is a mechanical factor in the appearance of damage.
Alternative medicine
Non-traditional methods of treatment for this pathology can only be auxiliary. Doctors include home recipes in a set of measures aimed at maintaining myocardial function. Any adjustments in treatment should be discussed with your doctor. It is unacceptable to self-prescribe a course of therapy. In myocardial cardiosclerosis, the course of the disease is improved:
- ginger - used as an additive to tea or as a tincture to prevent the formation of blood clots and eliminate atherosclerotic plaques;
- garlic - helps reduce cholesterol concentrations, normalize blood pressure, and is a powerful tool for strengthening vascular walls;
- hawthorn - has a positive effect on blood flow, normalizes cholesterol and blood pressure, restores heart rhythm (tea or alcohol tincture);
- parsley - strengthens the heart muscle, the walls of blood vessels (all components of the plant are used);
- artichoke - consumed in tinctures or in tablet form to strengthen blood vessels and reduce bad cholesterol;
The approach to eliminating the problem and alleviating symptoms should be comprehensive. A competent specialist combines conservative therapy with unconventional methods, recommends the patient to walk more, swim, and dance. It is important to correctly assess your capabilities and not overwork.
Causes
The following factors play an etiological role in the development of atherosclerotic cardiosclerosis. Age. Most cases of the disease occur in people over 50 years of age. As the body ages, the activity of elastase, the production and breakdown of cholesterol, and the concentration of acidic mucopolysaccharides increase.
Gender. In men, atherosclerosis develops more often and at an earlier age. In women, under the influence of sex hormones, beta lipoproteins are formed more slowly, and the concentration of alpha proteins, on the contrary, increases, which is why the risks of atherosclerosis are reduced. Smoking. The effect of nicotine on vascular permeability is extremely negative, since with this type of intoxication the production of adrenaline sharply increases, the synthesis of bradykinin is stimulated, and damage to the walls increases.
Hereditary predisposition. Type 3 lipid metabolism disorders mainly occur in families with coronary artery disease and hypertension. But according to Mendel's laws, only type 2 is inherited. Sedentary lifestyle. It has long been recognized by everyone that movement is one of the components of health. The higher a person’s activity, the better the compensation mechanisms and collaterals (bypass paths of blood flow) in his body.
Tendency to overeat. The calorie content of food consumed should not exceed the body's needs, since abundant nutrition will lead to obesity and all related problems. To avoid the development of diseases, you should not be guided by appetite - you need to eat food based on the calories expended.
Eating fatty and high-calorie foods in large quantities leads to increased cholesterol
In addition to predisposing general factors that can lead to the appearance of atherosclerosis, there are several diseases that also provoke and accelerate the pathological process. This list includes:
- arterial hypertension (all types);
- diabetes;
- obesity;
- hypothyroidism;
- gout.
In this case, it is customary to pay attention to the risk factors present for pathology, which imply various changes in the biochemical and clinical parameters of the body, bad habits and the presence of concomitant diseases. They are divided into:
- the main ones are arterial hypertension, hypercholesterolemia (increased cholesterol in the blood) and nicotine intoxication;
- additional – sedentary lifestyle, diabetes, obesity, gout.
Symptoms
As mentioned above, cardiosclerosis is the growth of connective tissue in the myocardium, which usually occurs after the death of muscle fibers or in parallel with this process. Clinical manifestations of cardiosclerosis directly depend on the type of pathology, of which there are four in medical practice.
Myocardial cardiosclerosis. The formation of a pathological process originates at the site of inflammation that occurs in the myocardium. The cause is proliferative and exudative foci in the stroma of the heart muscle, or destructive changes in myocytes (muscle cells). For this type of cardiosclerosis, the prerequisites are a history of allergic and infectious diseases, and the presence of chronic infectious foci.
Myocardial cardiosclerosis most often tends to develop in younger people. On the electrocardiogram (ECG), this disease manifests itself as diffuse changes in general or with large damage to the right ventricle. At the same time, deterioration of conductivity and rhythm disturbances are observed more often than manifestations of chronic heart failure (CHF).
The increase in heart size occurs evenly or with a bias to the right. Blood pressure is within normal limits, only sometimes a decrease is observed. Symptoms of chronic circulatory failure (CI) usually manifest themselves in the right ventricular type. In most cases, there are no deviations in biochemical blood parameters. Heart sounds are weakened, and a pathological third sound is often heard above the apex of the organ.
Diffuse changes in cardiosclerosis
Atherosclerotic cardiosclerosis. The disease, as a rule, develops quite slowly and is diffuse in nature. Occurs in the absence of focal necrotic changes in the myocardium. The development of pathology is caused by metabolic disorders and hypoxia, as a result of which slowly progressive dystrophy, atrophy and death of individual muscle fibers occur.
With the death of receptor cells, the myocardium loses sensitivity to oxygen, which ultimately leads to ischemic heart disease. However, clinical symptoms may remain mild for a long time. With further formation of connective tissue in the myocardium, the functional requirements for the remaining intact (healthy) myocytes increase accordingly.
Compensatory hypertrophy develops, and then dilatation (increase in chamber volume) of the heart. Basically, there is an enlargement of the left ventricle, and later the symptoms of heart failure (HF) are added - palpitations, shortness of breath, swelling of the legs, dropsy of the cavities and sometimes pulmonary edema.
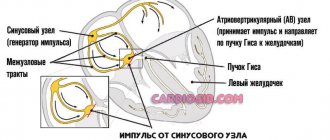
As the disease progresses, dysfunction of the sinus node appears, for example, bradycardia. The formation of scar processes at the base of the valves, in the tendon threads and papillary muscles in a certain number of cases can cause the development of aortic or mitral valve stenosis, or heart failure of varying degrees of severity.
Auscultation reveals a weakening of heart sounds, especially the first at the apex; often a systolic murmur is detected in the aorta, up to an extremely rough sound characteristic of sclerosis (stenosis) of the aortic valve. A systolic murmur may also be heard at the apex, which is the result of relative incompetence of the mitral valve. NK most often develops in such situations according to the left ventricular type.
In atherosclerotic cardiosclerosis, blood pressure is higher than normal, biochemical parameters also undergo changes, expressed in hypercholesterolemia and an increase in beta-liproproteins. This type is very characterized by conduction and rhythm disturbances - often atrial fibrillation (atrial fibrillation), extrasystole, as well as blockades of various parts of the conduction system of varying severity.
Post-infarction cardiosclerosis. The pathology is focal in nature and develops against the background of replacement of a dead portion of the heart muscle with young connective tissue. The clinical picture is similar to the symptoms of atherosclerotic cardiosclerosis. Primary cardiosclerosis. An extremely rare type of disease. This includes cardiosclerosis, which forms with certain types of collagenosis, congenital fibroblastosis, etc.
Reference! The prognosis for cardiosclerosis is based on the extent of damage to the heart muscle, the presence and types of conduction and rhythm disturbances.
Changes in the myocardium in post-infarction cardiosclerosis
Features of the pathology
The growth of connective tissue occurs more intensely during inflammatory processes in the heart muscle - myocarditis. Scars are also formed by inflammation of a rheumatic nature, allergies, and influenza. It should be noted that in some cases the degeneration process is reversible. With the flu, for example, the pathology can result in complete recovery.
Complications
Heart muscle disease has a negative impact on its ability to contract. If you do not pay attention to the pathology and do not provide supportive therapy to the myocardium, the following complications develop: Arrhythmia is the first sign of myocardial cardiosclerosis. Due to the proliferation of connective tissue, the heart cannot fully contract and conduct impulses. At the same time, it is difficult to predict in what rhythm the myocardium will contract—accelerated or slow.
Aneurysm - causes uneven distribution of stress on the heart muscle, which contributes to wear and tear in areas of excessive stress. Subsequently, the wall protrudes and may rupture.
Chronic heart failure is observed during a prolonged course of the disease with large areas affected. Thus, contractile dysfunction of the myocardium occurs.
In order to prevent a severe course of the disease, you should consult a doctor in a timely manner with symptoms, and also undergo a full course of therapy and follow the recommendations of a leading specialist.
Preventive actions
Prevention of myocardial cardiosclerosis consists of taking good care of health, maintaining a healthy lifestyle, and timely treatment of colds of bacterial and infectious etiology. An active lifestyle and a positive mood are the key to health and longevity.
Complications of cardiosclerosis
The process of myocardial sclerosis itself does not cause pain in humans. But this can continue for a certain time, that is, until complications of the disease begin to develop. Cardiosclerosis sooner or later leads to a decrease in the functional capacity of the heart, provoking a worsening of the patient's condition. Even if it is possible to eliminate the causes that caused the pathology, the formation of connective tissue in the myocardium will lead to negative consequences.
The most common complications of cardiosclerosis are:
- chronic fatigue syndrome;
- acquired heart defects;
- cardiac aneurysm;
- thromboembolism;
- arrhythmias;
- CHF.
Most of them are not life-threatening for the patient, but can seriously complicate a person’s existence by limiting his activity. At the same time, such as thromboembolism and aneurysm (if they rupture) pose a threat, since death can occur very quickly, and patients often die before the ambulance arrives.
Power Requirements
If you are diagnosed with myocardial cardiosclerosis, you should reconsider your gastronomic habits. The following are completely excluded from the food basket:
- coffee, caffeinated drinks;
- alcohol containing drinks;
- fast food, street food;
- scrambled eggs;
- rich meat broths;
- sauces, butter.
The diet should mainly consist of vegetables, herbs, fermented milk products, and sea fish. You will have to give up bad habits.
Treatment methods
To select the most appropriate treatment tactics for atherosclerotic cardiosclerosis, the patient is prescribed a full range of diagnostic procedures. These measures are necessary to determine the degree of damage to the myocardium by connective tissue scars, the type of disease, the number of foci and to determine the cause of the pathology. The list of examinations most often includes:
- Dynamic ECG;
- echocardiogram;
- MRI;
- examination of coronary vessels (if coronary artery sclerosis is suspected).
There is no single approach to the treatment of cardiosclerosis. The complex of therapeutic measures being developed is aimed at eliminating the causes of pathology - inflammation of the heart muscle, atherosclerosis in coronary heart disease or the consequences of myocardial infarction. Thus, with the post-myocardial form of cardiosclerosis, the emphasis will be on the treatment of an allergic reaction or infection that led to the onset of the disease.
In case of diffuse atherosclerotic form, it will be necessary to reduce the cholesterol content in the patient’s blood and prescribe treatment aimed at restoring blood flow in the coronary arteries, as well as correcting blood pressure. For this purpose, anticoagulants and vasodilators are used. To reduce the symptoms of heart failure, diuretics, cardiac glycosides, beta blockers, etc. are prescribed.
In case of severe obstruction of the patency of the coronary arteries, in some situations the question of surgical intervention, such as coronary artery bypass grafting or stenting, may arise. During the treatment of cardiosclerosis, the patient’s diet, lifestyle and physical activity must be adjusted. Developing healthy habits and following basic nutritional rules is one of the important aspects of recovery from atherosclerotic cardiosclerosis.
Clinical case
A 49-year-old man came to see me with complaints of weakness, increased fatigue, difficulty breathing, and frequent attacks of dizziness.
Last night I lost consciousness, which was the reason for visiting the doctor. During the interview, it turned out that six months ago, after a cold, the patient developed chest pain, to which the patient did not attach much importance. Auscultation revealed a weak, irregular heartbeat of 42 beats per minute. The ECG revealed complete atrioventricular block, the ventricular contraction rate was 35-47 per minute. Echo-CG showed thickening of the myocardial walls, zones of hypokinesis (reduced contractility) and a small ejection fraction (45%). I suspected postmyocardial cardiosclerosis. At the medical consultation, it was decided to perform an endomyocardial biopsy. The resulting histological specimen revealed myocardial fibrosis and degenerative cell changes.
The final diagnosis was: “Myocarditis, unspecified. Complications: NYHA class II CHF, complete AV block.” The patient was prescribed medications to treat heart failure and had a permanent pacemaker implanted. After the operation, the patient feels satisfactory, dizziness and shortness of breath are no longer bothersome.