Causes of autonomic dystonia syndrome
Autonomic dystonia syndrome is classified as a consequence of various pathologies of the central and peripheral nervous system. VDS is not an independent disease and rarely occurs overnight. The causes of vegetative dystonia syndrome are as follows:
- Problems at home, at school, which lead to systematic constant stress;
- Brain damage due to problems during pregnancy;
- Hormonal changes in adolescence (adolescence);
- Heredity, expressed by poor tolerance to work, high meteotropicity, and so on;
- Diseases of the endocrine system (diabetes mellitus, etc.);
- Bronchial asthma, stomach ulcer, hypertension and other somatic pathologies;
- Passive lifestyle;
- Systematic diseases of the nervous system;
- Carious teeth, sinusitis, otitis media and other permanent foci of infection;
- Mental and physical overload;
- Persistent autoimmune diseases.
Causes and factors contributing to the occurrence of vagotonia in adults
A specific cause causing the state of vagotonia has not been identified. First of all, there are several unfavorable factors that simultaneously affect the body and cause the patient’s painful condition.
In medical practice, the following factors contributing to the development of vagotonia are considered:
- traumatic brain injuries, including concussion;
- intracranial pressure;
- cervical spine injuries;
- prolonged emotional stress conditions;
- impaired functioning of the digestive and respiratory systems;
- presence of chronic diseases;
- diabetes;
- lack of physical activity;
- sudden change in climatic conditions;
- genetic predisposition;
- congenital tendency in case of damage to the nervous system during its prenatal formation;
- the period of menopause in women as a result of hormonal changes.
Such factors do not indicate a 100% probability of vagotonia, but they significantly increase the risk of its development.
What is the manifestation of vegetative dystonia syndrome?
Autonomic dystonia syndrome is divided into three main types:
Vegetative-vascular-trophic syndrome is based on autonomic disorders caused by lesions of mixed nerves, roots and plexuses responsible for supplying impulses to the extremities.
The syndrome of progressive autonomic failure is expressed by peripheral and cerebral disorders in combination with peripheral segmental disorders.
Psychovegetative syndrome is manifested by paroxysmal disorders caused by dysfunction of various brain systems.
Causes of VSD
External factors causing the development of VSD are acute and chronic psycho-emotional stress; iatrogeny; infections (tonsillogenic, carious, bacterial, viral); physical and chemical effects (brain injuries, chronic intoxication, hyperinsolation, vibration, ultra-high frequency currents, ionizing radiation), alcohol abuse; overwork.
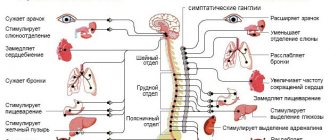
The interaction of internal and external factors leads to disruption at any level of the complex neurohumoral and metabolic regulation of the cardiovascular system, and the leading link in the pathogenesis of VSD is damage to the hypothalamic structures of the brain, which play a coordinating and integral role in the body. Neurologists, neuropathologists and reflexotherapists believe that the leading role in the development of VSD is given to hereditary-constitutional factors, which manifest themselves in the form of functional insufficiency of the regulatory structures of the brain or their excessive reactivity; features of the course of a number of metabolic processes and altered sensitivity of the peripheral receptor apparatus. Dysregulation manifests itself in the form of dysfunction of the sympathoadrenal and cholinergic systems, histamine-serotonin and kallikrein-kinin systems, disorders of water-salt and acid-base states, oxygen supply to physical activity, and decreased oxygen in tissues. All this leads to the activation of tissue hormones (serotonin, histamine, catecholamines) with subsequent metabolic disorders, microcirculation with the development of degenerative processes in the myocardium.
Symptoms of autonomic dystonia syndrome
Symptoms of SVD directly depend on which system or organ is affected. The disease leads to dysfunction of body systems. According to the nature of the course in children, the following deviations are distinguished:
Vagotonia is a disorder of the nervous system, which is manifested by acrocyanosis of the feet and hands. This pathology is manifested by blueness of the extremities. The reason for this is the extremely slow flow of blood to the extremities through small vessels. Other symptoms of SVD include acne, hyperhidrosis, as well as allergies and swelling under the eyes. In the case of a depressive disorder of the nervous system, the skin becomes cold, dry and quite pale, the vascular network becomes unexpressed. In some cases, an eczematous rash and itching may be noticed.
A characteristic disorder is a clear violation of thermoregulation: poor tolerance of frost, wet weather, drafts, as well as constant chills and chilliness.
Children with vegetative dystonia syndrome often complain of poor functioning of the gastrointestinal tract. Nausea, abdominal pain, vomiting, heartburn, diarrhea or, conversely, prolonged constipation, pain behind the sternum, a lump in the throat - a common occurrence with SVD. The cause of these disorders is contraction of the muscles of the esophagus and pharynx. Depending on the age of the child, the most popular symptoms of vegetative dystonia syndrome are: pain in the abdominal area - 6-12 years; periodic vomiting – 3-8 years; diarrhea and constipation – 1-3 years; colic and regurgitation - up to 1 year.
SVD is most clearly represented by dysfunction of the cardiovascular system. This condition is called neurocirculatory dystonia. With this disease, there can be a huge number of cardiac dysfunctions, the most popular of which are associated with conduction and heart rhythm disturbances. Traditionally, cardiac dysfunction includes:
Extrasystole is a contraction of the heart before the set time. Among all arrhythmias, children's extrasystole is a noticeable leader: about 75% of cases are due to this particular disorder. With extrasystole, patients complain of headache, irritability, dizziness, excessive fatigue, and so on. In parallel with this, other diseases and abnormalities arise: high meteotropicity, weather dependence, as well as vestibulopathy. Patients quickly get tired under stress, their performance is at a very low level.
Paroxysmal tachycardia is an extremely sudden symptom. Without adequate reasons, the child’s heart begins to beat much faster. This can last either several hours or a couple of seconds. Most often, children with high initial tone and mild or acute insufficiency of the sympathetic department become victims of paroxysmal tachycardia as a consequence of autonomic dystonia syndrome.
Mitral valve prolapse is often combined with stigmata of dysembryogenesis (minor developmental anomalies). Most often, this indicates some kind of inferiority of vegetative dystonia, as well as connective tissue.
Autonomic dystonia in combination with arterial hypertension is characterized by an increase in blood pressure. This is a fairly popular deviation, which often develops into hypertension of various degrees. The symptoms of this deviation are as follows: memory impairment, cardialgia, irritability, excessive fatigue, dizziness and frequent headaches. As for the headache, it affects the occipito-parietal or occipital zone and has a monotonous pressing character. It appears after waking up or during the day and can intensify after certain loads. Often, another symptom is added to headaches - nausea, but it does not come to vomiting.
Autonomic dystonia, combined with arterial hypertension, manifests itself already at 7-9 years of age. As a rule, it affects pulse pressure, which drops to 30-35 mmHg. Headaches associated with this disease can be easily dulled with a break from study or rest from physical activity, good healthy sleep, and walking in the fresh air.
With this disease, there is a deterioration in the physical development of children. The degree of this lag depends solely on the degree of the disease itself. Most often, children suffering from vegetative dystonia with arterial hypertension have pale skin, red dermographism and a pronounced vascular network.
Types and symptoms of VSD
In most cases, it is quite difficult to identify clearly distinguishable symptoms of vegetative-vascular dystonia. Many signs of this complex of syndromes may be indicators of the presence of diseases that are not directly related to VSD. Only a comparison of all indicators of the autonomic nervous system and/or brain in combination with cardiac or cardiovascular manifestations provides the basis for a definite medical conclusion. Before making a diagnosis of VSD, the doctor must understand the characteristics of the patient’s individual symptoms. Vegetative-vascular dystonia is usually divided into three types (based on blood pressure level):
- the hypertensive type is characterized by increased pressure (periodic surges), symptoms of vegetative-vascular dystonia of the hypertensive form may include increased sweating, anxiety, chills of the extremities, rapid heartbeat and visualized pulsation of large blood vessels (for example, carpal or popliteal);
- the hypotonic type is characterized by a decrease in blood pressure, in this case the symptoms of vegetative-vascular dystonia include shortness of breath, nausea, headache, general weakness, a tendency to faint, coldness of the toes and hands;
- the mixed type is characterized by periodic fluctuations in blood pressure (sometimes also called VSD of the cardiac form), here the symptoms of vegetative-vascular dystonia are usually considered to be general signs of fatigue, a feeling of lack of air, as well as interruptions in the functioning of the heart.
If you find yourself with the signs listed above, first of all, you should reconsider your work and rest schedule. Of course, consulting a doctor is also necessary.
Diagnosis of autonomic dystonia syndrome
In the diagnosis of the disease, an important place is occupied by symptoms, namely their development and course. Against this background, special importance is given to the collection of complaints and anamnesis. Next, the doctor examines the patient, monitors blood pressure, takes pharmacological and physical samples, studies the heart rate, and makes a thorough assessment of vegetative indices. To make a 100% correct diagnosis, additional procedures may be needed, such as cardiointervalography or electrocardiography. After the above studies, Doppler ultrasound of the vessels of the brain, neck and heart is usually performed.
Treatment of autonomic dystonia syndrome
There are several basic principles in the treatment of SVD:
- A complex approach. Doctors combine therapeutic methods of treatment: physiotherapy, drug therapy, herbal medicine, acupuncture, physical therapy, and so on.
- Individual approach. The disease is thoroughly studied, starting with the causes of its occurrence, the degree of development of symptoms and ending with the severity of the disease.
- Timely treatment. Vegetative dystonia syndrome is much easier to cure by consulting a doctor in a timely manner.
- Long-term treatment. It takes a lot of time to treat the consequences of SVD. And we are talking not so much about eliminating the symptoms that have appeared, but about complete recovery.
- Help for the whole family. Psychotherapeutic activities are carried out both with the sick child and with the parents.
In addition to drug methods of treating vegetative dystonia syndrome, non-drug methods are actively used. Medicines are used mainly for long-term VDS or severe disease. At the initial stage of the disease and in mild cases, experts prefer to use non-drug treatment. It should be supplemented by an adjusted lifestyle: sleep - 8-10 hours, daily walks in the fresh air - at least 2 hours a day, a maximum of 1.5 hours should be devoted to television and the computer, and parents should in every possible way protect the child from stress, create a environment around him pleasant microclimate.
It is necessary to strictly adhere to the prescribed diet. It is recommended to eat foods rich in magnesium and sodium salts: vegetables, fruits, legumes, cereals, and so on. In this case, sunflower oil must be replaced with olive oil.
Tea and coffee should be consumed only with milk, kefir and chocolate should be added to the daily diet, and foods with a high liquid content should be consumed as often as possible. The consumption of table salt should be reduced to a minimum in cases with hypertensive syndrome of vegetative dystonia, and beans, cottage cheese, milk, salads, spinach, carrots, and barley porridge should be added to the diet. In the cardiac form of SVD, any food that has a beneficial effect on the properties of the blood is relevant: a moderate amount of spices, vegetable oil, citrus fruits, gray porridge, and so on.
Regardless of the type of disease, honey (for 2-3 months before bedtime), compote of sea buckthorn, cranberries, rowan berries, rose hips, apricots, raisins, dried apricots, lingonberries, various fruit and vegetable juices, infusions and mineral waters are mandatory for consumption. .
Under no circumstances should you be freed from physical activity. Physical education and sports help in the treatment of all forms of SVD, with the exception of diseases that have reached a crisis. In the event of a crisis, it is necessary to engage exclusively in therapeutic exercises. In other cases, running and walking, cycling, skating, swimming, hiking, and skiing help well. A massage of the spine and cervical-collar area (up to 20 sessions) will not be amiss.
The hypotensive form of SVD involves active physical activity and active sports: tennis, shaping, dancing, and so on. In the treatment of cardiac autonomic dystonia syndrome, badminton, swimming and jogging are recommended. The hypertensive type of SVD limits the patient only to swimming, walking and hiking. For any type of disease, it is not recommended to engage in team sports such as basketball, football, handball, volleyball and so on.
Experts agree that physiotherapeutic treatment methods are more than successful. These include treatment with ultrasound, sinusoidal modulated currents, inductometry, electrosleep, electrophoresis of drugs and other methods of similar action. Mixed type vegetative dystonia syndrome is preferably treated with electrophoresis of drugs using one of the methods: either endonasal electrophoresis of a solution of novocaine (2%), or a 1% solution of novocaine in combination with a 0.2% solution of potassium iodide. For sympathicotonia, electrophoresis with a 0.5% solution of aminophylline, magnesium sulfate, papaverine, and bromine is recommended. For vagotonia, the most relevant is electrophoresis with caffeine, mesatone, and calcium. These procedures are carried out every two days for 20-30 days. If necessary, the course of treatment can be repeated after 1-2 months.
Treatment with medications is usually started either in combination with the above methods or after their use has ended. It is preferable to start drug treatment of vegetative dystonia syndrome with common drugs (Zamanikha, bromine, valerian) that have a minimal number of side effects. Drugs and their dosage are prescribed taking into account the individual characteristics of the patient’s body. Age plays a big role in choosing the dosage of medications. Since the duration of treatment for vegetative dystonia syndrome is long-term, drugs are prescribed gradually and often replace each other.
Part of the therapy consists of antipsychotics and tranquilizers that have a sedative effect. The former can significantly reduce the reaction to various external stimuli. Neuroleptics for children are selected from the most “light” ones, which are well tolerated when tranquilizers have shown their ineffectiveness. Sonopax (10-30 mg per day depending on age), frenolone (about 10 mg per day), Terolene (about 10 mg per day) are prescribed. These drugs can be combined.
Tranquilizers help cope with insomnia, fear, panic, and are a good remedy for cardialgia and extrasystole.
For vagotonia, amizil is recommended (about 2 mg per day). Hypersympathicotonic reactivity and sympathicotonia become the reason for the prescription of tazepam (20-30 mg per day), seduxen (about 10 mg per day). These drugs are not recommended for use in children with a tendency to hypotension, as well as in the presence of initial vagotonic tone. For mixed vegetative dystonia syndrome, bellaspon and belloid (1-3 tablets per day), phenibut (0.25-0.5 mg per day), meprobamate (0.3-0.7 mg per day). As a rule, tranquilizers in childhood are prescribed in the lowest possible doses. Over time, the dosage of the drugs is gradually increased. Treatment with small doses of tranquilizers is necessary for at least 2 months, and it is best to take the drugs in the evening or after lunch.
The further course of treatment with medications is prescribed individually and directly depends on the type of dystonia. For arterial hypertensia, sedative herbal preparations are prescribed; antispasmodic medications are used less frequently. ACE inhibitors and calcium antagonists are often prescribed, which are highly effective and have minimal possible side effects. If the effectiveness of these drugs individually is minimal, the doctor may prescribe a combination of drugs.
Rhodiola, eleutherococcus extract, tinctures of aralia, zamanika, ginseng, lemongrass, as well as other herbal psychostimulants are prescribed for arterial hypotension, which is quite severe.
Neurometabolic drugs are most relevant in childhood in the presence of autonomic dystonia syndrome with changes in the functioning of the central nervous system. Pyridoxal phosphate is prescribed for vagotonia; vitamins B4 and E in combination with potassium preparations - for sympathicotonia, and to increase the level of microcirculation - stugeron, cavinton, trental.
Drug treatment of almost all types of SVD also includes the use of herbal dietary supplements with vitamins, microelements and coenzymes.
Consequences and complications
Along with the classic symptoms and diseases accompanying vegetative-vascular dystonia, the patient’s condition can be worsened by frequently occurring (approximately 50%) vegetative crises - sympathoadrenal, vagoinsular and mixed (depending on the predominance of disorders of a particular part of the system).
Sympathoadrenal crisis. The development of a so-called panic attack is associated with a sharp release of adrenaline. The crisis begins with a sudden headache, rapid heartbeat, and paleness/redness of the face. Arterial hypertension, chills, tremors, numbness of the extremities, and anxiety are usually observed. The attack also ends suddenly and is accompanied by asthenia and polyuria (increased urine production).
Vagoinsular crisis. Its symptoms are almost the opposite of sympathetic manifestations. The crisis begins with the release of insulin into the blood and a sharp decrease in glucose levels. The activity of the digestive system increases, intestinal motility increases, and rumbling appears in the stomach. A vagoinsular attack is characterized by a feeling of cardiac arrest, dizziness, arrhythmia, and difficulty breathing. Blood pressure decreases, the pulse becomes rare, sweating, skin flushing, and darkening of the eyes appear. The patient feels weak throughout the body. The attack ends with a state of severe asthenia.
Mixed crises are characterized by activation of both parts of the autonomic nervous system and, consequently, all of the listed complications. As a rule, in the absence of timely treatment of VSD, rather unpleasant consequences arise. This is especially true for childhood, since psychosomatic pathologies often appear during this period of development. These consequences are quite difficult to correct. VSD is not a life-threatening disease, but over time its quality can significantly decrease. If such severe symptoms of vegetative-vascular dystonia persist in adulthood, poor adaptation is observed, and it becomes impossible to fully work and study.
Prevention of autonomic dystonia syndrome
Strengthening health and restorative measures is the most important stage in the prevention of SVD. It is important not only to monitor the child and his lifestyle, but also to maintain a good microclimate in the family (reduce stress, prevent conflicts, and so on). Proper nutrition should be combined with adequate physical activity that is feasible for the child’s body. For preventive purposes, walks in the forest, drinking mineral waters, swimming in the sea, and clean mountain air are useful.