Vascular atherosclerosis is one of the most common diseases in people, especially in old age. This pathology also affects the large vessels of the heart. This is the aorta - it supplies blood and nutrients to all organs of the body.
Therefore, narrowing of the lumen leads to disruption of the functioning of all systems. This, in turn, is fraught with serious complications. Atherosclerosis of the aorta is a chronic disease accompanied by the appearance of cholesterol plaques on the inner wall of the heart muscle vessel.
What it is
Atherosclerosis of the aorta is a chronic disease in which cholesterol plaques form on the wall of this vessel.
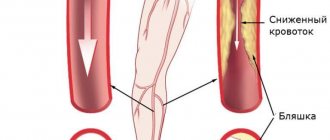
As a result, the lumen of the aorta narrows and blood flow becomes difficult, and this, in turn, leads to an increase in blood pressure and a deterioration in the blood supply to the body. Since the aorta is the largest blood vessel in the human body, pressure surges in such cases can be life-threatening. The walls of the vessel lose their elasticity and degenerative changes begin in them, which often lead to life-threatening conditions, which we will discuss later.
Manifestations
Blockage of a vessel by an atherosclerotic plaque can occur at any segment of the vessel. In this case, the symptoms may differ slightly, but the following symptoms remain common:
- weakness;
- heartache;
- headache;
- increased sweating;
- heart rhythm disturbance;
- increased heart rate;
- loss of consciousness;
- decreased sensitivity of the limbs;
- dizziness.
Depending on the location of the cholesterol plaque, these manifestations may be accompanied by other symptoms. Thus, when it forms in the ascending aorta, the patient may experience attacks of nausea and vomiting, severe pain in the sternum, unstable blood pressure, shortness of breath, which worsens when lying down, impaired swallowing function, and fainting.
Complications of such localization of aortic atherosclerosis are cardiac ischemia, angina pectoris and myocardial infarction. If the fatty deposit is localized in the area of the aortic arch, the patient may notice severe pain in the chest, which intensifies with physical exertion and emotional stress. It is fraught with complications such as cerebral ischemia and ischemic stroke.
If the atherosclerotic process affects the descending aorta, then the patient experiences a feeling of chest compression, increased blood pressure, and rapid pulsation in the right side of the chest. When the abdominal aorta is blocked by an atherosclerotic plaque, the patient encounters such manifestations as:
- pain in the stomach and intestines;
- loss of appetite;
- numbness of the lower extremities;
- swelling of the legs;
- intermittent claudication;
- decreased potency;
- weight loss;
- bloating and flatulence;
- constipation.
Causes
Experts identify several main causes of AA, although their opinions regarding the priority of one or another factor differ. Simply put, doctors have not yet come to a consensus which of the reasons listed below is most important. However, we can say with confidence that the more risk factors are combined in an individual patient’s history, the higher the risk of developing AA.
The main causes of atherosclerosis of the aorta:
- Stress. At first glance, what could be the relationship between nervous tension and cholesterol deposits in blood vessels? Meanwhile, it exists, and it is the most direct one. According to the neuro-metabolic theory of A.L. Myasnikov, nervous stress leads to disruption of the neuroendocrine regulation of protein-lipid metabolism. The result is hypercholesterolemia - increased cholesterol in the blood. It is these excesses that are deposited on the inner walls of blood vessels.
- Arterial hypertension. With a persistent increase in blood pressure, hemodynamics change, as a result of which acidic mucopolysaccharides gradually accumulate in the walls of the aorta.
- Unbalanced diet. Eating fatty foods in large quantities increases cholesterol levels in the blood. In obese people, the risk of aortic atherosclerosis increases many times over.
- Endocrine factor. In diabetes mellitus, lipid metabolism disorders occur, which lead to hypercholesterolemia. In addition, it has been experimentally proven that estrogens reduce blood cholesterol levels. Probably due to the higher levels of these hormones in women, AA occurs at an older age.
Figure 1. Levels of atherosclerosis.
Source: Betty1994 / Depositphotos 5. Genetic predisposition. This issue causes controversy among experts. However, in people whose close relatives suffered from vascular defects, cases of AA are observed more often. Opponents of this theory insist that additional research must be conducted to confirm it and form an evidence base.
6. Blood clotting disorder. Fibrin and fibrinogen are part of cholesterol plaques, which often form in those places where the blood clot is adjacent to the wall of the vessel.
7. Smoking. Doctors agree that smoking increases the risk of AA, but the reasons for this are explained differently. Some experts believe that the prerequisites for AA in smoking patients develop due to disturbances in regional blood flow, others believe that nicotine causes a deterioration in the condition of the vascular wall.
Stages of atherosclerosis of coronary vessels
The stage of the disease is determined by changes in the size, shape, structure of the plaque and the intensity of symptoms:
- Initial (pre-lipid). It is determined only by the results of a biochemical blood test, which shows high levels of total and “bad” cholesterol. Changes in blood vessels are minor.
- Lipoidosis. Cholesterol deposits have not yet formed into pronounced plaques; they look like a soft greasy spot, a few thousandths of a millimeter thick. There are no somatic signs.
- Clinical. A plaque forms, connective tissue fibers join the lipids, and red blood cells accumulate. The vessel narrows. The growth of the growth is accompanied by symptoms of impaired blood supply to the heart.
- Ultimate. Plaques are supplemented with calcium salts, acquire a hard structure, and stenosis progresses. Manifestations of IHD are clearly expressed.
Important! To identify atherosclerosis at an early stage and prevent severe heart pathologies, doctors recommend regular examination of blood vessels, starting from the age of 30.
Risk group
The risk group primarily includes men over 50 years of age who are overweight or obese. This also includes patients:
- with bleeding disorders
- with diseases of the endocrine system;
- with a hereditary predisposition (a history of cases of AA in close relatives);
- with arterial hypertension and other diseases of the cardiovascular system.
A separate group includes people whose work involves nervous tension. If a person tries to deal with stress by smoking or overeating, this significantly increases the risk of developing AA. In other words, the more risk factors identified in an individual patient, the higher the likelihood of cholesterol plaques being deposited on the inner wall of his aorta.
Causes of pathology and risk factors
Atherosclerosis of the aorta does not occur out of nowhere. A number of unfavorable factors affecting the human body lead to its occurrence. Some of them are irreparable, while others can be partially or completely eliminated.
Unavoidable factors include:
- gender (men are more susceptible to atherosclerosis than the fairer sex);
- hereditary predisposition;
- age-related characteristics of the body (most often, severe atherosclerotic damage to the main artery and other parts of the vascular bed occurs in people over 60 years of age).
Risk factors leading to the occurrence of atherosclerosis of the aortic arch and its branches, atherosclerosis of the aortic root, which can be eliminated, include: extra pounds, the presence of addictions, lack of cardio, excessive levels of lipids in the diet, exposure to frequent stress.
Partially removable causes are: impaired carbohydrate metabolism (type 2 diabetes mellitus), hypertension. Timely lifestyle changes have a positive effect on the outcome of the disease!
Symptoms
The most common symptom is aortalgia, which is pain in the aorta. It can be both pressing and burning, but its intensity is always high. Such pain is not always associated with physical activity. It can last from several hours to several days. In rare cases, an atypical pain syndrome is observed, when pain first appears in the back or on the sides of the chest.
Figure 2. Aorta in the heart. Source: Blausen.com staff (2014). "Medical gallery of Blausen Medical 2014". WikiJournal of Medicine 1 (2)
Other symptoms:
- paresthesia (tingling, goosebumps);
- fainting;
- attacks of dizziness;
- xanthoma and xantheplasma - the appearance of yellowish cholesterol plaques on the skin (more often on the skin of the face and eyelids);
- bloating and stool retention;
- blood pressure surges;
- numbness of the limbs;
- weight loss (as a result of digestive disorders);
- difficulty swallowing.
Aortalgia itself should be a reason for an urgent visit to the doctor. If it is combined with any of the symptoms listed above, there is every reason to call an ambulance.
Complications
One of the most common and dangerous complications of AA is the formation of an aortic aneurysm. This is a protrusion in the wall of the vessel, which over time ruptures under the pressure of the blood flow, and as a result of extensive internal hemorrhage, patients in most cases die. The main danger of an aortic aneurysm is its asymptomatic course, which makes diagnosis difficult.
As a result of impaired blood supply to the brain, a stroke (both ischemic and hemorrhagic) can occur, which, in turn, leads to impaired speech function, paresis and paralysis, and death.
Another dangerous complication of AA is thrombosis of the mesenteric arteries, which supply blood to the abdominal organs. Emerging areas of intestinal necrosis due to insufficient blood supply contribute to the rapid development of peritonitis.
With thrombosis of the abdominal aorta in the area of its branching, the blood supply to the lower extremities is disrupted, which can be fraught with the development of gangrene of the legs.
There is also a risk of myocardial infarction, which can occur as a result of embolism (blockage) of the coronary vessels by a detached atheromatous plaque.
Patients with diseases of the cardiovascular system belong to a high-risk group - complications associated with atherosclerosis occur especially often in them.
Diagnostics
Source: US Army photo by Jason W. Edwards / DVIDS
If a person experiences symptoms such as sharp pain in the chest, dizziness, difficulty swallowing and numbness of the limbs, he has every reason to suspect the development of atherosclerosis. When contacting a doctor, you should talk in detail about all manifestations of the disease. Based on the patient’s complaints and data obtained during the examination, the specialist can make a preliminary diagnosis, to confirm which a number of diagnostic studies are prescribed.
The emphasis is on hardware diagnostic methods:
- radiography;
- Ultrasound;
- angiography;
- aortography;
- CT or MRI.
Additionally, a blood test is prescribed to determine the level of total cholesterol, lipoproteins and triglycerides. In combination with medical history data, the research results make it possible to make a final diagnosis and begin therapeutic measures.
Treatment of aortic atherosclerosis
Depending on the severity of AA, treatment can be conservative or surgical. It should also be understood that it is very important to follow a special diet, without which the treatment will not be effective.
Medication
To stop the development of atherosclerosis, several groups of drugs are used:
- Statins (mevastatin, fluvastatin, pravastatin). They inhibit cholesterol synthesis, have an anti-inflammatory effect, and improve the condition of the inner wall of blood vessels.
- Fibrates (fenofibrate, gemfibrozil, bezafibrate). Increase the activity of lipoprotein lipase, an enzyme that breaks down lipoproteins. They also accelerate the metabolism of cholesterol in the liver and have an antithrombotic effect.
- Bile acid sequestrants (colestipol, cholestyramine). They slow down the absorption of bile acids in the intestines, as a result of which the level of lipoproteins and total cholesterol in the blood decreases by 10-20%.
- Antiplatelet agents (ticlopidine and clopidogrel). Reduce the tendency to thrombus formation and reduce blood viscosity. Drugs of this group are used in the treatment of AA to prevent parietal thrombus formation.
Additionally, the doctor may prescribe symptomatic treatment aimed at normalizing blood pressure and liver function. If necessary, the course of treatment can be supplemented with efferent therapy (enterosorption, hemosorption, LDL-immunosorption).
Surgical
In cases where cholesterol plaques grow so large that they damage the inner lining of the aorta and create a noticeable obstacle to normal blood flow, surgical treatment is resorted to. The mechanical obstacle (plaque) is removed along with the affected area of the inner lining of the aorta.
If it is necessary to expand the lumen of the aorta, a stent is installed - an elastic structure made of plastic or inert alloys that follows the shape of the vessel.
Diet
Source: Racool_studio / ru.freepik.com
It is necessary to significantly limit the consumption of foods rich in animal fats. Beef, lamb and pork should be replaced with poultry and sea or freshwater fish. It is also necessary to eat vegetables, herbs and fruits in large quantities - the recommended amount is five pieces a day.
Butter should be replaced with olive oil or any other vegetable oil to taste. It is also necessary to increase the amount of dietary fiber in the diet. For this, flax seeds are suitable (which, among other things, help reduce cholesterol in the blood), as well as granulated food bran, which can be bought in almost any supermarket.
Treatment tactics
Treatment of aortic sclerosis must begin with non-drug remedies, which include a healthy lifestyle, balanced diet and moderate daily physical activity, depending on the age and condition of the patient.
These methods can be attributed to the prevention of vascular atherosclerosis. Lifestyle changes are of great importance for recovery and increase the effectiveness of therapeutic interventions with the use of medications. To reduce the development of a pathological process in the body, folk remedies therapy is widely used.
Forecast
With timely detection of AA, properly selected conservative therapy, as well as adherence to a special diet in combination with lifestyle correction, the prognosis is favorable. In cases where AA is detected at late stages, in which severe complications such as aortic aneurysm or thrombosis of the mesenteric arteries are noted, the prognosis is significantly aggravated.
Prevention involves strict adherence to diet, normalization of body weight and cessation of bad habits (primarily smoking). It is important to avoid a sedentary lifestyle, however, physical activity should also be dosed. To begin with, the patient is recommended to walk for at least 30 minutes a day, then their duration increases as endurance develops. After a few weeks, you can add complexes of therapeutic exercises or swimming in the pool.
It is important to avoid stress and minimize psycho-emotional stress. In addition, it is necessary to carefully monitor the pressure - it should not exceed 130/85 mm Hg. Art.
Folk recipes
Traditional medicine offers recipes that have no absolute contraindications, have a gentle effect on the body and can effectively complement drug therapy.
- Sophora japonica tincture is prepared from a glass of crushed pods and 500 ml of medical alcohol. The medicine is infused in a cold place for 20 days. Drink a tablespoon of tincture three times a day before meals, the treatment course is 3 months.
- Lemon juice, liquid honey and vegetable oil are mixed in equal proportions. Take a dessert spoon of the product in the morning on an empty stomach for three weeks, repeat the treatment if necessary.
- Finely chopped garlic and grated lemon along with zest are mixed in equal quantities. The resulting slurry is poured with half a liter of water and left for 5 days. Take 50 ml in the morning on an empty stomach for a month.
The use of medicines and traditional medicine recipes must be agreed with a doctor and carried out under his watchful supervision.
Atherosclerosis of the aorta can occur without clinical symptoms for a long time and cause the development of severe complications. Preventive measures, annual medical examinations, and treatment of concomitant diseases such as diabetes mellitus, hypertension, and obesity are of great importance for preventing the disease.