Stenting of the carotid arteries is an effective minimally invasive method for preventing ischemic stroke in atherosclerosis and stenosis. If a patient has a narrowing of the carotid sinus of more than 70% in area, then the risk of stroke is about 10% per year. In cases of previous cerebrovascular accidents, the risk of major stroke increases to 50% per year.
Stenting has a number of advantages over carotid endarterectomy, since it does not require surgical access, is performed under local anesthesia and can be used in weakened patients. The main vessels supplying the brain and neck are the two common carotid arteries. They rise up the neck, where each divides into two branches, the external carotid, which supplies blood to the skin and soft tissues of the head, and the internal carotid (ICA), which supplies blood to the brain. Damage to these vessels by atherosclerosis is the cause of most ischemic strokes.
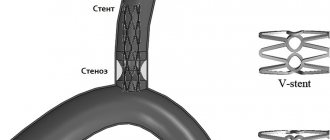
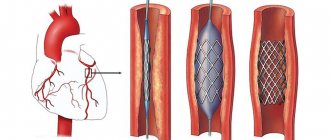
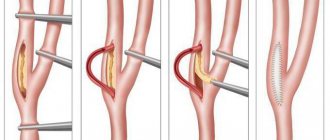
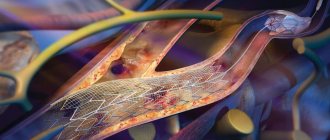
Carotid artery stenting involves an operation to expand the narrowed vessel from the inside with a special balloon and strengthen the wall with a metal mesh (stent). To prevent complications associated with the entry of pieces of plaque into the brain during angioplasty, an intravascular filter is used, located above the site of the atherosclerotic plaque. This operation is performed without incisions, through a puncture in the leg or arm.
Advantages of carotid artery stenting at the Innovative Vascular Center
Our clinic has extensive experience in treating patients with carotid artery pathology. In recent years, stenting has almost replaced open carotid endarterectomy in our practice, as we have become convinced that this method has undeniable advantages and is suitable for most cases.
We perform stenting of the internal carotid artery after assessing the intracerebral vascular bed in order to eliminate the risk of stroke as much as possible. The price for carotid artery stenting in our clinic is affordable, although a disposable instrument is used to perform the operation in our clinic - a recognized world leader in the development of peripheral endovascular products.
During the use of carotid artery stenting in our clinic, we have not noted a single case of serious complications (stroke, bleeding, thrombosis). The clinic’s vascular surgeons have a differentiated approach to the choice of method for restoring arterial patency. We try to perform open endarterectomy in young patients, and ICA stenting in older patients.
Discussion
CEA has proven itself as a method of surgical treatment of ICA stenoses [29, 30]. CAS is an alternative method of correction with equal effectiveness and the absence of complications such as damage to cranial nerves, laryngeal paresis, Horner's syndrome, acute hematomas at the surgical site requiring revision of the paraarterial space, which was also noted in our study [2, 10, 13 , 29, 30].
However, for each of the above methods of correction of the brachiocephalic bed there are specific indications and contraindications, thanks to which CAS, if CEA is not possible, can replace it with less likelihood of dangerous complications [10, 11, 14, 16]. Thus, in our study, clear criteria for choosing CAS were identified in most cases due to the risk of complications associated with a severe comorbid background, which is confirmed in the literature [15, 16, 22, 23, 29, 30].
Perioperative mortality in our study was 2.7% (n=2) compared with 0.7% and 0.6% in the CREST and SAPPHIRE clinical trials, respectively [15–18, 32]. Both cases are associated with a severe comorbid background of patients who had a history of repeated strokes, diabetes mellitus requiring insulin therapy, and post-infarction cardiosclerosis.
Initially, residual symptoms of stroke/TIA occurred in almost half of the patients, which was accompanied by the presence of cysts in the brain. The phenomenon of “luxurious perfusion” after hemodynamic correction aggravates this condition [20, 21, 24, 25, 27]. In addition to the listed reasons, it is necessary to note pronounced atherosclerotic changes in the aorta in the study cohort of patients, which, according to the literature, is a source of atherothrombosis during catheterization of the brachiocephalic arteries during stenting [15–18].
Myocardial infarction, according to foreign authors, is one of the main cardiovascular complications of CAS and CEA in patients with concomitant lesions of the coronary arteries, which is reflected in the presented study [1—10, 15, 17, 24, 32]. This pattern is explained by the presence of multivascular lesions of the coronary bed with high SYNTAX values and occurs due to hemodynamic changes associated with the development of bradycardia during irritation of the carotid glomus and vagus nerve, restoration of normal blood flow after correction of ICA stenosis, as well as artificial hypertension to compensate for cerebral circulation during manipulations with affected carotid artery [1, 5, 10, 29, 30]. Therefore, the cardiac status of each patient must be determined before choosing a carotid revascularization strategy.
Preparing for the intervention
- Before the operation of carotid artery stenting, the patient must undergo a number of mandatory examinations:
- Clinical blood and urine tests
- Biochemical blood test (urea, creatinine, electrolytes)
- X-ray of the lungs
- ECG
- Echocardiography
- Ultrasound of the carotid arteries and transcranial Dopplerography
- Multislice computed tomography of the vessels of the neck and brain
- MRI of the brain
- Consultation with a neurologist
- One day before stenting, all patients receive combination antiplatelet therapy with 300 mg of Plavix. Immediately before the intervention on the vessel, heparin is administered intravenously.
The cause of age-related changes in the vessels of the neck
Throughout life, the human body is affected by many negative factors. The environment, lifestyle, and foods consumed play an important role. With excessive consumption of foods high in cholesterol, atherosclerotic plaques form. As you age, they grow, causing partial blockage of the arteries, a condition called stenosis.
Another reason for age-related changes in the vessels of the neck is a decrease in the synthesis of collagen and elastin by the body. Vascular tissues become less elastic and more susceptible to negative influences.
Pain relief during stenting
The intervention is performed under local anesthesia using light sedatives, since it is necessary to assess the patient’s neurological status during stenting. When the balloon is inflated, the patient may experience a slow heart rate (bradycardia) and a decrease in blood pressure (hypotension), so continuous monitoring of cardiac activity during surgery is necessary.
The patient lies on his back, with his arm abducted, on which a blood pressure cuff is attached. The electrodes of the device for taking a cardiogram are glued to the chest. The surgical field is processed and the patient is covered with a sterile sheet.
Endarterectomy of the carotid arteries
A number of randomized clinical studies of ESA and drug therapy were conducted in parallel with drug therapy itself in patients with symptomatic carotid artery stenosis. More studies - ECST (the European Carotid Surgery Trial), NASCET (the North American Symptomatic Carotid Endarterectomy Trial) and Veterans Administration Cooperative Trial 309 - were the subject of meta-analysis after they concluded the harmonization of the world's stages of stenosis in the carotid arteries. As a result, we managed to accumulate data from 6092 participants and collected 35,000 patients under surveillance in dynamics. Of the 6,092 patients, 601 (10%) were female, over 75 and 1,763 (28%) were female. Carotid endarterectomy increased the risk of ipsilateral ischemic stroke, intraoperative stroke, and operative death in patients with less than 30% stenosis. The procedure is not less costly in patients with stenosis of 30–49%. However, in patients with stenosis of 50–69%, ESA showed a reduction in the 5-point absolute risk of ipsilateral stroke by 4.6% (95% CI, 0.6–8.6%). A more pronounced decrease in the 5-point absolute risk (16%, 95% CI, 11.2–20.8%) was found in patients with stenosis of 70–99%, but not in patients as and Mali Stan, close until occlusion. Patients with a stage close to occlusion did not lose the essential benefits of the ESA, but the number of participants with such a level of stenosis was small, so it is important to change the basic procedure. ESA is small, but there are fewer positive effects in women and less in men.
Asymptomatic stenosis of the carotid artery of moderate to high severity is also a risk factor for ischemic stroke. A cohort study of 1115 patients with asymptomatic carotid artery stenosis found that the risk of stroke increased with the grade of stenosis.
Carotid endarterectomy has proven effective in patients with asymptomatic high-grade carotid artery stenosis. A systematic review of 3 randomized studies involving 5223 patients found that ECA significantly reduced the risk of perioperative stroke and death, as well as subsequent stroke (terminal risk [RR] 0.69). When asymptomatic carotid artery stenosis is detected, ECA has a much greater positive effect in men and young patients.
Complications during stenting
- Transient cerebrovascular accidents
Transient ischemic attacks occur in 0.5% of patients during or immediately after carotid artery stenting. May be associated with tiny pieces of plaque entering the brain as the conductor passes through the narrowed area. These may be transient visual or speech disturbances, weakness in an arm or leg, which disappear within the next 3 hours after the intervention.
- Ischemic stroke
The development of stroke, according to the literature, occurred in 1% of patients after stenting, but in recent years, due to the advent of new technologies for protecting the brain, this complication is much less common.
- Reflex bradycardia and hypotension
These phenomena are associated with the effect of the balloon on the vagus nerve passing next to the carotid artery. They manifest themselves as a decrease in heart rate and a drop in blood pressure. With a timely response from the anesthesiologist, this complication is quickly relieved with medications.
- Bleeding from the puncture site
A rare complication, accompanied by the formation of a tense hematoma in the area of access to the vessel. Sometimes open surgery may be necessary to stop bleeding.
Symptoms of atherosclerosis
The disease may not manifest itself in any way in the early stages. In most patients, the first sign of pathology is a stroke. But atherosclerosis can be recognized by indirect symptoms:
- feeling of weakness, tingling only on one half of the body (right/left);
- inability to control the motor activity of the arm/leg;
- temporary loss of vision in one eye;
- slurred speech.
Symptoms may subside within a few hours, but this is a warning sign. They indicate a high risk of stroke, so you should consult a doctor immediately.
Postoperative period
The patient is discharged on the 2nd day after surgery with a mandatory follow-up ultrasound scan.
After carotid artery stenting, combination antiplatelet therapy with clopidogrel 75 mg/day and aspirin 100 mg/day is prescribed for up to 12 months. Subsequently, aspirin and anti-cholesterol drugs - statins remain.
A control ultrasound scan is performed one month after stenting surgery. The patency of stented segments should be assessed at intervals of 6 months. If signs of restenosis are detected, the patient is prescribed a multislice computed tomography scan with contrast.
Balloon angioplasty
Through a puncture of the peripheral artery, a special guiding catheter is installed at the mouth of the coronary artery. A metal coronary conductor (0.36 mm thick) is passed through it. All stages of its progress are controlled by fluoroscopy. A balloon catheter is brought through a guidewire to the narrowing zone and predilatation of the narrowing is performed (preparing the artery for direct stenting), the diameter and length of the balloon depends on the nature of the vessel lesion. After preliminary balloon angioplasty, a stent is inserted into the artery. It is a balloon catheter with a compressed stent mounted on it. Such a stent is elastic and flexible enough to adapt to the condition of the vessel, and is also compatible with all tissues and organs of the human body. Under X-ray control, the inserted stent is inflated with a pressure of 9-20 atm and is securely implanted into the narrowed area. After this, the balloon is deflated and removed. Control angiography is performed to monitor the positioning of the stent, its full expansion and the absence of residual narrowing. If necessary, repeat angioplasty (inflation) of the stent area is performed using a balloon catheter of greater pressure and size. The stent remains in the lumen of the artery, but cannot move into the artery (since it is implanted with high pressure), and it cannot be removed from the artery. To restore blood flow in the artery, it is periodically necessary to use 2 or more stents (this depends on the extent and severity of the lesion).
Stenting is always preceded by a preparatory period. The patient undergoes a standard examination on an outpatient basis, including gastroscopy (to exclude erosions in the gastrointestinal tract). After the operation, the patient spends 1-2 days in a specialized department. If necessary (for medical reasons), the patient may spend the first day in the intensive care unit. Hospitalization usually takes 1-3 days. After discharge, the patient should be observed by a cardiologist at the clinic or a cardiologist (general practitioner) at his place of residence. When stenting, the patient should receive dual antiplatelet therapy (acetylsalicylic acid drugs + platelet ADP P2Y12 receptor blockers) for 3-6-12 months (depending on the type of stent and the plan of surgical treatment). This is necessary to ensure that blood clots do not form in the installed stents. Within the recommended period of time, the stent cells are completely covered with the body’s own cells, after which the risk of thrombosis is very low.