Thrombosis of the popliteal vein: symptoms
Standard symptoms of popliteal vein thrombosis appear only in half of the cases, so sometimes the disease is difficult to diagnose. The main symptoms of the pathology include acute, prolonged pain in the lower leg area, which can intensify in the evening and at night.
.
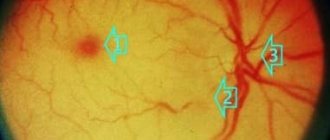
Statistics on the localization of thrombotic lesions
Also, popliteal thrombosis may be accompanied by the following changes:
- when playing sports and physical activity, the leg begins to hurt sharply;
- if you try to bend your foot towards you, you feel pain in your lower leg;
- the limb swells, turns blue, the skin begins to shine;
- there is a feeling of heaviness and distension in the limb.
The person may feel weak and have trouble moving.
Thrombosis of the popliteal vein: causes
The exact cause of blood clots in the vessels has not yet been identified. But several factors are known that provoke thrombosis of the femoral-popliteal segment. These include:
- Age. Most often, the disease affects women after 40 years of age. Older people are more likely to get sick than younger people. After age 50, the risk doubles every ten years.
- Surgical operations. During operations, tissues are injured, blood circulation in them is disrupted, and as a result of anesthesia, blood clotting may increase.
- Limb fractures. The disease manifests itself in more than half of cases after a broken leg. Such injuries disrupt blood flow, and as a result of prolonged immobility of the limbs, the muscles weaken and the blood stagnates in them. As a result, a blood clot appears in the lumen of the vein.
- Phlebeurysm.
- Oncological diseases also often lead to the appearance of blood clots. In many cases, the disease manifests itself in patients who have had tumors surgically removed.
- Sedentary lifestyle, long forced bed rest or sedentary work.
- Thrombosis of the popliteal vein occurs during pregnancy and childbirth due to the high pressure of the uterus with the fetus on the pelvic organs and lower limbs.
- Prolonged static load, injury or compression of a vein, which impairs blood circulation.
- Using hormonal medications (such as birth control) that contain estrogen. Such drugs increase blood clotting, which leads to the formation of blood clots.
- Insufficient fluid intake.
- Heart disease, inflammation, infectious diseases.
- Hypothermia of the limb.
- Long journeys during which a person is forced to sit for a long time.
- Systematic overeating, unhealthy diet and obesity.
- Smoking and alcohol.
Acute deep vein thrombosis of the lower extremities
What is acute deep vein thrombosis of the lower extremities and why is it dangerous? Acute deep vein thrombosis (DVT) of the lower extremities is dangerous due to the risk of pulmonary embolism (PE), which can cause death. DVT occurs as a complication after many diseases, but sometimes it develops in completely healthy people. Postoperative thrombosis is the most common. The incidence of thrombosis in the world is inexorably growing, which is associated with an increase in the number of surgical interventions. Description of the disease
The disease is very common.
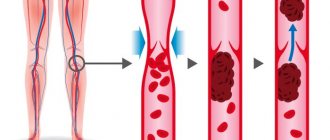
According to various sources, from one to one hundred cases per 1000 people are recorded. The likelihood of thrombosis increases sharply after 40 years. What is acute deep vein thrombosis of the legs and how often does it occur? Blood clots form in the deep veins of the legs or pelvis. They are dense blood clots and often form in areas where blood flows slower: near venous valves, in the sinuses of the gastrocnemius and soleus muscles. Parietal thrombi attach to the vascular wall and leave the lumen of the vein partially free, while clotting thrombi completely block it. Impaired blood flow often causes swelling or pain. The disease sometimes develops rapidly. Since the deep veins of the leg muscles flow into the inferior vena cava, when it breaks off, the blood clot first enters it, and then into the pulmonary circulation. Acute DVT of the lower extremities is the cause of PE in more than 80% of cases. Causes and risk factors Among the causes are primary, associated with hereditary blood clotting disorders, and secondary, arising under the influence of external conditions. Causes and risk factors for the development of deep vein thrombosis For the first time, the process of thrombosis was studied by R. Virchow, who identified several causes of this phenomenon: irritation of the vessel, coagulation disorders and blood flow disorders (Virchow’s triad). The following risk groups for DVT and PE are distinguished: Low risk: patients under 40 years of age and those undergoing minor operations; Moderate risk: 40-60 years, minor or major surgery; High risk: after 40 years, major operations; Very high risk: after 60 years of age, major leg surgeries, hip fractures and other complicated injuries. About ¼ of all cases of the disease occur after fractures of the long tubular bones of the legs, major operations on the joints and peritoneum. Thrombosis threatens a person both in the early and late postoperative periods. Hip and knee surgery increases the risk of DVT to 30-50%, while minor procedures lasting up to 30 minutes have a risk of less than 10%. Main risk factors: Prolonged immobility: condition after a stroke, bed rest, physical inactivity, air travel; Risk factors for which there is a high probability of developing deep vein thrombosis Obesity, accompanied by changes in fibrinolytic activity; General anesthesia with the use of muscle relaxants, when the muscle pump is turned off; Pregnancy and the postpartum period, when changes in hemostasis and compression of blood vessels by the growing fetus occur; Taking certain medications (thalidomide, heparin) and birth control pills with estrogen; Oncological diseases: the combination of a tumor process and DVT is known as Trousseau's syndrome; elderly patients with DVT must be examined for oncological pathology; Hemostasis disorders - thrombophilia; Coronary heart disease along with chronic heart failure; Viral infections; Age-related changes: weakening of blood circulation, weakness of the venous wall, increased blood viscosity; A history of DVT increases the risk of recurrence after injury and surgery. Hemostasis disorders that increase the likelihood of thrombosis are combined under the term thrombophilia. There are congenital genetic defects that determine the tendency to form thrombosis: Leiden mutation, deficiency of antithrombin III, proteins S and C. Thrombophilia can be suspected if thrombosis occurs at a young age. Forms and types
of Thrombosis are distinguished by etiology, location of formation and types of blood clots: Proximal thrombosis is localized in the popliteal or femoral vein and causes pain in the leg, swelling and tenderness when palpated over the affected veins.
But sometimes its first manifestation is pulmonary embolism. Distal thrombosis affects the calf veins. There is moderate pain and tenderness in the lower leg, but sometimes there are no symptoms. There is usually no swelling. Ileofemoral thrombosis occurs in the iliac and femoral vessels. Pain is felt along the inner thigh, calves, and groin. The leg swells noticeably from the foot to the groin. Palpation in the projection of the main veins of the thigh and groin is painful. Thrombi often form in the femoral vein, somewhat less frequently in the popliteal and gastrocnemius, and in the inferior vena cava - relatively rarely. By origin, thrombosis can be stagnant (with varicose veins, external compression of blood vessels, internal obstructions to blood flow), inflammatory and associated with thrombophilia. There are also occlusive, parietal and floating thrombosis. A floating thrombus is diagnosed in approximately 10% of cases. It is attached to the venous wall at only one end and seems to dangle in its lumen, so the likelihood of tearing off is very high. Danger and complications
A complication of deep vein thrombosis can be pulmonary embolism.
The main danger is pulmonary embolism. Complete blockage causes instant death, partial blockage causes heart failure. As a cause of sudden death, pulmonary embolism ranks third after coronary artery disease and stroke. After thrombosis of the proximal veins, chronic venous insufficiency often develops. Venous pressure increases when moving, valves do not work well. Venous stagnation is manifested by trophic disorders: hyperpigmentation, dermatitis, induration, and in severe cases, trophic ulcers. Venous insufficiency can be suspected by swelling of the legs, depending on the position of the body. More than half of patients develop postthrombotic disease. Almost a third of such patients become disabled. Symptoms
Sudden pain in the leg, worsening when standing or walking, is the most characteristic symptom.
Soon soft tissue swelling, heaviness and distension develop, and the temperature may rise. The skin in the area of edema is bluish and shiny. After a few days, a network of superficial veins appears. Blood clots in the calf and deep main veins sometimes do not manifest themselves. Disturbances in blood flow are partially compensated by other veins. You should pay attention to slight swelling of the ankle and pain in the calf muscle. Diagnosis
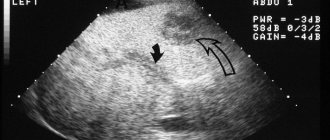
The main diagnostic method is ultrasound duplex scanning, which determines how narrowed the lumen of the vein is, the size and mobility of the blood clot.
X-ray contrast venography is performed to clarify the diagnosis, as well as for blood clots above the inguinal fold. In difficult cases, magnetic resonance venography is performed. Treatment Treatment
methods for deep vein thrombosis of the lower extremities.
Patients are treated inpatiently. Bed rest with the affected leg elevated and anticoagulants are prescribed. Thrombolytic therapy is indicated at the very beginning. Drugs for dissolving blood clots have serious side effects (bleeding) and are prescribed according to strict indications. When diagnosing a floating thrombus, a vena cava filter is placed in the vein to prevent it from moving upward. In severe cases with a risk of gangrene, a thrombectomy is performed - mechanical removal of a blood clot. Compression hosiery is used to reduce the likelihood of complications. After discharge, patients are recommended to undergo lifelong therapy. Prognosis
Depends on the type and position of the blood clot.
Occlusive thrombosis is not dangerous, since the thrombus is tightly attached and completely blocks the blood flow. A parietal thrombus is also not dangerous, but it can continue to grow and become floating. The probability of a floating thrombus breaking off is very high. Proximal vein thrombosis in approximately half of cases is accompanied by pulmonary embolism, often asymptomatic. After a few months, in most patients, venous blood flow is restored, but weakness of the valve apparatus develops. In distal veins, thrombi often resolve on their own, but thrombosis can spread to the proximal veins. Within several years after the disease, more than half of patients develop postthrombotic syndrome, and in the absence or ineffectiveness of treatment, asymptomatic pulmonary embolism. Chronic venous insufficiency worsens the quality of life and leads to disability. Prevention
The following preventive measures are used: Early start of activity in the postoperative period, gymnastics, exercise therapy; Compression stockings or elastic bandaging; Anticoagulants; Avoidance of risk factors. After discovering the risk of thrombosis during long air travel, many airlines began informing passengers about preventive measures. It is advised to wear loose clothing, drink plenty of fluids, do exercises to combat blood stagnation in the legs, and massage your calves. When sitting for a long time, you should use footrests to avoid squeezing the veins. Acute DVT of the lower extremities poses a serious threat to life. If symptoms of the disease appear (sharp, sudden pain in the leg, swelling, bluish skin color), it is important to start treatment as soon as possible. Timely treatment in a hospital prevents the development of pulmonary embolism. Along with medications, an effective way to prevent the disease is an active lifestyle and exercise.
Popliteal vein thrombosis: diagnosis
To determine the exact signs of thrombosis, duplex ultrasound scanning (USDS) is used. The method helps to find a blood clot, measure it, determine its exact location, and recognize whether it is floating in the vessel. The method also helps to examine the condition of the veins. In addition, during the examination, doctors receive information at what speed the blood moves.
Diagnosis of popliteal vein thrombosis
Doppler ultrasound is also used in diagnosis. This method is used to determine the patency of the veins and find the place where the thrombus is located.
Treatment of thrombosis
The objectives or goals of the treatment are very specifically formulated today:
1. Stop the spread of thrombosis.
2. Prevent pulmonary embolism.
3. Prevent the progression of edema and prevent venous gangrene.
4. Restore the patency of the veins and the function of the valve apparatus in order to further avoid the development of post-thrombophlebitic disease.
5. Prevent recurrence of thrombosis.
Conventionally, modern approaches to the treatment of patients with acute phlebothrombosis in the inferior vena cava can be divided into three main ones:
1. Conservative.
2. Minimally invasive.
3. Surgical aggression.
Conservative therapy
The set of measures of this approach includes:
- early activation using elastic compression,
- anticoagulant,
- nonspecific anti-inflammatory therapy,
- hemorheological therapy,
- intermittent pneumocompression.
With the timely use of the above methods, it is possible to restore the patency of the veins and minimize the manifestations of post-thrombotic disease.
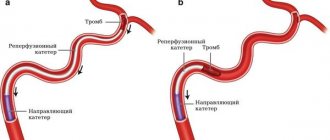
Minimally invasive methods
Today, this is the most common group of methods in clinical use, designed to solve all of the above problems or goals of treating patients with deep phlebothrombosis.
Here it is necessary to distinguish three subgroups of methods:
1. Installation of vena cava filters and partial cavaplication.
2. Regional and systemic thrombolysis.
3. Catheter thrombus extraction and pharmacomechanical thrombectomy.
Installation of vena cava filters and partial cavaplication
At the beginning of the formation of phlebology as a separate scientific specialty, one of the main issues requiring immediate resolution was the issue of preventing pulmonary embolism in phlebothrombosis. After the development in 1959 of the method of external plication of the vena cava with mattress sutures and external plication with clamps, it was possible to determine the further direction of solving the problem of acute deep phlebothrombosis and its complication - pulmonary embolism. Until 1967, the method in combination with conservative therapy remained the only clinical approach to this problem. Despite the fact that the technology of external partial clipping with clamps is associated with the need for traumatic surgical access and is practically impossible in seriously ill patients, this approach has been used and improved in limited situations to this day (for example, using endovideoscopic techniques, plication from a mini-approach).
The Mobin-Addin intraluminal vena cava filter, created and applied clinically, which required studying methods for delivering the device to the object, was the first experience of intraluminal catheter intervention and, in fact, served as the beginning of the development of a new branch of angiology - interventional radiology. Further development of this direction was carried out mainly along the path of improving the design of vena cava filters and studying their effect on hemodynamics and the clinical course of the main process.
Currently, temporary vena cava filters are preferred. The temporary vena cava filter is removed no later than the third week.
In the vast majority of cases, installation of a vena cava filter is not required at all.
Why is it not advisable to install a permanent vena cava filter?
You should always remember that a permanent vena cava filter means a lifelong use of anticoagulant drugs and a lifelong risk of filter thrombosis (a foreign body in the lumen of the vein is often complicated by thrombosis).
It has been repeatedly noted that as a result of the installation of vena cava filters, pulmonary embolism may occur in the immediate period with a frequency of 1.5-8%, and in a period of up to 3 years, thrombosis of the inferior vena cava occurs with a frequency of 12-25%.
For thrombosis below the inguinal ligament, installation of a vena cava filter is not advisable, since there are other methods for preventing pulmonary embolism.
Regional and systemic thrombolysis, catheter thrombus extraction, rheolytic thrombectomy
Thrombolytic therapy. The method is based on the administration of drugs that activate endogenous fibrinolysis (streptokinase, urokinase, tPA, etc.).
Apparently because the means of influencing the blood clot used in this method can only be effective in relatively fresh areas of the blood clot (up to 3-5 days), so its effectiveness is low. Meanwhile, the use of regional catheter thrombolysis in 44% of cases allowed some authors to preserve valve function and thereby prevent the development of postthrombotic disease.
Catheter thrombus extraction . It should be immediately clarified that this method is applied only to high segments of the inferior vena cava basin, since the technology itself does not allow its application in the infrainguinal position due to the obstacles formed by the valve apparatus of the veins at this and lower lying levels. The method is based on capturing thrombomass from accessible segments of the inferior vena cava and iliac veins into a special container bag and removing them by removing them through a phlebotomy opening.
Pharmaco-mechanical thrombectomy . The newest of all interventional and surgical technologies. So far, there are descriptions of individual cases in the literature. The method is based on the Bernoulli effect, where the speed of a hydrodynamic jet creates areas of negative pressure in the surrounding media. The method has the same scope as catheter thrombectomy.
Surgical interventions for femoropopliteal phlebothrombosis
It is known that the most effective thrombectomy is possible only for blood clots no more than 3-7 days old.
Currently, most authors still adhere to cautious tactics when surgically removing thrombus masses from the femoropopliteal segment, completing the operation by ligation or resection of the ostial segment of the proper femoral vein, assessing the immediate results as good due to the lack of severity of symptoms of chronic venous insufficiency. The calculation with this approach is to switch the main venous flow to the deep vein of the thigh, which should provide a stable main outflow. In some cases, arteriovenous fistulas are used to prevent rethrombosis.
A number of researchers use the tactic of surgical antegrade thrombectomy without subsequent ligation or ligation of the femoral vein itself, in some cases supplemented by plication of the femoral vein itself or without it.
Popliteal vein thrombosis: treatment
If we talk about the dangers of popliteal vein thrombosis, then first of all it is worth mentioning its complications. More than 10% of patients die from them. If the disease is not treated, blood clots can break off and travel through the vessels. When they enter the lungs, they completely block the lumen of the pulmonary artery. This leads to death in most cases.
It is the danger of complications that is taken into account when choosing a treatment method. Most patients are recommended to be treated in a hospital. If their risk of thromboembolism is high, treatment will take longer. In the first days of treatment (from 3 to 10 days), the patient must remain in bed. In this case, the affected limb should be elevated at all times. This is especially important if doctors are unable to conduct a complete examination.
The ratio of venous and arterial thrombosis
If conservative treatment of thrombosis does not have an effect, doctors recommend that the patient undergo surgery.
Many patients are given medication to treat thrombosis in combination with the use of elastic compression bandages, which help protect the valves and increase blood flow. To increase the effectiveness of treatment, local topical preparations are used. Such products (creams, ointments, venotonic tonics) are recommended to be used regularly after exacerbations, as a preventive measure.
Treatment is also accompanied by internal medication. The patient is prescribed anticoagulants to slow blood clotting and protect against blood clots. For severe pain, analgesics are also prescribed. To increase blood flow from the legs, phlebotonics are used.
Expert opinion
Angioprotectors are widely used in the treatment of this disease. These are special preparations with complex action. They suppress the inflammatory process, restore vascular walls, improve blood composition and accelerate microcirculation. Also, such products help fight swelling. .
Vascular surgeon, phlebologist
Osipova Ekaterina Yakovlevna
In some cases, antibiotics are also used in treatment. The doctor develops suitable therapy in each case individually.
To reduce the manifestations of popliteal vein thrombosis, the use of Normaven® products is recommended as an additional measure. Testing of the Foot Cream proves that its use for 3 months can reduce the feeling of heaviness and fatigue in the lower extremities, minimize cramps and swelling, and also reduce the severity of the vascular pattern. The product was developed by specialists from the pharmaceutical company VERTEX and has the necessary documents and certificates.
Treatment of thrombosis with folk remedies
Symptoms of thrombosis
Symptoms of acute deep vein phlebothrombosis include:
- edema,
- bursting pains,
- cyanosis of the limbs,
- expansion of saphenous veins,
- local increase in skin temperature,
- pain along the vascular bundle.
However, local hyperthermia and pain are more typical for superficial thrombophlebitis. The latter should be considered more likely to be risk factors for the development of deep vein thrombosis.
Classic symptoms of DVT:
- pain,
- soreness,
- swelling,
- hyperemia,
- Homan's sign.
The overall sensitivity/specificity of these symptoms ranges from 3 to 91%. The presence of symptoms does not confirm DVT. The absence of symptoms does not exclude DVT (up to 50% of patients do not have any clinical symptoms).
Calculation of the probability of thrombosis
In 1997, Wells et al developed and tested a clinical model of the likelihood of DVT
The presence of each feature is scored 1 point:
The primary development of thrombosis in the deep veins of the leg is most common. This is facilitated by conditions under which such an important hemodynamic factor as contraction of the lower leg muscles is turned off. Such localization occurs in more than half of the observations.
Physical examination reveals positive symptoms:
- Moses - pain when squeezing the lower leg in the anteroposterior direction,
- Homans - pain in the calf muscles with dorsiflexion of the foot,
- Lowenberg - pain in the calf muscles at a pressure of up to 150 mm Hg. Art., created by the sphygmomanometer cuff.
However, the same symptoms will be positive with any other inflammatory process in the limb being examined.
When the femoral vein is involved in the process, patients note aching pain along the medial surface of the limb according to the projection of the Gunter canal.
Thrombosis of the common femoral vein is manifested by a more pronounced increase in the volume of the leg and even the thigh, cyanosis of the skin, the intensity of which increases towards the periphery. There is an expansion of the saphenous veins in the distal part of the thigh and lower leg. If thrombosis spreads to the mouth of the great saphenous vein of the thigh, then hypertension developing in the superficial venous system leads to the shutdown of the anastomoses crossing with the contralateral limb. In this case, there is an increase in the pattern of the saphenous veins in the pubic and groin areas. On palpation, the vascular bundle is painful throughout the entire thigh. The period of pronounced venous stasis lasts 3-4 days, after which a slow decrease in edema occurs. This phenomenon is due to the inclusion of collateral systems in the blood circulation. Thus, a decrease in pain and less pronounced swelling can create imaginary well-being and often lead to a later visit to a specialist. In addition, phlebothrombosis can occur without any complaints from the patient (asymptomatic), especially in postoperative patients.
More or less characteristic symptoms:
- bursting pains,
- swelling (increase in calf circumference),
- skin cyanosis.
Edema is of greatest importance in terms of making a preliminary diagnosis. However, none of the listed clinical symptoms can be considered absolutely reliable in the diagnosis of this nosology. Any, even the most minimal patient complaints (for example: simple discomfort in the distal segments of the lower limb), especially in combination with the presence of risk factors, require additional examination of the patient for the presence of phlebothrombosis.
Thus, we can conclude that the presence of phlebothrombosis based on the history, patient complaints and clinical symptoms can only be suspected in order to confirm or exclude its existence during further examination, determine the localization and embologenic danger. The absence of pathognomonic symptoms and the presence of a period of imaginary improvement are the reason for late hospitalization of patients, which in many cases limits the possibility of effective surgical treatment.
Diagnostic tests in patients with suspected DVT
- Assessing the clinical likelihood of having DVT,
- D-Dimer,
- Ultrasound examination of veins,
- MRI venography,
- MSCT.
Thrombosis of the popliteal vein: treatment with folk remedies
At the first pain and symptoms of thrombosis, immediately consult a doctor. It is important to remember that untimely treatment or its absence leads to the fact that normal blood circulation in this area can be lost irretrievably, without restoration.
Some people choose traditional medicine to combat blood clots. Indeed, selected recipes passed down from generation to generation gave in some cases positive results. It is not recommended to experience the power of ancestral knowledge without consulting a doctor. Traditional recipes can act as a counterweight to traditional medicine and interfere with the main treatment. We talk about the methods that are considered the most popular among the people.
You can try verbena infusion. Brew a spoonful of verbena in a glass of boiling water, then strain and drink in small sips all day long.
Baths with marsh dried dried herbs can relieve pain. To do this, pour 200 g of the plant into a bucket of boiling water and infuse. Take a warm bath for sore feet for 30 minutes. Regular procedures are distracting.
!
Combine such procedures with the main treatment, after consulting with your doctor.
Instead of swampy cucumber, you can use regular cucumber. Preparation for the procedure is the same, only you need to keep your feet in the infusion for no more than 20 minutes.
A popular traditional medicine in the treatment of popliteal vein thrombi are compresses based on a decoction of thistle. They relieve pain and have a healing effect.