Postthrombotic disease (or PTFS - postthrombophlebitic syndrome) is a pathological condition that develops after thrombosis in the deep veins. This disease is manifested by swelling and trophic ulcers of the lower leg. The first year after thrombosis determines the further state of the venous system of the affected lower limb. This year it is necessary to strictly adhere to the recommendations of the phlebologist. The maximum restoration of venous patency achieved with the help of treatment significantly improves the condition of venous outflow. If targeted treatment is not carried out, severe post-thrombotic disease develops in the next 2-3 years. Implantation of a non-removable vena cava filter for venous thrombosis prevents dangerous complications, but very often leads to the development of post-thrombotic disease of both legs.
The Innovative Vascular Center successfully treats post-thrombotic disease using endovascular and reconstructive valve surgeries.
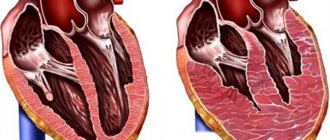
Postthrombotic disease (or postthrombotic syndrome) develops 3-5 years after thrombosis of the main deep veins of the limb. Over time, the clot becomes fixed in the vein, begins to gradually decrease, and holes appear in it through which blood begins to flow. However, the thin structures that facilitate blood flow - the venous valves at the location of the blood clot - become scarred and no longer create an obstacle to the reverse flow of blood. Due to valvular insufficiency, blood through the deep veins begins to move up and down, thus creating conditions for venous stagnation, especially in the lowest parts - in the foot and lower leg.
Risk factors
- The patient suffered deep vein thrombosis 2-5 years ago, which was confirmed by ultrasound examination of the venous vessels.
- If the patient has had a vena cava filter installed.
- There was an injury to the lower leg (large bruise, fracture of the bones of the lower leg, femur, ankle) and after the injury there was significant swelling for a long time.
- Difficult pregnancy with complications and prolonged subsequent swelling of one or both legs.
- Long-term post-mortem treatment associated with severe surgery, trauma, coma.
- Congenital tendency to thrombosis (thrombophilia)
Perverted venous blood flow through the deep and superficial veins causes changes in blood circulation at the microscopic level. As a result, skin nutritional disorders occur, manifested first by brown coloration and hardening of the skin, and then by a trophic ulcer. At the same time, the outflow of lymph is disrupted, which in the long term can lead to elephantiasis. Venous congestion can be associated with reflux (backflow of blood) when the venous valves are damaged, with difficulty in venous outflow due to blockage of the veins or their narrowing. Treatment methods are aimed at correcting these disorders.
Complications of varicose veins
What is postthrombotic (thrombophlebitic) disease or syndrome? What leads to the development of PTF? How to treat postthrombotic (thrombophlebitic) disease? What treatments are there for this disease? Is it possible to completely cure PTF? What is the prognosis for a patient with PTF? Which doctor treats PTF?
What is postthrombotic (thrombophlebitic) disease or syndrome?
Postthrombophlebitic (post-thrombotic) disease or syndrome is a common complication after deep vein thrombosis. The problem is that the main body of blood flows through the deep veins of the legs to the body, which comes to the legs through the arteries. Normally, blood flow through deep veins relative to superficial veins is approximately 5:1. Thrombosis (that is, complete blockage) of part of the deep system leads to redistribution of blood flow along the bypass lines of the deep femoral vein. However, the superficial veins are usually not able to fully cope with the increased blood flow. This leads to acute venous insufficiency, which is manifested by swelling of the leg below the level of thrombosis, bluish color of the skin, and bursting pain in the leg. The pain subsides a little after sleep, in a horizontal position, but returns again. If the thrombosis does not recanalize (resolve) for a long time, a restructuring of the venous and lymphatic systems occurs, swelling persists, and the increased volume of the leg remains for a long time (or forever). Unfavorable changes in the microcirculation system and chronic edema lead to disruption of skin trophism and decreased function of the muscles of the limb. All these changes represent postthrombotic syndrome.
Deep vein thrombosis leads to the development of PVT
The clinical picture of postthrombotic syndrome or disease (PTSD) is characterized by swelling and changes in the skin, as well as dilation of superficial veins and varicose veins. Skin changes may include darkening or hyperpigmentation and venous eczema. In some cases, fibrosis of subcutaneous adipose tissue and skin develops. This condition, known as lipodermatosclerosis, impairs the perfusion (nourishment and circulation) of the skin and puts patients at increased risk of venous ulcers. Venous ulcer is one of the most serious complications of postthrombophlebitis disease. In addition to skin problems, patients may experience symptoms such as heaviness, pain, itching, cramps and paresthesia. These symptoms are worse when standing or walking and improve with rest or elevating your legs. Swelling of the limb due to blockage of blood outflow can be quite significant, leading to asymmetry of the limbs, causing cosmetic discomfort for the patient and problems with the selection of clothes and shoes.
Photo of a patient with PTF. Pronounced asymmetry of the legs due to swelling.
Some patients experience severe pain with exertion, known as venous claudication. This is the result of restriction of venous outflow, which is most often located in the iliofemoral segment of the deep veins.
Important: post-thrombotic disease seriously impairs the quality of life. The quality of life of patients with PTF is also affected by age, obesity, and the presence of chronic diseases.
Appearance of a patient with PTF 2 years after popliteal vein thrombosis.
Postthrombotic syndrome is a chronic condition that is diagnosed based on clinical assessment. Although not all symptoms and signs are permanent after a diagnosis of PTF, the diagnosis is considered chronic.
Postthrombotic syndrome is a fairly common condition, occurring in 20%-50% of patients who have suffered thrombosis of the deep venous system. The multiplicity of diagnostic rating scales may be a likely reason for the lack of precision in estimating prevalence and incidence. There are at least six scales that are used to assess the severity of PVT - Villalta, Brandjes and Ginsberg, as well as scoring scales that were designed to assess the severity of chronic venous insufficiency: VCSS, CEAP and Widmer score. None of the so-called “PTFB-specific” scores have been officially validated. Note that the incidence of PVT appears to have remained unchanged in recent years, despite many improvements in the treatment of acute deep vein thrombosis, including state-of-the-art anticoagulation therapy, early mobilization, and adequate (if necessary) compression therapy.
At the International Society on Thrombosis and Haemostasis (ISTH) subcommittee meeting in 2008, consensus was reached to diagnose PVT with a Villalta score of ≥5, 6 months after deep vein thrombosis (Kahn SR, Partsch H, Vedantham S , Prandoni P, Kearon C; Subcommittee on Control of Anticoagulation of the Scientific and Standardization Committee of the International Society on Thrombosis and Haemostasis. Definition of post-thrombotic syndrome of the leg for use in clinical investigations: a recommendation for standardization. J Thromb Haemost 2009;7:879–83.)
The Villalta scale has many advantages because it has good scoring properties and is easy to use. The Villalta score, in combination with the quality of life questionnaire specific to venous diseases, allows for the standardization of subjective criteria and has even been proposed as the “gold” standard for diagnosing PVT. However, this scale also has a number of limitations: venous claudication is not included in the scoring system, and venous ulcers are not graded according to severity.
Postthrombotic syndrome is a chronic disease and, therefore, a diagnosis based on examination alone may not be ideal. Villalta scores tend to be unstable. This may lead to overestimation of the diagnosis, especially in patients with mild PTF. With minor or irreversible skin changes, the final assessment becomes more dependent on complaints. Thus, making a diagnosis based on one examination alone may result in a less accurate assessment than making a diagnosis based on repeated observations.
With a diagnosis based on only one grading scale, patients will be diagnosed with PTF more frequently, with the majority of these patients being classified as having a mild course. For cases of moderate to severe PTF, it does not matter what Villalta score definition results in, as the symptoms and signs observed are likely to be irreversible.
There are still no predictive models to identify patients at low or high risk of developing PTF. The fact that patients at risk cannot be identified early makes it difficult to provide timely and adequate therapy.
One model for predicting the development of PTF was proposed by Amin et al in 2021. It involves a two-stage assessment. At the first stage, the diagnosis of PTF is made based on the score on the 2008 ISTH consensus scale. The basic model (first step) is based on the assessment of examination results and complaints in the acute phase of thrombosis. Predictors in the base model were: age, BMI, gender, episode of deep vein thrombosis or iliofemoral thrombosis, deep vein thrombosis due to varicothrombophlebitis, and smoking. The second model (second step) in assessing PTF is performed in the subacute phase 6 months after the onset of deep vein thrombosis and contains one additional variable: residual thrombosis. The rationale for developing the secondary model was that for some, treatments are quite effective in the acute and subacute phase and can be discontinued in selected patients at low risk of developing PTF after 6 months of thrombosis. However, at present, the effectiveness of using the scale in predicting PTF has not yet been assessed.
Treatment of postthrombophlebitic disease
Until now, the basis of treatment and prevention of PTF is compression therapy. To date, there are eight studies evaluating the effect of medical compression stockings for the prevention of PVT, starting in the acute or subacute phase after deep vein thrombosis. In three studies, a good preventive effect of compression was obtained, in two others there was no effect. Other studies have assessed decreased duration of compression or delayed initiation of compression therapy, and another has examined the comparative effectiveness of different types of compression stockings. Several meta-analyses on this topic have been published in recent years. Recently, a contemporary meta-analysis (with subsequent updates) was conducted focusing on the results of compression initiated in the acute and subacute phase. This assessed the effect of wearing compression stockings for 1 year versus 2 years (elastic compression stockings) for the prevention of post-thrombotic syndrome (OCTAVIA study). This is a randomized controlled trial which found that after initial treatment, continued wearing of an elastic compression stocking for 1 year in patients without PTFE was significantly better than discontinuation of treatment, with an NNT score of 14. Although at this stage the overall conclusion is that that the quality of the evidence is not very high, but the overall direction of effect is toward a beneficial effect of compression, as well as surgical treatment of thrombosis for the prevention of PTF (RR 0.62, 95% CI 0.38-1.01; P = .05)
Leg banding for PTF
A good study on the role of diosmin in the form of a micronized purified flavonoid fraction (Detralex 1000) was carried out by K.V. Lobastov. and co-authors in 2021 (Lobastov, K., Schastlivtsev, I., & Barinov, V. (2018). Use of Micronized Purified Flavonoid Fraction Together with Rivaroxaban Improves Clinical and Ultrasound Outcomes in Femoropliteal Venous Thrombosis: Results of a Pilot Clinical Trial Advances in Therapy. doi:10.1007/s12325-018-0849-z). The study found that the incidence of PVT after deep vein thrombosis was lower when using a combination of an anticoagulant with MOFF compared with the anticoagulant alone group. In addition, when using MOFF, the rate of thrombus recanalization increased.
Thus, to prevent the development of PTF after acute deep vein thrombosis, wearing compression stockings, taking anticoagulants (but not aspirin!!), as well as micronized flavonoid fraction (MOFF, Detralex 1000) can reduce the likelihood of developing postthrombophlebitic disease.
Compression stockings for the treatment of post-thrombotic disease (syndrome)
How does postthrombotic disease develop?
The disease develops some time after thrombosis of the main deep veins of the limb. The thrombus is first fixed to the venous wall, begins to gradually decrease, and holes appear in it through which blood begins to flow. However, the delicate structures that allow blood to flow, the venous valves, become scarred and stop functioning normally. Due to valvular insufficiency, blood through the deep veins begins to move up and down, and leads to venous stagnation, especially in the lowest parts - in the foot and lower leg. Clinical signs of chronic venous insufficiency develop with the formation of a “venous swamp” and edema in the lower parts of the leg. Under these conditions, any scratch, scratching, or insect bite leads to the formation of a long-term, non-healing trophic ulcer. This is the most severe manifestation of postthrombophlebitic disease.
Methods for diagnosing postthrombophlebitis syndrome
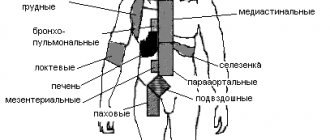
First, the doctor must determine the presence of thrombosis and the degree of disruption of the lumen of the vessels. It is also important to assess trophic disorders in the distal parts of the lower extremities. The doctor conducts this study during the initial and subsequent examinations of the patient. In addition, it is necessary to take blood tests and undergo several modern studies. The main problem is that not every patient suffering from thrombosis seeks medical help even in Moscow and the Moscow region. Today, the main way to study veins is ultrasound angioscanning.
Diagnosis of postthrombophlebitic disease PTF
Thus, it is possible to determine the presence of thrombus remnants, check the condition of the valves, and assess the nature of the blood flow. Nevertheless, for better diagnosis of post-thrombophlebitis disease, other European methods are already used. The leading methods for visualizing postthrombotic obstruction are: multislice computed tomography and intravascular ultrasound scanning (IVUS). These state-of-the-art medical technologies allow the most accurate assessment of obstruction and innovative treatment. These techniques are available in Moscow and the Moscow region, the regional centers of our state.
Clinical forms of postthrombotic disease of the lower extremities
- Edema form
Edema - the affected limb is increased in volume compared to the healthy one. During the day, swelling increases and reaches a maximum in the evening. After an overnight rest, the swelling decreases. If the symptoms of postthrombotic disease are dominated by edematous syndrome, then this form is called edematous. Swelling may be accompanied by heaviness in the leg and pain - this form is called edematous-painful.
- Ulcerative form
Prolonged venous stagnation leads to darkening of the skin and the appearance of trophic ulcers. Trophic ulcers in postthrombotic disease are very difficult to treat and gradually progress. Pain syndrome often develops against the background of deep ulcers. This form of postthrombotic disease is called peptic ulcer.
Prognosis for postthrombotic disease
The ulcerative form of PTFS has an unfavorable prognosis. Persistent healing of a trophic ulcer occurs very rarely. Surgical treatment is quite complex, but can be successful in most patients.
Extensive trophic ulcers develop in 40% of patients with postthrombotic disease. This problem can be complicated by the development of chronic intoxication, when the ulcer does not heal for years and leads to the development of a specific lesion - amyloidosis of internal organs. This condition leads to death from multiple organ failure.
Damage to bones and joints complicates the situation and leads to amputation of the limb. A similar outcome is observed in 10% of patients with the ulcerative form of postthrombotic disease.