Quick transition Treatment of heart attack
Myocardial infarction (heart attack) is an acute, life-threatening condition caused by a decrease or complete cessation of blood supply to the heart as a result of blocking one of the coronary arteries with a blood clot (thrombus) and the development of one or more foci of necrosis in the heart muscle.
A heart attack is a clinical form of coronary heart disease (CHD), a disease characterized by impaired blood supply to the myocardium as a result of damage to the coronary arteries.
A patient with symptoms of myocardial infarction needs emergency pre-medical and medical care. Not only his successful recovery from a heart attack, but also his life depends on this.
A heart attack can occur at rest (rest or sleep), after intense physical activity, with increased activity in cold weather, after severe emotional or physiological stress (including various diseases).
Causes
The most common cause of myocardial infarction is long-term atherosclerotic damage to the walls of blood vessels (narrowing of the lumen of the arteries due to the deposition of atherosclerotic plaques consisting of cholesterol and lipoproteins on their walls), which provokes insufficiency of blood supply to the myocardium. A heart attack can cause vascular thrombosis; prolonged spasm of the coronary artery (not affected by atherosclerosis), associated with taking drugs, stress, painful shock, exposure to cold, smoking; lack of oxygen in the blood (hypoxia); heart disease; blockage of an artery during surgery.
Risk factors
Unchangeable factors include:
- age (risk increases with age);
- gender (in men the risk of heart attack is higher, in women it increases and approaches “male” indicators in the postmenopausal period);
- genetic predisposition (heart disease in close relatives);
- race (for example, African Americans have a higher risk).
Modifiable (changeable) risk factors, i.e. factors that a person can influence:
- smoking (if you smoke, it is important to quit this habit);
- limiting the consumption of alcoholic beverages;
- control cholesterol levels, high blood pressure, diabetes (through proper nutrition, exercise, medications);
- playing sports, any physical activity (walking, cycling, cardio exercises);
- maintaining normal weight;
- a healthy diet (fruits, vegetables, whole grains, lean meats and milk, reducing the amount of salt consumed, eliminating fried and processed foods, foods containing saturated and hydrogenated fats, moderate consumption of sweets and baked goods);
- avoiding stress.
Symptoms
The most common “warning” symptoms of a heart attack:
- pain or discomfort in the chest (usually for several minutes, repeated attacks, sometimes reminiscent of dyspepsia or heartburn);
- chest pain spreading to the arm(s), shoulders (between the shoulder blades), neck, lower jaw, epigastric region;
- severe shortness of breath (during physical activity or at rest, before the onset of chest pain or simultaneously with them).
An attack of pain may be accompanied by profuse sweating, weakness, nausea and vomiting, dizziness, increased heart rate, rhythm disturbances, a sharp increase and then a decrease in blood pressure. And also intensify or be supplemented by other symptoms that did not appear before.
The clinical manifestations of a heart attack vary from person to person, and the acute condition is not always accompanied by chest pain and discomfort and other common symptoms. At the slightest suspicion of a heart attack, immediately call an ambulance.
Complications
Complications (or consequences) of a heart attack are associated with damage to the myocardium during a heart attack. These include: heart rhythm disturbances (type 1 arrhythmia can cause sudden cardiac arrest); cardiogenic shock; heartbreak. These complications develop quite quickly and are the main cause of death from heart attack. The prognosis depends on how quickly after a heart attack the patient received first aid, his age, and the severity of the infarction (size and location of the focus of myocardial necrosis).
Diagnostics
The diagnosis of myocardial infarction is established on the basis of the patient's symptoms and complaints, family history, electrocardiographic signs (signs of a heart attack on the ECG) and laboratory diagnostic results (identify certain proteins and enzymes that indicate myocardial damage). Typical blood tests used to diagnose a heart attack include a serum myoglobin test, a troponin test, and a creatine phosphokinase level.
The patient may also be prescribed coronary angiography with a contrast agent to assess the speed of blood flow, the condition of the coronary arteries and identify areas of their narrowing; CT or MRI of the heart - for the same purpose and to assess the structures and function of the organ.
Diagnostic methods
Physical examination
The primary diagnosis of myocardial infarction, which will be carried out by the arriving doctors, consists, first of all, of examining the patient and asking about health complaints. This disease can be confused with an attack of angina, especially if it appears for the first time. The nature of the pain is similar - they spread from the sternum to the left arm (including fingers), shoulder, shoulder blade, neck, jaw. The difference between a heart attack is more severe and acute pain, which is not relieved by taking nitroglycerin.
Pain syndrome during myocardial infarction can last about a day, accompanied by weakness, a drop in blood pressure, and vomiting. The patient is in emotional arousal, in contrast to an attack of angina, when patients, on the contrary, try to move as little as possible.
The doctor measures pressure (most often it decreases by 10-15 mm) and pulse, checks for possible dysfunction of the left ventricle and myocardium, listening to heart sounds.
Lab tests
At the hospital stage, the diagnosis of a heart attack consists of conducting biochemical and general blood tests. With this disease, noticeable changes occur in the composition of the blood:
- the level of leukocytes, ALT, AST, cholesterol, fibrinogen levels increase;
- the erythrocyte sedimentation rate and albumin indicator decrease.
These are indicators of necrosis, scarring of cardiac muscle tissue and the presence of inflammation. The patient has polymorphic cell leukocytosis.
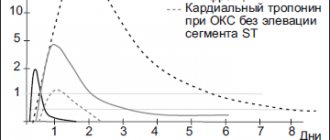
The laboratory method for diagnosing myocardial infarction also checks the level of serum enzymes. Markers appear in it indicating myocardial necrosis, in particular the contractile protein troponin, which is not found in a healthy person. Markers also include CPK and myoglobin, which appear in the blood serum in the first hours after the onset of the disease.
A number of biochemical reactions in the blood are not specific to a heart attack, so it is extremely important to entrust the diagnosis to highly qualified doctors and a clinic with extensive technical capabilities.
Electrocardiography
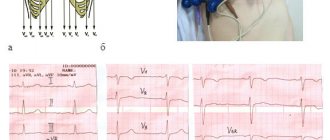
ECG for myocardial infarction is one of the most effective, objective and informative diagnostic methods. If possible, seek emergency help from the doctors of the cardiology team - their car must be equipped with a portable electrocardiograph, which will allow you to diagnose the disease as soon as possible.
ECG equipment picks up the electrical impulses generated by the heart muscle and records them on paper. Based on the analysis of the cardiogram, a qualified doctor can determine:
- localization of necrosis (posterior, anterior or lateral wall, septum, basal wall, etc.);
- the size and depth of the lesion;
- process stage;
- complications that have arisen.
The doctor pays attention to the nature of the electrocardiogram waves and analyzes the increase in the level of individual segments. In particular, large-focal transmural myocardial infarction is characterized by the appearance of a pathological Q wave.
The examination takes about 10 minutes and does not cause any discomfort. During a heart attack, an ECG may be performed every half hour to provide continuous data updates.
Echocardiography
The more common name for echocardiography among patients is cardiac ultrasound. This is an extremely effective tool for diagnosing acute myocardial infarction and other types of this pathology.
The examination is not associated with painful sensations and takes 20-25 minutes. The doctor lubricates the patient’s chest with a special gel and moves an ultrasonic sensor over it. The echocardiograph reads the data obtained on the state of the myocardium, pericardium, large vessels, and valves, and the doctor immediately analyzes them. The advantage of the method is the ability to visually assess the functionality of the organ in the shortest possible time and diagnose regional contractility disorders.
The Doppler mode in which modern ultrasound machines operate makes it possible to assess the quality of blood flow in the heart and determine the presence of blood clots. The sound signals of the heart are also analyzed, the pressure in the organ cavities is measured, and complications are studied.
Radiography
To objectively predict the development of complications during myocardial infarction, a chest x-ray is performed as part of the diagnosis.
Among the dangerous complications, this method most often diagnoses pulmonary edema, which is one of the clear signs of acute left ventricular failure. The image shows impaired blood flow in the upper parts of the lungs, pulmonary artery, blurry pattern of blood vessels, etc. Also, with a heart attack, dissection of the aorta and other changes in the thoracic part are likely. Radiography allows you to diagnose disorders of the blood supply to organs located in close proximity to the heart.
Among the radiological methods used in cardiology to determine a heart attack, coronary angiography and multislice computed tomography of the heart are also common. With their help, the location and nature of the narrowing of the coronary artery is determined.
Treatment of heart attack
While waiting for an ambulance to arrive, a person with signs of a heart attack can take aspirin (300 mg) if they are not allergic to this drug. Aspirin thins the blood and increases blood flow to the heart. At the medical institution, the patient is provided with immediate assistance: the pain attack is stopped, thrombolytic and anticoagulant therapy is performed (drugs that restore blood flow by dissolving blood clots, preventing their formation), antiarrhythmic therapy or (if necessary) surgery to restore coronary blood supply.
The time required to recover from a heart attack depends on the degree of myocardial damage. Some patients recover within 2 weeks, others may take several months. Rehabilitation after a heart attack is aimed at reducing the risk of relapse; lifestyle changes are recommended (healthy diet, exercise, quitting smoking and alcohol), and statins are prescribed - drugs that lower blood cholesterol levels.
LABORATORY DIAGNOSTICS FOR HEART DISEASES
There are three groups of indicators:
— Indicators characterizing risk factors for atherosclerosis;
— Nonspecific indicators of stress reaction and necrosis of the heart muscle;
— “Cardiospecific” indicators of cardiomyocyte death.
The first group includes laboratory signs of atherosclerosis:
1) increase in the level of total cholesterol in the blood > 5 mmol/l;
2) increased LDL cholesterol levels > 3 mmol/l;
3) reduction in HDL cholesterol < 1.0 mmol/l;
4) increase in TG level > 1.7 mmol/l.
Second group:
1) leukocytosis 12 – 15*10 9/l, maximum on days 2 – 4 of myocardial infarction, decreases by the end of the week;
2) increase in ESR from 2 – 3 days;
3) by the end of the first week of myocardial infarction, the graphic representation of the leukocyte level and ESR intersect “scissors symptom”. The level of α2 globulins and fibrinogen increases.
Third group: biomarkers of cardiomyocyte death
1) myoglobin - the earliest indicator - increases after 2 hours.
2) troponins I and T - the “gold standard” of diagnosis. If in the first hours of myocardial infarction the level of troponins is normal, then it is necessary to repeat the analysis after 6–12 hours.
3) creatine kinase - MB fraction - specific, but not sensitive. It increases only with large focal myocardial infarctions.
Determination of the level of AST and LDH is not included in the mandatory diagnostic program, since these enzymes are nonspecific (increased in other conditions). Na and K levels indicate whether there are abnormalities in the heart rhythm. Sputum in cardiovascular failure is scanty, pink, with a large number of reticuloendothelial cells (so-called macrophages). The addition of a secondary infection leads to the development of purulent processes and the appearance of clots of yellowish sputum and mucus, which is always very viscous and thick.
Recommended tests for ischemic heart disease: angina pectoris, myocardial infarction, post-infarction cardiosclerosis, arrhythmias and heart block, heart failure.
1) General blood test - changes during the acute period of MI and its complications (pericarditis, endocarditis, thromboembolism, congestive pneumonia). Leukocytosis, accelerated ESR, and anemia develop.
2) General urine analysis - with congestive heart failure, there may be the appearance of protein, leukocytes, and red blood cells. There is a decrease in urine volume (oliguria), and nocturnal diuresis (nocturia) appears.
3) Biochemical blood test - the content of total cholesterol, cholesterol - LDL, TAG often increases.
4) Blood coagulogram - with ischemic heart disease, as a rule, the blood coagulation system worsens. A number of indicators (APTT, INR), D-dimers and others must be monitored during treatment with anticoagulants (heparin, warfarin, fraxiparin).
5) Markers of heart damage - in case of necrosis of the heart muscle caused by myocardial infarction, the most informative indicator is the determination of troponin, myoglobin, creatine phosphokinase, LDH1,2 fraction (HBDN), CRP (nonspecific test).
6) Blood electrolytes – K, Na, Ca, CL. These indicators must be determined in case of arrhythmias and heart blocks, as well as during treatment with diuretics, which can wash them out of the body and in other concomitant conditions (renal failure).
Recommended tests for myocarditis.
1) General blood test - leukocytosis with a shift of the formula to the left may be observed (the appearance of band neutrophils, an increase in the number of segmented neutrophils). Acceleration of ESR.
2) Biochemical blood test - the content of myocardial enzymes increases - CPK (due to the CPK-MB fraction), LDH (due to the LDH fraction, 1), troponin I. An increase in CRP, an increase in α and β globulins may be observed.
4) Tests for antibodies to viruses that can infect the myocardium are prescribed if a specific infection is suspected. These can be viruses, adenoviruses, influenza, measles, mononucleosis infections, CMV, HIV.
5) Tests for bacteria. The causes of myocarditis can be diphtheria bacillus, streptococcus, staphylococcus, gonococcus, clostridia, etc. Therefore, with a corresponding infection, one should not forget about the effect of these microbes on the heart, especially in severe forms of the disease (sore throat, pneumonia).
4) Other tests for pathogens that cause myocarditis - fungi (candidiasis of the heart), rickettsia, spirochetes, toxoplasma, amoeba, schistosomes, toxoplasma. Syphilis most often affects the valve apparatus of the heart.
For hypertension it is recommended to take:
1) General analysis of blood and urine.
2) Biochemical blood test - including cholesterol, LDL cholesterol, HDL, TAG, creatinine, urea, glucose.
3) Blood electrolytes - especially with periodic monitoring during treatment with diuretics.
4) Coagulogram - with hypertension there is a tendency to increase the blood coagulation system.
Laboratory Diagnostics Doctor, Central House of Writers
Novopolotsk city hospital
Afanasenko A.P.
Prevention of heart attack
Prevention of heart attack is based on reducing modifiable risk factors for coronary heart disease. Changing lifestyle, receiving timely medical care and taking prescribed medications for concomitant diseases (diabetes, hypertension, chronic kidney disease, peripheral arterial disease, high cholesterol), proper nutrition, normalizing weight, regular exercise, giving up bad habits will help prevent heart disease attack (including repeated).
Blood tests that determine the risk of heart attack and stroke
The blood tests below help determine the risk of developing coronary heart disease, stroke , peripheral vascular disease and, if necessary, prescribe treatment.
Lipoprotein A ( Lp (a)) is a blood protein whose levels indicate an increased risk of heart attack and stroke.
Normal value:
Desired level for adults: no more than 30 mg/dl.
Preparing for the analysis:
Blood is taken for analysis after a 12-hour fast (except for drinking water). To get more accurate results, you should refrain from taking the test for at least two months after a heart attack, surgery, infection, injury, or pregnancy.
Lipoprotein A is a low-density lipoprotein (LDL) that has a protein called apo attached to it. Currently, it is not fully known what function lipoprotein A performs in the body, but it is known that blood levels of lipoprotein A higher than 30 mg/dl increase the risk of developing myocardial infarction and stroke. In addition, high levels of lipoprotein A can lead to the development of fat embolism and increases the risk of developing blood clots.
It is especially important to bring the level of LDL (low-density lipoprotein) to normal if the content of lipoprotein A is high. The causes of high levels of lipoprotein A are kidney disease and some familial (genetic) disorders of lipid metabolism. Apolipoprotein A1 (A p o A1) is the main protein of HDL (high density lipoprotein). Low levels of apolipoprotein A1 indicate an increased risk of early cardiovascular disease. Apo 1 is more often reduced in patients suffering from physical inactivity, obesity, or eating a high amount of fat.
Normal value:
Desired level for an adult: more than 123 mg/dl.
Preparing for the analysis:
Blood should be drawn for testing after a 12-hour fast (excluding drinking water). To get more accurate results, you should refrain from taking the test for at least two months after a heart attack, surgery, infection, injury, or pregnancy.
Apolipoprotein B (a p oB) is the main protein found in cholesterol. ApoB is a better overall marker of cardiovascular risk than LDL, a new study suggests.
Normal value:
Less than 100 mg/dL for low/moderate risk individuals. Less than 80 mg/dL for those at high risk, such as those with cardiovascular disease or diabetes.
Preparing for the analysis:
Blood should be drawn for testing after a 12-hour fast (excluding drinking water). To get more accurate results, you should refrain from taking the test for at least two months after a heart attack, surgery, infection, injury, or pregnancy.
Fibrinogen is a protein found in the blood and involved in the blood clotting system. However, high fibrinogen levels may increase the risk of myocardial infarction and vascular disease.
Normal value:
Less than 300 mg/dl.
Preparing for the analysis:
Blood should be drawn for testing after a 12-hour fast (excluding drinking water). To get more accurate results, you should refrain from taking the test for at least two months after a heart attack, surgery, infection, injury, or pregnancy.
Elevated levels of fibrinogen are more often detected in older patients, in patients with high blood pressure, body weight and LDL. On the other hand, lower levels of fibrinogen are detected in patients who drink alcohol and regularly undergo physical activity. An increase in fibrinogen levels occurs with menopause.
High-sensitivity C-reactive protein (protein) (CRP ) is a protein found in the blood that is called an “inflammatory marker,” meaning its presence indicates an inflammatory process in the body. Inflammation is a normal response to many physical conditions, including fever, injury, and infection. But the inflammatory process, localized in the vessel wall, plays an important role in the initiation and progression of cardiovascular diseases. Inflammation (ie, swelling and damage) of the inner wall of the arteries is an important risk factor for the development of cardiovascular diseases such as atherosclerosis, myocardial infarction, sudden death, stroke, blood clots, and peripheral artery disease.
In the Harvard University Health Study, elevated CRP levels were a more accurate marker of coronary heart disease than cholesterol levels. The study assessed twelve different markers of inflammation in healthy postmenopausal women. After three years, C reactive protein was the strongest predictor of risk. Women in the group with the highest CRP levels were more than four times more likely to die from coronary heart disease or suffer a nonfatal heart attack or stroke.
More recently, the JUPITER (Justification for Statins in Primary Prevention) study showed that statins prevent heart disease and reduce the risk of stroke, heart attack, and death in individuals with normal LDL (bad cholesterol) levels but elevated high-sensitivity C-reactive protein (CRP) levels. ).
While elevated levels of cholesterol, LDL and triglycerides and low HDL are independent risk factors for heart disease, high-sensitivity C-reactive protein provides additional information about the inflammatory process in the arteries that cannot be determined by the lipid spectrum.
Normal value:
Less than 1.0 mg/l = low risk of cardiovascular disease; 1.0 - 2.9 mg/l = intermediate risk of developing cardiovascular diseases; more than 3.0 mg/l = high risk of developing cardiovascular diseases.
CRP levels of 50 mg/L or higher are sometimes detected, but usually CRP levels above 10 mg/L are due to another inflammatory process, such as infection, injury, arthritis, etc.
Therefore, testing should not occur during illness or injury. CRP should be studied to assess the risk of developing cardiovascular disease in apparently healthy individuals who have not had a recent infectious disease or other serious illness. Those patients whose CRP level during the study was above 10 mg/l should be examined to identify the source of the inflammatory process.
Preparing for the analysis:
This test can be performed at any time of the day, without any preparation. The only condition is the absence of acute inflammation.
Myeloperoxidase (MPO) is a marker of the inflammatory process in the arteries. As a result of this process, destruction of atherosclerotic deposits in the vessel wall often occurs, leading to thrombosis. A high level of myeloperoxidase, in combination with other risk factors (CRP, LDL, high blood pressure, excess weight) is an accurate criterion for an increased risk of heart attack, myocardial infarction, sudden death, stroke or peripheral vascular disease, including in apparently healthy people .
Normal value:
Less than 400 microns.
Preparing for the analysis:
This test can be done at any time of the day and does not require fasting.
N -terminal pro-brain natriuretic peptide (N-proBNP, NT- proBNT) is a peptide that is produced in the atria and ventricles of the heart in response to increased compliance of cardiomyocytes and increased pressure in the chambers of the heart. By measuring the concentration of NT-proBNP, one can judge the amount of brain natriuretic peptide synthesized. NT-proBNT level correlates closely with left ventricular ejection fraction and pulmonary artery systolic pressure. NT-proBNP levels indicates a high probability of heart failure and the advisability of appropriate examination to confirm the diagnosis.
Normal value:
Less than 125 pg/ml.
Preparing for the analysis:
This test can be done at any time during the day and no fasting is required.
Level of lipoprotein-associated phospholipase (LP-PLA2, PLAC).
High levels of lipoprotein-associated secretory phospholipase a2 (LP-PLA2) indicate an increased risk of developing cardiovascular diseases. However, in some cases, the cause of the elevated levels may not be an arterial cause.
Normal value:
Less than 200 ng/ml - relatively low risk of developing cardiovascular diseases;
Between 200-235 ng/ml - average risk of developing cardiovascular diseases;
More than 235 ng/ml - high risk of developing cardiovascular diseases.
Preparing for the analysis:
Blood should be drawn for testing after a 12-hour fast (excluding drinking water). To get more accurate results, you should refrain from taking the test for at least two months after a heart attack, surgery, infection, injury, or pregnancy.
The ratio of albumin to creatinine in urine. (Ualb/Cr). The appearance of albumin in the urine is a sign of kidney disease, diabetes and cardiovascular complications.
Normal value:
More than 30 mg/g indicates an increased risk of cardiovascular disease and diabetic nephropathy.
More than 300 mg/g indicates clinical nephropathy.
Preparing for the analysis:
A urine test can be done at any time during the day and does not require fasting.
Features and advantages of treatment of myocardial infarction at the Rassvet clinic
Dawn cardiologists are engaged in primary and secondary prevention of cardiovascular diseases, including myocardial infarction.
Our clinic is equipped with modern equipment for diagnosing heart disease and identifying increased risk of cardiovascular pathologies, including digital electrocardiographs, digital X-rays, high-end ultrasound and echocardiography. For patients diagnosed with CVD, our doctors develop secondary prevention measures aimed at preventing complications and relapse of the disease. Cardiovascular pathologies are treated according to the protocols of European and American Heart Associations with proven effective drugs.
Laboratory diagnosis of myocardial infarction and other cardiovascular markers
Prevention of myocardial infarction:
I. Study of the hemostatic system.
Basic coagulogram parameters:
- Fibrinogen (normal 2.0 - 5.0 g/l), in pregnant women its level increases and reaches 6.0 g/l at the end of the third trimester. Blood plasma without fibrinogen is called blood serum. It increases in the blood during myocardial infarction and decreases during disseminated intravascular coagulation syndrome.
- Prothrombin time - shows the external coagulation pathway, normally 11 - 14 seconds. An increase indicates a tendency to hypocoagulation, a decrease - to hypercoagulation. Expressed as prothrombin index (PTI, normal 93-107%) and INR (international normalized ratio).
- Activated partial thromboplastin time (aPTT) is a screening test for assessing the activity of certain coagulation factors, as well as the effectiveness of heparin therapy, normally 24 - 36 seconds.
- Thrombin time characterizes the final stage of the coagulation process - the conversion of fibrinogen into fibrin, normally 8 - 14 seconds.
Additional hemostasiogram parameters:
- D-Dimer . Its fragments are formed as a result of the destruction of a blood clot, the norm is up to 0.5 mcg/ml.
II. Study of lipids to prevent the risk of atherosclerosis.
- Total cholesterol is a fat-like substance that is part of cell membranes. Its level is higher than normal (more than 5.0 mmol/l) - the main indicator of the risk of developing atherosclerosis.
- High-density lipoproteins ( HDL, α-lipoproteins ) and low-density lipoproteins ( LDL, β-lipoproteins ). HDL is antiatherogenic, normally 1.04 - 1.55 mmol/l. LDL is capable of transporting cholesterol into cells, therefore they are the most atherogenic, their level is normally less than 2.59 mmol/l.
- Apolipoprotein A1 (APO-A1) is a blood plasma protein that is part of high-density lipoproteins and is an indicator of the risk of cardiovascular diseases; normal women: 107.0 - 205.0 mg/dl; men: 107.0 - 177.0 mg/dl.
- Apolipoprotein B (APO-B) is a carrier of “bad cholesterol”, which causes cholesterol to accumulate in the walls of blood vessels. The accumulation of APO-B in the blood leads to the development of atherosclerosis. The concentration of APO-B in the blood is a more reliable indicator of the risk of atherosclerosis than total cholesterol or LDL cholesterol. Normal: women: 52.0 - 129.0 mg/dl; men: 60.0 - 138.0 mg/dl.
- Triglycerides are a type of fat that provides us with energy. Knowing your optimal triglyceride levels is important because elevated levels can put you at risk for a heart attack or stroke, up to 1.7 mmol/L.
- The atherogenicity coefficient is the main indicator by which one can judge disorders and determine the prognosis; it should not exceed 3.0.
New in laboratory medicine:
- Homocysteine is a sulfur-containing amino acid in blood plasma. High homocysteine levels increase the risk of heart disease, stroke, Alzheimer's disease and osteoporosis. Acts as a marker of homocysteinuria, a rare hereditary disease, the result of its development is early cardiovascular diseases.
- NT-proBNP or brain natriuretic peptide is a hormone that is produced in the atria and ventricles of the heart in response to increased elongation of cardiomyocytes and increased pressure in the chambers of the heart, and is determined in the blood serum.
Diagnosis of myocardial infarction:
- Myoglobin is an iron-containing protein of muscle cells; an increase in blood levels is observed within 2-3 hours after the onset of pain during MI and persists for up to 2 days. Myoglobin levels are the first of all MI markers to increase; its concentration in the blood can increase 4-10 times or more.
- Creatinine phosphokinase is an enzyme that plays an important role in the energy metabolism of muscle, nervous and other tissues; in particular, its subunit MB-fraction, which is found in large quantities in the heart muscle and acts as a marker of MI, showing maximum activity 20 hours after the onset of the first symptoms and decreases to normal after 40 - 50 hours from their onset. KFK-MV norm is up to 24.0 U/l.
- The enzyme lactate dehydrogenase (LDH) is involved in the final stages of glucose conversion and is one of the main enzymatic tests in the laboratory diagnosis of late MI, as it increases in the interval 8–12 hours from the onset of a painful attack, reaches a maximum after 24–48 hours, remaining elevated for 7 or more days. Its increase is usually observed 3-4 times higher than the upper limit of the reference values, but can be 10-fold. LDH levels may be moderately increased in myocarditis and heart failure with liver congestion. The norm in our laboratory is 225.0 - 450.0 U/l.
- 1st LDH isoenzyme (LDH-1, α-hydroxybutyrate dehydrogenase (HBDH) ). An increase in GBDG-α during the first three days after the onset of pain makes it more likely to diagnose MI. 46 - 20 hours after a painful attack, when the total LDH activity does not yet go beyond the reference values, an increase in GBDG-α is observed, and its activity may remain increased after the total LDH activity has already returned to normal. Norm < 182.0 U/l.
- Also, in typical cases of acute myocardial infarction, serum AST activity becomes higher than the normal level 6–12 hours after the onset of clinical signs, reaches a maximum (8–10 times higher than normal) after 18–36 hours and returns to the initial level before 3–4 days of illness.
- Troponin I is more specific and reliable than traditional cardiac enzymes, particularly CK or CK-MB. In patients with MI, an initial increase in the concentration of troponins in peripheral blood is observed after 3-4 hours, its level persists for up to 6 days.