Hydropericardium - what is it?
Hydropericardium is an abundant accumulation of fluid in the heart sac. This bag itself consists of two leaves surrounding the heart. Their task is to protect it and separate it from other organs. Fluid accumulates in the middle of the sac (called the pericardium). Its amount is insignificant, and it is designed to prevent friction of the walls of the bag against each other, as well as the heart. For normal conditions, the leaves are 3-5 millimeters apart from each other, the amount of accumulated liquid is up to 50 milligrams.
If there is too much fluid, it prevents the heart from working normally, which can lead to cardiac tamponade and cardiac arrest.
The disease we are talking about dramatically increases the amount of natural fluid in the heart sac by several times. If the natural amount of liquid mass ranges from 15 to 50 milligrams, then in a pathological condition this amount can be over a liter. In addition, when pathology develops, blood or lymph enters the bag.
Causes of hydropericardium
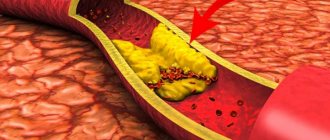
Normally, fluid (transudate) is produced by the cells lining the pericardium from the inside, and is reabsorbed by them. Its quantity increases in two cases - with increased production or slower absorption. Many diseases can lead to this disorder:
- chronic heart failure;
- pericarditis;
- cardiomyopathy;
- congenital malformations of the heart and pericardial sac;
- a decrease in blood protein levels, which occurs in many diseases;
- hypothyroidism;
- allergy;
- injuries;
- anemia;
- radiation therapy;
- chronic renal failure;
- tumors of the mediastinum (the place in the chest where the pericardium and heart are located).
There are special forms of hydropericardium in which fluid accumulates and:
- lymph (chylopericardium – a consequence of blocking the flow of fluid through the lymphatic vessels; occurs during metastasis of malignant tumors);
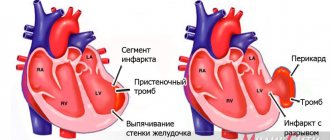
- blood (hemopericardium; causes - trauma to the heart or pericardial vessels, myocardial infarction, obesity).
Why does pericarditis occur?
The following are the main causes of pericarditis:
- Infectious agents: viruses, bacteria, fungi and even parasites. The inflammatory process in the pericardium is triggered by the influence of exo- and endotoxins released by microorganisms.
- Autoimmune connective tissue diseases such as lupus erythematosus or scleroderma. At the same time, the body synthesizes antibodies to its own cells, which damage connective tissue and cause systemic inflammation.
- Heart diseases. The result of serious damage to the heart muscle is the spread of the pathological process to the surrounding pericardium. This can occur with transmural myocardial infarction, infectious or reactive myocarditis.
- Damage to other organs, such as the kidneys, can lead to pericarditis. In cases of serious impairment of excretory function and the formation of renal failure, deposition of metabolic products in the serous cavities, including the pleura and pericardium, is observed.
- Penetrating pericardial injuries that disrupt the integrity of the pericardial layers.
- Metastatic tumors that cause pericardial carcinomatosis.
- The causes of pericarditis are varied, and, therefore, treatment approaches depend on what caused the inflammation. But in the absence of timely diagnosis and correction of this condition, the outcome is always the same. The result of chronic pericarditis is cardiac tamponade, which leads to the death of the patient.
At CELT you can consult a cardiologist.
- Initial consultation – 3,500
- Repeated consultation – 2,300
Make an appointment
Signs of hydropericardium
With this syndrome, the onset of symptoms does not begin immediately. At first, only signs of the disease that caused the hydropericardium are noticeable. With a small accumulation of fluid, it does not manifest itself in any way, but as its amount increases, the heart is compressed and it is impossible to contract. Main manifestations:
- shortness of breath at rest or with minimal effort;
- increased heart rate;
- edema syndrome;
- decreased blood pressure due to decreased cardiac output;
- pallor of the skin, blueness of the lips and the space between the upper lip and nose (acrocyanosis of the nasolabial triangle).
With massive hemopericardium, the vagus nerve adjacent to the esophagus is irritated and then painful hiccups can occur. This is a sign of a life threat, and in this case it is necessary to immediately call an ambulance.
In case of hemopericardium due to injury, a critical condition may occur - cardiac tamponade. In this case, the heart contractions are not enough to push blood through the vessels, and the person may die within a few minutes. Dobrobut.com clinic specialists recommend studying cardiopulmonary resuscitation measures and using them in such cases - this is the only chance to save a person before specialists arrive. If symptoms of tamponade appear, you should immediately call a doctor. Symptoms:
- a sharp decrease in pressure, especially with loss of consciousness;
- feeling of lack of air with frequent shallow breathing;
- weakness, darkening of the eyes;
- feeling of heartbeat;
- fear of death, overexcitement
Possible complications
The development of complications of hydropericardium is associated with the severity of heart failure.
An increase in the volume of pathological effusion to 1-1.5 liters provokes an increase in symptoms: pressure numbers decrease, shortness of breath worsens, and swelling becomes more noticeable. Advanced hydrocele of the heart leads to the development of tamponade, in which accumulated fluid compresses the heart muscle so much that physiological contractions become impossible. The clinical picture of the condition is accompanied by a pronounced loss of strength, weakness, attacks of suffocation with frequent shallow breathing, a feeling of rapid heartbeat, and episodes of loss of consciousness. In such a case, emergency medical attention is required.
Diagnosis of hydropericardium
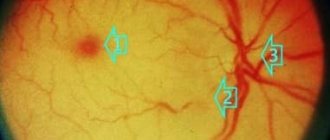
The main method for diagnosing this condition is ultrasound. Echocardiography in the area in the area of the posterior wall of the left ventricle of the heart can reveal a discrepancy between the parietal and visceral layers of the pericardium, which is normally 5 mm. An increase in this distance clearly indicates the presence of liquid between the sheets. Criteria for echodiagnosis of hydropericardium:
- 6-10 mm divergence of the leaves is the early stage of hydropericardium;
- 10-20 mm – moderate stage;
- over 20 mm – pronounced stage.
In the latter case, an additional puncture of the pericardium is performed with suction of part of the fluid and study of its nature (inflammatory exudate, lymph, blood, etc.)
Echocardiography can also identify hydropericardium in the fetus during pregnancy. In this case, the diagnostician should suspect a congenital heart defect in the unborn newborn or a hemolytic disease. In this case, the woman should be thoroughly examined and, if necessary, undergo a course of appropriate treatment under the supervision of specialists.
In addition to ultrasound, to diagnose diseases that have led to a worsening of the condition, you will have to undergo other studies:
- chest x-ray;
- general urinalysis and complete blood count;
- thyroid hormone levels;
- blood protein level;
- ECG, etc.
Symptoms
Depending on the cause that caused the accumulation of effusion in the pericardium, the symptoms of this phenomenon will vary, but all forms of the disease are characterized by the severity of symptoms depending on the stage of the disease.
At the stage of mild hydrocephalus, the accumulation of fluid in the pericardial sac is asymptomatic. Chest discomfort appears at the stage of moderate hydrocephalus.
When symptoms worsen
During the major hydrocephalus stage, the heart is compressed, impairing its ability to relax.
Symptoms of the third stage of the disease are:
- shortness of breath;
- rapid pulse;
- swelling of the face;
- swelling of the limbs;
- cold sweat;
- low blood pressure;
- stimulation;
- fast, shallow breathing;
- bright colors of mucous membranes and skin.
The continued flow of exudate into the pericardial sac increases the volume of the organ so that it narrows the esophagus, preventing the passage of the bolus, causing prolonged hiccups. This condition is life-threatening; you must immediately call an ambulance without wasting time on self-medication.
Features of the disease
Usually, in the early stages of hydrocele, there are no complaints of pain, and auscultation of the heart does not reveal the sounds of pericardial friction; only light tapping is heard.
Fluid accumulation in the pericardium does not always worsen heart disease. In some diseases, a small amount of transudate in the pericardial sac has a stabilizing effect on the heart muscle and has a supporting effect in severe heart failure.
Treatment of hydropericardium
The underlying disease is what the doctor should first pay attention to. Treatment of heart failure, taking medications containing thyroid hormones, restoring protein levels are all methods of treating the disease that caused the hydropericardium. Often this approach is enough to relieve the patient of this symptom.
There may be situations when there is not enough time to wait for the effect, and then it is necessary to supplement the treatment of the underlying disease by combating the hydropericardium directly. Initially, diuretics are used - potassium-sparing (spironolactone, triamterene, hydrochlorothiazide) or thiazide diuretics (furosemide, torsemide) in combination with potassium supplements. If there is no result and if the volume of fluid is critical, it is possible to perform a pericardial puncture with pumping out excess exudate.
Hydropericardium is a symptom or complication. The underlying disease that led to the appearance of this symptom needs to be treated. And it is best to prevent the development of such complications, for which you should consult a doctor if there are any signs of trouble in the body.
Related services: Cardiac examination
Stages and forms
The degree of development of hydrocephalus varies depending on the amount of effusion accumulated in the pericardial sac.
- Minor hydrocephalus - the volume of fluid does not exceed 100 ml;
- moderate - volume from 100 ml to 500 ml;
- large - the volume of transudate exceeds 500 ml.
At the third stage, up to 1 liter of transudate can accumulate in the pericardial sac.
Depending on the characteristics of the permeate composition, the following forms are distinguished:
- Hemopericardium - blood accumulates in the pericardium. This phenomenon occurs when the blood vessels supplying the pericardial tissue rupture, a heart attack, trauma, or obesity of the heart;
- Chylopericardium - when the lymphatic ducts are compressed, the outflow of lymph is disrupted, and lymphatic fluid accumulates in the pericardium.
Forecast
{banner_banstat10}
Determined by the degree of impairment, timeliness of treatment and underlying disease. Hydropericardium of the 1st degree is easily treated, survival rate is maximum.
The third degree, especially if the transudate volume is over 500 ml, is associated with high mortality. Approximately 60-70% without quality timely intervention.
If it is possible to completely cure the etiological factor, they speak of good prospects. Otherwise, constant monitoring by a cardiologist will be required, as relapses are likely. Even the best specialist won’t say when exactly.
Clinical picture
If the fluid content in the pericardial cavity is low, the person does not notice anything. The condition worsens when there is 80–100 ml in the “bag”. Patients experience pressure in the front behind the sternum, which increases when the torso is tilted forward.
Further symptoms of impaired cardiac activity appear:
- general weakness;
- shortness of breath independent of physical activity;
- pain behind the sternum of a pressing nature, very long-lasting due to compression of the coronary vessels and increasing myocardial ischemia;
- paroxysmal suffocation;
- the face and hands are swollen and look puffy;
- swelling on the feet and legs increases.
The neck veins become visible without palpation
When examining a patient, the doctor pays attention to:
- pulsating veins in the neck (due to compression of the mouth of the vena cava);
- constant tachycardia;
- tendency to lower blood pressure;
- dull heart sounds on auscultation.
In the advanced stage, due to compression of the esophagus, there are difficulties in swallowing, hiccups are disturbing.
If the pericardial cavity is full, then symptoms of incipient cardiac tamponade appear:
- weakness increases;
- the feeling of heaviness in the chest is constant and intensifying;
- shortness of breath at rest;
- the skin is covered with profuse cold sweat;
- the patient is excited, there is a fear of death;
- tachycardia intensifies, heart sounds are barely audible;
- a drop in blood pressure causes dizziness and fainting;
- breathing is shallow, frequency reaches 30 per minute.
Lack of treatment is accompanied by acute heart failure, cardiogenic shock, cardiac arrest and death.
Ascites: what is it and how to treat it
Contents ASCITS
REMOVAL OF ASCITES
FEARS AND MISCONCEPTIONS
There is always fluid present in the abdominal cavity of a healthy person. Normally it is no more than 150 ml. Up to 1.5 liters are produced per day, but it is absorbed and does not accumulate. However, with some diseases, the amount of fluid increases - it begins to be produced in excess, or it stops being absorbed.
Together with surgeon Alina Pribytkova, we understand what ascites is and how it is treated.
ASCITS
What is ascites?
Ascites is an accumulation of free fluid in the abdominal cavity. The reasons may be different: most often it is oncology, chronic heart failure, cirrhosis of the liver or kidney disease.
In oncology, the development of ascites most often provokes metastatic damage to the peritoneum, which causes excess fluid production and/or impairs its reabsorption.
There is another cause of ascites in cirrhosis. Normally, the liver synthesizes proteins that help retain fluid inside the vessel. When the liver is damaged, this function suffers, and fluid leaks through the walls of blood vessels more easily.
In chronic heart failure, blood stagnates in the systemic circulation, increased pressure occurs in the vessels and fluid from them leaks into the abdominal cavity. Also, with this pathology, sodium retention occurs in the body, which also contributes to the development of edema.
Kidney disease causes excessive excretion of proteins in the urine (proteinuria). The loss of protein leads to the fact that the liquid part of the blood is not retained in the vessels and leaks through their walls.
Important Ascites indicates deterioration and progression of the disease. In the early stages of the disease, fluid will not accumulate in the abdominal cavity. This happens only in the later stages of the disease, when the body's ability to compensate has been exhausted.
What types of ascites are there?
Ascites is divided into non-tense and tense.
Small or moderate ascites (non-tense) is a condition when fluid has already accumulated inside the abdominal cavity, but this is not enough to prescribe a procedure for removing ascites: there are no signs of tension, the abdominal wall is soft, pliable during palpation - “pressed”. In this case, surgical evacuation of fluid (laparocentesis) is not used due to the high risk of injuring internal organs, since with non-stressed ascites the distance between the internal organs and the anterior abdominal wall is not enough for manipulation due to the small layer of fluid between them.
With intense ascites, the abdomen becomes greatly enlarged, the skin is tightly stretched, shiny, and the navel may protrude, as during pregnancy. When palpating the anterior abdominal wall, great resistance is felt, which is created due to fluid pressure from the inside.
In quantitative terms, ascites becomes tense when fluid accumulates approximately over 7 liters, but all people are different: physique, parameters, body constitution, size of the abdominal cavity. Therefore, doctors do not focus on the volume of fluid: they perform an ultrasound of the abdominal cavity, examine and palpate the abdomen.
In a person with short stature and asthenic physique, ascites can be tense and with the accumulation of 5 liters of fluid. At the same time, in a tall person with a hypersthenic physique, 10 liters of free fluid may not give signs of tense ascites.
Webinar: Organizing therapeutic nutrition for a seriously ill patient How to organize therapeutic nutrition, what to prepare, what and where to feed, so that the food brings not only benefits, but also pleasure Workshop of CareOlga Kotelnikova
Care
Characteristic symptoms appear with tense ascites: a large belly with a protruding navel, like in pregnant women, a feeling of fullness in the abdomen and pressure on the stomach, nagging pain in the abdomen, shortness of breath, problems with eating due to the pressure of fluid on the stomach - belching, nausea or even vomiting, restriction of physical activity. The accumulation of fluid leads to increased intra-abdominal pressure and pushing of the diaphragm into the chest cavity. As a result, the respiratory movements of the lungs are significantly limited (up to the development of respiratory failure), the activity of the heart is disrupted, and the resistance to blood flow in the abdominal organs increases, the functions of which are also impaired. With long-term ascites, the outflow of lymph from the lower extremities and abdominal organs is disrupted, and swelling of the lower extremities occurs. People note a significant increase in general weakness.
Should we sound the alarm? When?
Ascites does not occur overnight; fluid accumulates gradually. A person may not even notice it and think that he is gaining weight. Usually, suspicions arise when specific symptoms occur: an enlarged abdomen, a feeling of fullness in the abdomen and pressure on the stomach, nagging pain in the abdomen, shortness of breath, belching, nausea or even vomiting, limitation of physical activity, swelling of the lower extremities, general weakness.
If a person notices signs of ascites, you need to see a doctor and do an ultrasound of the abdominal cavity: then the doctor will give recommendations and tell you whether the ascites needs to be removed surgically.
If a person is regularly observed by a doctor, then ascites can be detected during routine instrumental examinations (ultrasound, CT), during examination. If necessary, the doctor will prescribe additional examinations and give recommendations.
REMOVAL OF ASCITES
How is ascites removed?
To treat mild ascites, diuretics can be prescribed, which are most effective in cases of ascites resulting from chronic heart failure or cirrhosis of the liver. However, it should be remembered that there are refractory ascites, that is, resistant to diuretic therapy, when the use of medications does not have a positive effect. With prolonged, uncontrolled use of diuretics, the patient develops water and electrolyte disturbances, dehydration, and a drop in blood pressure. With ascites of an oncological nature, diuretics are most often ineffective.
For tense ascites, doctors perform laparocentesis: under local anesthesia, a puncture of the anterior abdominal wall is performed and the fluid is evacuated.
The frequency of the procedure depends on how quickly the fluid accumulates, on the existing pathology and the degree of its progression. For some, tense ascites may recur within a few months, for others within a week/month.
For ascites, the cause of which is chronic heart failure or cirrhosis of the liver, diuretics are also prescribed after surgical removal of the fluid, if the person’s condition allows.
How is the procedure done?
If there is a clinical picture of tense ascites, an ultrasound of the abdominal cavity is performed to assess the level of free fluid and determine the safest point for puncture of the anterior abdominal wall.
They talk with the person: they explain to him the principle of the planned manipulation, the possible risks, as with any invasive intervention. After which, if he agrees to the manipulation, the person signs an informed consent to the intervention. If a person is legally capable, he must sign the document himself; if not, then this is done by his official representative.
The area of the planned puncture of the anterior abdominal wall is treated with an antiseptic solution and then anesthetized layer by layer with a 5-10 ml syringe with a local anesthetic solution (lidocaine, novocaine - if the patient is allergic to these drugs, tell the doctor!). At the same time, the location of the needle is monitored - when it enters the abdominal cavity, ascitic fluid appears in the syringe.
Then, using a long hollow needle - or a special instrument - a stylet with a trocar, depending on the equipment chosen for the manipulation - the doctor pierces the anterior abdominal wall at a previously designated point and penetrates the abdominal cavity, receiving a flow of fluid through the needle. A plastic catheter is passed through the needle into the abdominal cavity, and the needle itself is removed. The plastic catheter is sutured to the skin to prevent it from moving or falling out. Through the catheter, the outflow of fluid goes into a vacuum bag attached to it (for better outflow, the bag should be below the level of the bed - on the floor or attached to the side of the bed).
The most favorable is fractional removal of fluid - 3-4 liters per day, as this will help avoid a sharp drop in pressure inside the abdominal cavity.
Skin care products for a sick person: how to choose? We help you understand the variety of foams, dry shampoos, creams and lotions for hygiene, including in special cases - with bedsores, an established stoma, urinary and fecal incontinence Evgeniya RezvanCar Care Workshop
Care
The drainage is in the abdominal cavity for several days, since it is fixed to the skin with a suture - you can turn, eat, move, the tube will not go anywhere. The puncture site must be treated with an antiseptic once a day and covered with an aseptic bandage. Usually, drainage does not cause pain; on the first evening after the puncture, there may be a slight pain in the area of the puncture of the abdominal wall, then, if there is no planned pain therapy, you can take a painkiller from the NSAID group (if there are no contraindications). But the drainage tube can touch the peritoneum, which lines the anterior abdominal wall from the inside and internal organs, and this in turn can cause discomfort.
After removing the ascites, the drainage from the abdominal cavity is removed. A suture may be placed over the punctured area to prevent any remaining fluid from leaking out. It is impossible to remove everything “dry”, since residual fluid remains in the pelvic cavity and between the intestinal loops, and its accumulation does not stop after laparocentesis. If a suture was not applied, then after a while the tissues “stick together” and the liquid stops leaking.
If a suture was placed after removing the drainage, then it must be treated with an antiseptic solution, the dressings should be changed once a day, healing usually occurs in 7-10 days. If a suture was not applied, the principle of care is the same, the difference is that in the first day or two after removal of the drainage, there may be a need to change the dressing more often due to slight leakage of fluid.
There are ascites that are difficult to evacuate: the liquid may have a gel-like nature, a heterogeneous structure, which can clog the drainage, or in rare cases, the liquid may not flow through the drainage at all due to its excessive viscosity. If the drain is blocked, the doctor will flush it with sterile saline to restore drainage.
Patient N., 56 years old. Diagnosis: Ovarian cancer, disease progression, peritoneal carcinomatosis, tense ascites. According to ultrasound, ascites is gel-like in nature, with a volume of about 10 liters. A decision was made to perform laparocentesis. As a result of the manipulation, practically no liquid flows through the installed plastic catheter due to an excessively thick jelly-like consistency that cannot be actively aspirated (that is, removed by attaching a syringe to the catheter). Next, a repeat laparocentesis was performed using a large-diameter trocar (hollow metal tube), with which it was possible to evacuate no more than 3 liters of secretion. The patient was recommended symptomatic therapy; further attempts to evacuate secretions are inappropriate due to the risk of complications.
The laparocentesis procedure is not very long, in typical cases it takes no more than 15-20 minutes. There are technically complex cases that require more time: if a person has excessively developed subcutaneous fat, there have been surgeries on the abdominal organs in the past, massive growth of metastases in the peritoneum, the presence of voluminous tumors in the abdominal cavity. In such cases, puncture can be performed directly under ultrasound guidance.
Is it possible to carry out the procedure at home? Can I go home immediately after the procedure?
Removal of ascites is a surgical intervention; it is not performed at home, like any other surgical operation: there is no necessary equipment, conditions, and sterility cannot be ensured.
It will also not be possible to go home with drainage, since it is a foreign body. It must be removed at a medical facility. At home, if the drainage is handled incorrectly, it can become dislodged/fall out, which can lead to infection. It is not recommended to remove ascites “in one day”; it is better to do it gradually, over several days, since the immediate removal of a large amount of fluid can provoke a sharp drop in pressure inside the abdominal cavity, which will entail a drop in a person’s systemic blood pressure and a deterioration in general well-being.
Are there any contraindications to the procedure? When can doctors refuse to perform a procedure?
The procedure is not performed when the ascites is not tense or is not tense enough, since in these cases internal organs can be damaged. With mild ascites, there are no painful symptoms, which is the reason to perform laparocentesis. It must be remembered that evacuation of fluid does not cure the disease, but only alleviates the painful manifestations that arise when there is a large accumulation of fluid.
Evacuation of fluid is not carried out if a person is in extremely serious condition, in other words, when the life prognosis is calculated in hours or days, and this means a complete depletion of the body’s compensatory forces. And the loss of protein, electrolytes, a decrease in intra-abdominal pressure with general hypotension (which is always present in the last days and hours of life) can only worsen the patient’s condition; after the manipulation he may not experience relief, and the stress of the intervention will add additional painful sensations to the already extremely serious condition. And we remember that the manipulation is invasive in nature, that is, like any surgical intervention, it can have a number of complications.
The procedure may be refused when a critical accumulation of fluid coincides with the transition to the terminal stage of the disease. Of course, the fluid can be evacuated: technically this is possible for almost any patient's condition, but the person's general condition will continue to get worse as the underlying disease progresses, and the fluid, even during the evacuation process, can quickly accumulate again. As mentioned above, it must be remembered that laparocentesis does not cure the disease, but only alleviates the painful manifestations that occur with a large accumulation of fluid, and it is necessary to compare the expected benefits of the manipulation and the existing risks of causing additional discomfort to the person at the end of life.
For example, according to abdominal ultrasound, the volume of ascites is 8 liters. The doctor puts in a drainage, but the fluid accumulates every day. A person gets 8 liters, 10 liters, 12 liters removed - so a week passes, and the drainage is still standing. He does not experience relief from the manipulation, and the drainage located in the abdominal cavity causes discomfort and complicates the care of the patient.
We already know that when ascitic fluid is removed, a person loses valuable substances - proteins and electrolytes. The protein concentration in serous ascitic fluid is usually relatively low, but with massive ascites, its total loss can be significant, especially with frequent repeated removal of large amounts of fluid, and the loss of protein is combined with the loss of salts, which leads to the development of severe protein and electrolyte deficiency.
Frequent laparocentesis or fractional pumping of fluid from the abdominal cavity over a long period of time will do more harm than good, so transition to the terminal stage of the disease is a contraindication to the procedure.
When it cannot be cured: 7 questions about palliative care Why palliative care is needed, whether it is necessary to register and what to do if a person or his relatives insist on continuing treatment Editorial Board "Vera" Foundation
About palliative care
Laparocentesis is not performed if:
- blood clotting is impaired (the risk of bleeding increases);
- decreased platelet levels (especially after chemotherapy);
- a pronounced adhesive process has been diagnosed (dense connective tissue (cords, adhesions) is formed in the abdominal cavity after inflammatory processes, injuries or surgical interventions, which “solder” the internal organs in the peritoneum, lining the anterior abdominal wall from the inside) - this is a risk of injury to the internal organs;
- peritoneal carcinomatosis was diagnosed, when the abdominal cavity is so affected by metastases that a safe area for puncture is not visualized, which is also fraught with injury or bleeding;
- a person has an unfavorable life prognosis (days, hours).
FEARS AND MISCONCEPTIONS
Is it possible to die from ascites or from the procedure for its removal?
Ascites, like the procedure for removing fluid from the abdominal cavity, cannot cause death. Ascites is not an independent disease, but usually acts as a symptom of one or another serious disorder in the body.
It should be remembered that with laparocentesis, as with any surgical intervention, even in the absence of contraindications, there is a low risk of complications.
Can ascites occur due to medications? Chemotherapy?
Drugs and chemotherapy cannot cause ascites.
Important: People with ascites are advised to evacuate it before chemotherapy to increase effectiveness.
To prevent fluid from accumulating, should you drink less water?
It is necessary to maintain a water-drinking regime, drink as needed. Refusal to drink can worsen the general condition and provoke the appearance of additional painful symptoms against the background of dehydration.
What happens if ascites is not removed?
Fluid in tense ascites does not mechanically damage internal organs, but can put pressure on the stomach, intestines, diaphragm, lymphatic system and disrupt their functions. This can cause breathing problems, constipation, nausea, vomiting, hiccups, belching, heartburn, loss of appetite, swelling of the lower extremities, even lymphorrhea (“sweating” of fluid through the skin). Against the background of the underlying disease, pain may intensify, and a feeling of tension and fullness in the abdominal cavity may appear.
It happens that with a very large accumulation of fluid in the abdominal cavity (20 liters or more), the pressure on the tissue is so high that the fluid begins to find “weak spots” in the abdominal wall and seep through them (scars after operations and even the navel).
Can internal organs be damaged during the procedure?
With mild ascites, there is a high probability of damaging internal organs, so in this case laparocentesis is contraindicated. If there is a significant amount of fluid and signs of tension, the risk of injury is minimal. Complications are possible with any operation, but with the correct indications and taking into account all contraindications, in the vast majority of cases laparocentesis occurs without complications or injuries.
Can drainage damage internal organs?
Changing the position and turning a bedridden patient Care specialist Olga Vygovskaya shows how to correctly turn a bedridden patient Olga Vygovskaya
Care
The drainage tube is soft, it will not damage the internal organs, but it can touch the peritoneum lining the anterior abdominal wall from the inside and internal organs, and this in turn can cause discomfort.
Is it possible to lie on your stomach with ascites? Is the blow dangerous?
Lying on the stomach for a person with tense ascites is extremely uncomfortable, but this is not prohibited. Most often, a person takes a position on his side. Any blows to the stomach in everyday life are also not dangerous: it is a liquid, it “flows around” the internal organs. Blows of excessive force are equally dangerous for internal organs, regardless of the presence of fluid in the abdominal cavity.
Are emergency operations performed for ascites?
If, for urgent reasons, a person with ascites suddenly finds himself on the operating table, this is not a contraindication to emergency surgery; surgeons simultaneously remove free fluid; all operating rooms are equipped with electric aspirators.
The material was prepared using a grant from the President of the Russian Federation provided by the Presidential Grants Foundation.
We would like to thank the volunteers of the Vera Hospice Fund for their assistance in preparing the material.
Stock image used from Depositphotos.
The occurrence of hydropericardium in the fetus
Ultrasound examination reveals fetal hydrocephalus. Accumulation of free fluid in the fetal pericardium indicates malformation or edema due to hemolytic disease.
The condition is dangerous for the baby and often occurs with congenital heart defects. The echo-negative bandwidth should be within normal limits.
If examination during pregnancy shows abnormalities in the development of the fetus, the woman should undergo a course of treatment and monitor the condition of the fetus until delivery.
Classification
This is done on two grounds. The first concerns the type of change that occurs.
Accordingly they talk about:
- Hydropericardium. Classic shape. There is a release of fluid into the sac surrounding the heart. Essentially, this is a serous transudate that comes out of the vessels and intercellular space for one reason or another. Which one you need to look at.
- Chylopericardium. Impaired lymph drainage. The main development factors are trauma, tumors, and inflammatory processes.
- Hemopericardium. It is not part of the structure of a typical hydropericardium, since it is not serous fluid that accumulates in the cavity, but blood. Some scientists combine all three pathological varieties in one classification.
The second criterion is the degree of severity. The basis for the distinction is the volume of output.
- First. No more than 100 ml in total. The pathological process is accompanied by minor symptoms. The clinical picture includes chest pain of moderate intensity, shortness of breath, and nausea. There may be pressing discomfort, a feeling as if a heavy stone had been placed.
- Second degree. 100-300 milliliters. Accompanied by severe clinical manifestations, breathing disorders, heart sounds, pallor, cyanosis. The patient takes a forced position, usually half-sitting due to increasing asphyxia and arrhythmia.
- Third degree. Over 300-400 ml. The risk of death is maximum, recovery in a hospital setting is urgent. Without help and surgical intervention, the patient will die.
Despite the indicated volumes, the pericardium can take up to several liters of fluid. All this time the patient is walking on the edge; at what point he breaks down is a matter of the body’s endurance. It's not worth testing.