Hypertensive crisis is a severe form of arterial hypertension. Can occur at any time. More often observed in women than in men. The cause of the occurrence lies in the disruption of blood pressure regulation. If arterial hypertension is common in 40% of the population, then in only 1% of cases there may be a sudden jump from baseline values, which leads to a sharp deterioration in health with a high risk of death.
What exactly are the symptoms of a hypertensive crisis should be known not only to hypertensive patients, but also to their loved ones. Normal and elevated blood pressure values are individual for each person. When a crisis occurs, signs of impaired cerebral or coronary blood supply are observed.
Symptoms and signs of their manifestation
When a hypertensive crisis occurs, the following symptoms appear:
- nausea, vomiting, suffocation;
- convulsions and loss of consciousness;
- intense headache;
- clouding of consciousness and disturbances in speech and vision;
- heart pain and palpitations;
- trembling, sweating, chills;
- feeling of lack of air;
- Possible loose stools.
Are you experiencing symptoms of a hypertensive crisis?
Only a doctor can accurately diagnose the disease. Don't delay your consultation - call
Types of pathology
Types of hypertensive crisis are classified depending on the manifestation of symptoms. Medical care is selected individually according to indications and clinical manifestations. Hypertensive crisis types I and II, complicated and uncomplicated forms are types of pathology. Hyperkinetic crisis or type I is characterized by rapid development. Acute headache and dizziness, nausea, and vomiting occur. The state is close to fainting. Blood pressure rises above 200 mm Hg. Art. (systolic - upper), which is why red spots appear in the face, neck, chest, feeling of heat, tachycardia, moist skin.
Hypokinetic crisis or type II occurs when there is a violation of the treatment regimen or rhythm of life in patients with stage III arterial hypertension. Deterioration in well-being develops more slowly, although the intensity remains noticeable. The severity of the headache increases exponentially. Diastolic (lower) pressure remains in the range of 140-160 mmHg. Art. Symptoms include nausea and vomiting, lethargy, blurred vision and hearing, and a tense pulse.
A complicated hypertensive crisis has several vectors of development, which affects the type of complications. There are such subtypes: coronary, asthmatic, cerebral. Against this background, pulmonary edema or cardiac asthma, acute left ventricular failure may develop. Cerebrovascular accidents, ischemic stroke and other pathologies may occur. An uncomplicated hypertensive crisis requires pressure correction in the next 24 hours, but it has an important nuance - there is no risk of target organ damage.
Nursing process in hypertension
Content
Introduction…………………………………………………………………………………3
1. Etiology……………………………………………………………………………….4
2. Clinic………………………………………………………………………………….5
3. Diagnostics………………………………………………………………………………..7
4. Treatment………………………………………………………………………………….8
5. Nursing process for hypertension……………………..9
Conclusion……………………………………………………………………………….15
Literature………………………………………………………………………………..16
Introduction
Arterial hypertension is an increase in blood pressure in the arteries as a result of increased heart function or increased peripheral resistance, or a combination of these factors. There are primary (essential) and secondary arterial hypertension.
Hypertension, or essential hypertension, is an increase in blood pressure not associated with organic damage to the organs and systems that regulate it. The development of hypertension is based on a violation of the complex mechanism that regulates blood pressure under physiological conditions.
According to a survey of a representative sample (1993), the age-standardized prevalence of hypertension (>140/90 mm Hg) in Russia is 39.2% among men and 41.1% among women. Women are better informed about the presence of the disease than men (58.9% versus 37.1%), are treated more often (46.7% versus 21.6%), including effectively (17.5% versus 5. 7%). In men and women, there is a clear increase in hypertension with age. Before 40 years of age, hypertension is more often observed in men, after 50 years - in women.
The development of hypertension can be divided into three parts:
central - a violation of the relationship between the processes of excitation and inhibition of the central nervous system;
increased production of pressor substances (norepinephrine, aldosterone, renin, angiotensin) and a decrease in depressor effects;
tonic contraction of arteries with a tendency to spasm and organ ischemia.
Etiology
Hereditary burden is the most proven risk factor and is well identified in relatives of the patient of close kinship (the presence of HD in mothers of patients is of particular importance). We are talking, in particular, about the polymorphism of the ACE gene, as well as the pathology of cell membranes. This factor does not necessarily lead to headache. Apparently, genetic predisposition is realized through the influence of external factors.
People with excess body weight have higher blood pressure. Epidemiological studies have convincingly shown a direct correlation between body weight and blood pressure. With excess body weight, the risk of developing hypertension increases 2-6 times (Quetelet index, which is the ratio of body weight to height, exceeds 25; waist circumference >85 cm in women and >98 cm in men). The factor of excess body weight is associated with a more frequent development of hypertension in industrialized countries.
Metabolic syndrome (syndrome X), characterized by a special type of obesity (android), insulin resistance, hyperinsulinemia, and lipid metabolism disorders (low levels of high-density lipoproteins - HDL - are positively correlated with increased blood pressure).
Alcohol consumption. SBP and DBP in persons who consume alcohol daily are 6.6 and 4.7 mmHg, respectively. higher than in people who drink alcohol only once a week.
Salt consumption. Many experimental, clinical and epidemiological studies have shown a connection between high blood pressure and daily consumption of table salt.
Physical activity. People living a sedentary lifestyle are 20-50% more likely to develop hypertension than physically active people.
Psychosocial stress. It has been established that acute stress load leads to an increase in blood pressure. It is assumed that long-term chronic stress also leads to the development of hypertension. The patient’s personality traits are probably also of great importance.
Clinic
The central symptom of hypertension is an increase in blood pressure, from 140/90 mm Hg. Art. and higher.
Main complaints: headaches, dizziness, blurred vision, pain in the heart, palpitations. Patients may have no complaints. The disease is characterized by an undulating course, when periods of deterioration are replaced by periods of relative well-being.
In the stage of functional disorders (stage I) there are complaints of headaches (usually at the end of the day), sometimes dizziness, and poor sleep. Blood pressure increases inconsistently, usually due to anxiety or fatigue (140-160/905-100 mm Hg).
In the second stage.
Complaints of constant headaches localized in the occipital region. Patients have poor sleep and dizziness. Blood pressure is persistently elevated. Attacks of pain in the heart appear.
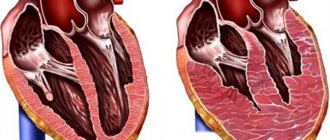
In stage 2 hypertension, the ECG shows signs of left ventricular hypertrophy and myocardial malnutrition.
In stage three hypertension, various organs are affected, primarily the brain, heart and kidneys. Blood pressure is persistently elevated (more than 200/110 mm Hg). Complications develop more often.
Hypertensive crisis
- a sudden increase in blood pressure, accompanied by disorders of the autonomic nervous system, increased disorders of the cerebral, coronary, and renal circulation and an increase in blood pressure to individually high numbers.
There are crises of types I and II.
Type I crisis occurs in stage I headache and is accompanied by neurovegetative symptoms.
Type II crisis occurs in stages II and III of headache.
Symptoms of a crisis:
severe headache, transient visual impairment, hearing impairment (stupefaction), heart pain, confusion, nausea, vomiting.
The crisis is complicated by myocardial infarction and stroke. Factors provoking the development of crises: psycho-emotional stress, physical activity, sudden withdrawal of antihypertensive drugs, use of contraceptives, hypoglycemia, menopause, etc.
The benign variant of the development of hypertension is characterized by slow progression, changes in organs are at the stage of stabilization of blood pressure. The treatment is effective. Complications develop only in the later stages. For definitions of risk levels, see the table.
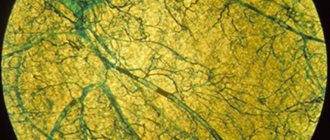
The malignant variant of hypertension is characterized by a rapid course, high blood pressure, especially diastolic, rapid development of renal failure and brain disorders. Changes in the fundus arteries with foci of necrosis around the optic nerve nipple and blindness appear quite early. The malignant form of hypertension can be fatal if left untreated.
Diagnostics
Diagnosis of hypertension and examination of patients with hypertension is carried out in strict sequence, meeting certain objectives:
— determination of the stability of the increase in blood pressure and its degree;
- exclusion of symptomatic hypertension or identification of its form;
— identifying the presence of other risk factors for cardiovascular diseases and clinical conditions that may affect prognosis and treatment, as well as classifying the patient to a particular risk group;
— determination of the presence of lesions of “target organs” and assessment of their severity.
According to the 1999 WHO-ITF international criteria, hypertension is defined as a condition in which blood pressure is 140 mmHg. Art. or higher and/or ADD - 90 mm. rt. Art. or higher in individuals not receiving antihypertensive therapy.
Headache is divided into primary, when headache and associated symptoms form the core of the clinical picture and are combined into an independent nosological form (migraine, tension headache, cluster headache), and secondary, when it becomes a consequence of obvious or masked pathological processes.
Among primary headaches, the most common forms are tension-type headache (TTH) and migraine (M).
In a patient with newly diagnosed hypertension, a careful history must be taken, which should include: - the duration of hypertension and levels of elevated blood pressure in the history, as well as the results of previously used antihypertensive treatment, a history of hypertensive crises.
Additional examination:
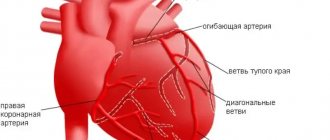
OAK—increase in red blood cells, hemoglobin. BAC—hyperlipidemia (due to atherosclerosis). OAM—proteinuria, cylindruria (with chronic renal failure). Zimnitsky test - isohyposthenuria (with chronic renal failure). ECG - signs of left ventricular hypertrophy. Ultrasound of the heart - enlargement of the wall of the left ventricle. Examination of the fundus - narrowing of the arteries, dilatation of the veins, hemorrhages, swelling of the optic nerve nipple.
Treatment
Treatment of stage I headache is usually carried out using non-drug methods, which can be used at any stage of the disease. A hyposodium diet is used, body weight is normalized (fasting diets), limiting alcohol intake, quitting smoking, constant physical activity, acupuncture, rational psychotherapy, acupuncture, physiotherapeutic treatment, herbal medicine.
If there is no effect from non-drug treatment within 6 months, drug treatment is used, which is prescribed in stages (starting with one drug, and if ineffective, a combination of drugs).
In patients with stages I and II, the leading role in treatment belongs to systematic drug therapy, which should be comprehensive. At the same time, it is necessary to systematically carry out preventive measures, among which physical education occupied a significant place.
Long-term antihypertensive therapy with individual maintenance doses is required. In elderly patients, blood pressure decreases gradually, since a rapid decrease worsens cerebral and coronary circulation. Blood pressure should be reduced to 140/90 mmHg. or to values lower than the original ones by 15%. Treatment should not be abruptly stopped; treatment should begin with known medications.
Of the many groups of antihypertensive drugs, 4 groups have received practical use: β-blockers (propranolol, atenolol), diuretics (hypothiazide, indapamide, uregit, veroshpiron, arifon), calcium antagonists (nifedipine, adalat, verapamil, amlodipine) ACE inhibitors (captopril , enalapril, sandopril, etc.).
Nursing process in hypertension
Lifestyle changes are recommended for all patients, including those receiving drug therapy, especially in the presence of certain risk factors. They allow:
lower blood pressure; reduce the need for antihypertensive drugs and maximize their effectiveness; favorably influence other existing risk factors; carry out primary prevention of hypertension and reduce the risk of concomitant cardiovascular disorders at the population level.
Non-drug methods include:
- to give up smoking; — reduction and/or normalization of body weight (achieving a BMI < 25 kg/m2); - reducing the consumption of alcoholic beverages to less than 30 g of alcohol per day in men and less than 20 g per day in women; - increase in physical activity (regular aerobic (dynamic) physical activity for 30-40 minutes at least 4 times a week); — reducing the consumption of table salt to 5 g/day;
- a comprehensive change in diet (increasing the consumption of plant foods, reducing the consumption of saturated fats, increasing the diet of potassium, calcium contained in vegetables, fruits, grains, and magnesium contained in dairy products).
The target blood pressure level is a blood pressure level of less than 140 and 90 mm Hg. In patients with diabetes, it is necessary to reduce blood pressure below 130/85 mm Hg. Art., with chronic renal failure with proteinuria more than 1 g/day below 125/75 mm Hg. Achievement of target blood pressure should be gradual and well tolerated by the patient. The higher the absolute risk, the more important it is to achieve the target blood pressure level. With regard to concomitant hypertension and other associated risk factors, it is also recommended to achieve their effective control, and, if possible, normalize the corresponding indicators (Table 5. Target values of risk factors).
Achieving and maintaining target blood pressure levels requires long-term monitoring with monitoring of compliance with recommendations for lifestyle changes, regularity of antihypertensive therapy and its correction depending on the effectiveness and tolerability of treatment. During dynamic observation, it is crucial to achieve individual contact between the patient and the nurse, and a patient education system that increases the patient’s sensitivity to treatment.
In a hospital setting, the entire rehabilitation process is based on three motor modes: bed: strict, extended; ward (semi-bed); free.
During extended bed rest, the following tasks are solved: improving the neuropsychic status of the patient; gradual increase in the body’s adaptation to physical activity; decreased vascular tone; activation of the function of the cardiovascular system by training intra- and extracardiac circulatory factors.
At the stage of ward (semi-bed) rest, the following tasks are solved: eliminating the patient’s mental depression; improving adaptation of the cardiovascular system to increasing loads through strictly dosed training; improvement of peripheral blood circulation, elimination of congestion; training in proper breathing and mental self-regulation.
During the free regime, the tasks of improving the functional state of the central nervous system and its regulatory mechanisms are solved; increasing the overall tone of the body, the adaptability of the cardiovascular and respiratory systems and the whole body to various physical activities; strengthening the myocardium; improving metabolic processes in the body.
This motor mode in a hospital setting is characterized by the greatest motor activity. The patient is allowed to walk freely around the department; it is recommended to walk up the stairs (within three floors) with pauses for rest and breathing exercises
In hypertensive crisis
Lasix IV, nitroglycerin, clonidine or Corinfar, nifedipine - 1 table are used. under the tongue. If there is no effect - intravenous aminophylline, intravenous labetolol. Parenteral treatment is prescribed by a doctor.
It should be remembered that blood pressure must be reduced slowly, over 1 hour; with a rapid decrease, acute cardiovascular failure can develop, especially in the elderly. Therefore, after 60 years, antihypertensive drugs are administered only intramuscularly.
Treatment of hypertension is carried out for a long time and antihypertensive drugs are discontinued only when blood pressure stabilizes to the desired level over time (the doctor decides to cancel).
Stage I – nursing examination based on objective and subjective complaints
sick
Stage II Stage III Stage IV Stage V
| Patient problems | Goals | Nursing interventions | Evaluating the effectiveness joint venture (produced upon expiration of the delivery period) no purpose | ||
| k/s | d/s | plan | motivation | ||
| Main: - increased blood pressure | Achieve a gradual decrease in blood pressure by the end of the first day | Achieve stabilization of blood pressure indicators by day 10 (at discharge) | 1. Ensure physical and psychological rest 2. Place the patient or transfer him to a horizontal position with the head end raised 3. Provide access to fresh air 4. Place mustard plaster on the area. back of the head and calf muscles 5. Monitor the patient’s condition, measure blood pressure every 30 minutes until blood pressure normalizes 6. Follow all doctor’s orders: monitor regular intake of antihypertensive drugs 7. Train the patient in measuring blood pressure | For the effectiveness of treatment In order to reduce blood flow to the goal. brain and heart For enriched. air with oxygen To reduce blood pressure For timely. providing emergency assistance in case of emergency. complications | By the end of the first day, blood pressure was reduced - the goal was achieved. By the 10th day, blood pressure remained at a stable level - the goal was achieved. |
| - headaches, dizziness, tinnitus | The patient will note a decrease in goals. pain and dizziness by the end of the 3rd day | The patient will not complain about the goal. pain and dizziness - dizziness at the time of discharge | 1. Ensure physical and mental rest 2. Ensure medication intake. Medicines prescribed by a doctor. 3. If dizziness occurs, accompany the patient. 4. Ensure frequent ventilation of the rooms. | By day 3, the patient has no headaches - the goal has been achieved. At the time of discharge, the patient does not complain of headaches - the goal has been achieved. | |
| Comorbidities: sleep disturbance | Within 7 days the patient will be able to fall asleep and sleep without awakening for 4-6 hours, if necessary with the help of sleeping pills | By the time of discharge from the hospital, the patient will be able to sleep from 6 to 7 hours continuously without taking sleeping pills | 1. Observe the patient’s sleep and assess sleep disturbances. 2. Distract the patient from sleep during the day (which promotes night sleep) 3. Ensure that all types of food and drinks containing caffeine are excluded from the patient’s diet, including tea and coffee. 4. Take measures to help the patient fall asleep, e.g.: rubbing the back, warm baths, airing the room before bed, warm non-stimulating drinks (milk), quiet music, relaxation exercises. 5. Set a certain time for going to bed and do not violate this schedule. 6. Assure the patient that if he needs anything, he will get the help he needs. 7. As prescribed by the doctor, give the patient sleeping pills | For the first 5 days the patient slept with the help of sleeping pills, from the 6th day he began to fall asleep without them - the goal was achieved. | |
| - vomit | Reduce the severity of vomiting by the end of 3 days | Vomiting will not bother the patient | 1. Provide the patient with everything necessary (basin, tray) for vomit, towel, mouthwash, if necessary 2. Avoid dehydration (give drink) 3. Create physical and mental peace, eliminate bright light, noise. 4. Give antiemetics as prescribed by the doctor. | On the 2nd day the patient no longer complains of vomiting - the goal has been achieved | |
| - irritability, anxiety | Reduce the patient's irritability and anxiety within 6 days | The patient will not be irritable upon discharge | 1. Create a calm environment. 2. Talk with the patient more often on various topics. 3. Instill confidence in a favorable outcome of the disease 4. Ensure the use of sedatives (such as valerian, motherwort) as prescribed by the doctor 5. Teach the patient relaxation methods. | By day 6, the patient became less irritable, the anxious state does not bother the patient - the goal has been achieved. | |
| Potential - the possibility of developing complications; — ineffectiveness of taking antihypertensive drugs. | Prevent the development of complications and progression of the disease | 1. Conduct conversations: A) about the importance of observing work, rest, diet - with limited salt and liquid. B) about the effect of smoking and drinking alcohol on increasing blood pressure C) about the importance of systematically taking antihypertensive drugs and periodically visiting a doctor. | |||
Conclusion
Hypertension is a chronic disease that affects various systems of the body, characterized by an increase in blood pressure above normal, the most common disease of the cardiovascular system.
It has been established that those suffering from hypertension account for 15 - 20% of the adult population according to various epidemiological studies. HD quite often leads to disability and death. The underlying cause of the disease is arterial hypertension.
Arterial hypertension is one of the main risk factors for the development of coronary artery disease, cerebral stroke and other diseases.
Primary prevention of hypertension is the prevention of etiological risk factors.
Secondary prevention is medical examination of patients with hypertension. Patients are examined and examined at least once a year.
The main goal of treating a patient with hypertension is to achieve the maximum degree of reduction in the overall risk of cardiovascular morbidity and mortality. This involves addressing all identified reversible risk factors, such as smoking, high cholesterol and diabetes, appropriate treatment of associated diseases, as well as correction of high blood pressure itself.
The target blood pressure level is a blood pressure level of less than 140 and 90 mm Hg. In patients with diabetes, it is necessary to reduce blood pressure below 130/85 mm Hg. Art., with chronic renal failure with proteinuria more than 1 g/day below 125/75 mm Hg. Achievement of target blood pressure should be gradual and well tolerated by the patient.
Literature
1. Gogin E.E. “Hypertension” - M, 1997 – 62 p.
2. Roytberg G. E. Strutynsky A. V. Internal diseases. Cardiovascular system, M, 2002 – 123 p.
3. Smoleva E.V. Nursing in therapy. – Rostov n/a: Phoenix, 2007 – 169 p.
4. Tulyankin V.F. Tulyankina T.I. Home Doctor. JSC "Paritet", 2002-248p.
Preventive measures
The best prevention of a hypertensive crisis is awareness of the peculiarities of the occurrence of attacks, an understanding of how an increase in blood pressure occurs and the causes of this phenomenon.
Timely diagnosis and interaction with a doctor, following medical recommendations is an opportunity to prevent the development of crises of varying degrees. Hypertension can be controlled if:
- avoid drinking alcohol;
- stop smoking;
- reduce salt intake to 5 g per day;
- normalize body weight;
- adhere to antihypertensive therapy;
- reduce stress levels;
- avoid overwork.
Information about the diagnosis and treatment of patients
Regardless of the causes of a hypertensive crisis in a man or woman, diagnosis comes first to determine the further course of treatment. Symptoms may coincide with other pathological conditions. Diagnosis of hypertensive crisis includes the following procedures and studies:
- Analysis of urine;
- ECG, CT, radiography;
- heart rate measurement.
The doctor needs to collect a detailed history of the patient's condition. When the attacks began, the frequency of their occurrence, symptoms, whether the patient receives regular antihypertensive therapy, what methods were used to reduce blood pressure, whether there was experience in independently stopping the crisis, the presence of concomitant diseases - basic information for the doctor during the diagnosis.
Treatment and its features
Treatment for a hypertensive crisis is prescribed depending on the medical history and the presence of other conditions in acute form or chronic pathologies (cardiac percussion, auscultation of the heart, lungs, large vessels, hemorrhagic stroke, renal failure, severe myocardial ischemia). At the time of the attack, the patient needs medical attention. It consists of lowering blood pressure.
Afterwards, drug therapy is prescribed. When prescribing drugs, it is important that they act after a maximum of 20-30 minutes, and the effect lasts for at least 4-6 hours. When treating crises, the danger is the occurrence of uncontrollable hypotension. For this reason, self-medication with such a diagnosis carries the risk of drug collapse. Special medical supervision is necessary for patients with a history of concomitant diseases. It is important to understand that with proper treatment of arterial hypertension, crises occur extremely rarely.
Hypertension: risk factors, treatment and prevention methods
Gilmanshina Diana Ralifovna
Cardiologist, general practitioner
Hypertension
is a pathology of the cardiovascular system, developing as a result of dysfunction of higher centers of vascular regulation, neurohumoral and renal mechanisms and leading to arterial hypertension, functional and organic changes in the heart, central nervous system and kidneys.
Arterial hypertension (AH)
– stable increase in systolic pressure more than 140 mmHg. Art. or diastolic more than 90 mm Hg. Art.
According to research, arterial hypertension is one of the most common chronic diseases. Hypertension is the most common chronic disease in the practice of general practitioners and cardiologists.
Arterial hypertension occurs in approximately one third of the population of most developed and developing countries. According to recent epidemiological studies in Russia, about 48% of men and 40% of women have arterial hypertension.
Risk factors for hypertension.
They can be conditionally divided into irremovable and removable.
Unavoidable risk factors for hypertension:
• Age (the incidence of the disease is more common after 45 years).
• Gender (men are more susceptible to hypertension).
• Genetic predisposition, heredity (if one of the parents had the disease, the probability is 50–60%, if both parents were sick, the probability is almost 100%).
Avoidable risk factors:
• Overweight and obesity (if the waist circumference in men is 102 cm or more, and in women – 88 cm or more). It is known that for every 10 kg of excess weight, systolic (upper) blood pressure increases by 2-3 mmHg, and diastolic (lower) - by 1-3 mmHg.
• Smoking.
• Nutritional factors.
• Poor nutrition (excessive consumption of table salt, overeating, excessive consumption of animal fats, lack of dairy products, vegetables and fruits).
• Abuse of alcohol and coffee.
• Chronic stress.
• Physical inactivity – sedentary lifestyle (risk increases by 20 – 50%).
• Presence of concomitant diseases (diabetes mellitus, kidney pathology and atherosclerosis).
You need to know that arterial hypertension ranks first in its contribution to mortality from cardiovascular diseases (CVD). Most often, patients die from its complications. The relationship between blood pressure (BP) and CVD risk is continuous, constant and independent of other risk factors.
With a long-term or malignant course of hypertension, chronic damage to the blood vessels of target organs develops: the brain, kidneys, heart, eyes.
Instability of blood circulation in these organs against the background of persistently elevated blood pressure can cause the development of:
• angina pectoris, • myocardial infarction, • hemorrhagic or ischemic stroke, • cardiac asthma, pulmonary edema, • dissecting aortic aneurysm, • retinal detachment, etc.
The development of acute emergency conditions against the background of hypertension requires a decrease in blood pressure in the first minutes and hours, as it can lead to the death of the patient.
The course of hypertension is often complicated by hypertensive crises - periodic short-term increases in blood pressure. The development of crises may be preceded by emotional or physical overstrain, stress, changes in meteorological conditions, etc. In a hypertensive crisis, there is a sudden rise in blood pressure, which can last several hours or days and is accompanied by dizziness, severe headaches, a feeling of heat, increased heartbeat, vomiting, cardialgia (pain in the heart area), visual impairment. During a hypertensive crisis, patients are frightened, excited or inhibited, and drowsy; in severe cases they may lose consciousness.
Against the background of a hypertensive crisis and existing organic changes in blood vessels, myocardial infarction, acute cerebrovascular accidents, and acute left ventricular failure can often occur.
Hypertension is classified according to a number of characteristics:
reasons for the rise in blood pressure, damage to target organs (brain, blood vessels, heart, kidneys), by blood pressure level, by course, etc.
According to the etiological principle, they distinguish:
- essential (primary) - secondary (symptomatic, i.e. against the background of other diseases) arterial hypertension
Depending on the level there are:
• Optimal blood pressure is < 120/80 mm Hg. Art. • Normal blood pressure - 120-129 /84 mm Hg. Art. • Borderline normal blood pressure - 130-139/85-89 mm Hg. Art. • Arterial hypertension of the 1st degree - 140-159/90-99 mm Hg. Art. • Arterial hypertension II degree - 160-179/100-109 mm Hg. Art. • Stage III arterial hypertension - more than 180/110 mm Hg. Art.
Treatment.
When treating hypertension, it is important not only to lower blood pressure, but also to correct and reduce the risk of complications as much as possible. It is impossible to completely cure hypertension, but it is quite possible to stop its development and reduce the frequency of crises.
Hypertension requires the combined efforts of the patient and the doctor to achieve a common goal.
At any stage of hypertension it is necessary:
• Follow a diet with increased consumption of potassium and magnesium, limiting the consumption of table salt;
• Stop or sharply limit alcohol intake and smoking;
• Get rid of excess weight;
• Increase physical activity: it is useful to engage in swimming, physical therapy, and walking;
• Take prescribed medications systematically and for a long time under the control of blood pressure and dynamic supervision of a cardiologist.
The criteria for the effectiveness of treatment of hypertension is the achievement of:
•
short-term goals:
maximum reduction in blood pressure to a level of good tolerance;
• medium-term goals:
preventing the development or progression of changes in target organs;
• long term goals:
prevention of cardiovascular and other complications and prolongation of the patient’s life.
Cardiologist, Candidate of Medical Sciences Diana Ralifovna Gilmanshina.
Answers to frequently asked questions from patients
How long does a hypertensive crisis last?
On average, an attack lasts about 2-3 hours. Symptoms develop either quickly or progressively, depending on the form of the crisis.
What should not be done during a hypertensive crisis?
You cannot endure and wait for the crisis to pass. It is necessary to carry out first aid measures that involve a gradual decrease in blood pressure. During an attack, the patient should not stand, stand up sharply, bend over, push, or take physical action. When blood pressure decreases, the patient can rest in a horizontal position, but with the head of the bed raised.
What is the hidden danger of a hypertensive crisis?
The consequences of a hypertensive crisis are widespread - stroke, myocardial infarction, disorders of the central nervous system, angina pectoris, and aneurysm. For this reason, hypertension should be monitored by a doctor, and the patient should take antihypertensive drugs regularly.
Publications in the media
Hypertensive crisis is a sudden increase in systolic and/or diastolic blood pressure, accompanied by signs of deterioration of cerebral, coronary or renal circulation, as well as severe autonomic symptoms. A hypertensive crisis, as a rule, develops in untreated patients with abrupt cessation of antihypertensive drugs, and may also be the first manifestation of hypertension or symptomatic arterial hypertension in patients who do not receive adequate treatment. Statistical data. 1% of patients with arterial hypertension.
Clinical manifestations • Clinically, a hypertensive crisis is manifested by an increase in blood pressure, may be accompanied by the occurrence of: •• acute hypertensive encephalopathy •• subarachnoid hemorrhage •• stroke •• MI •• acute left ventricular failure in the form of pulmonary edema •• aortic dissection •• acute renal failure • In hypertensive crisis of patients may be disturbed by severe headache, severe dizziness, visual impairment in the form of decreased acuity and loss of visual fields, chest pain (due to myocardial ischemia, aortalgia), palpitations, shortness of breath • When examining the patient, signs of target organ damage should be identified: •• changes fundus (narrowing of arterioles, hemorrhages, exudates, swelling of the optic nerve nipple) •• dysfunction of the left ventricle (tachycardia, “gallop rhythm”, pulmonary edema, dilatation of the veins of the neck) •• cerebral circulation disorders (neurological signs).
Additional examination. In a clinical setting, in addition to measuring blood pressure, it is necessary to conduct a chest x-ray, ECG, fundus examination, blood and urine tests. If possible, blood pressure monitoring is recommended (preferably intra-arterial).
TREATMENT
General tactics • Intensive therapy • Bed rest • Favorable psychological environment • Diets No. 10, 10a • Intensive therapy with intravenous administration of antihypertensive drugs against the background of constant blood pressure monitoring (optimally - using an arterial catheter) • After normalization of blood pressure - selection of antihypertensive drugs for systematic use • From a clinical point of view, it is advisable to distinguish emergency conditions when it is necessary to reduce high blood pressure within 1 hour, and conditions when it is possible to reduce high blood pressure within several hours (a decrease in mean blood pressure by approximately 20-25% of the initial or diastolic within 1 hour Blood pressure up to 100–110 mm Hg) • Conditions in which it is necessary to reduce blood pressure within 1 hour •• Aortic dissection (dissecting aortic aneurysm) •• Acute heart failure •• MI •• Unstable angina •• Severe nosebleeds • • Encephalopathy •• Intracranial hemorrhage •• Subarachnoid hemorrhage •• Skull trauma •• Eclampsia •• Catecholamine crisis in pheochromocytoma •• Postoperative bleeding from the area of vascular sutures • Conditions in which blood pressure can be reduced within several hours (12–24 hours) • • Systolic blood pressure 240 mm Hg. and/or diastolic blood pressure 130 mm Hg. and more without complications •• Malignant arterial hypertension without complications •• Arterial hypertension in the pre- and postoperative period •• Severe withdrawal syndrome of antihypertensive drugs •• Severe burns •• Renal crisis in scleroderma
Drug therapy • Drugs for relief of hypertensive crisis •• Sodium nitroprusside 0.25–10 mcg/kg/min intravenously, onset of action is immediate, duration of action is 1–2 min •• Nitroglycerin 5–100 mcg/min i.v. by drip, onset of action - 2-5 minutes, duration of action - 3-5 minutes •• Enalapril 1.25-5 mg IV, onset of action - 15-30 minutes, duration of action - 6 hours •• Esmolol 250-500 mcg/kg/min over 1 min, then 50–100 mcg/kg/min over 4 min, onset of action 1–2 min, duration of action 10–20 min •• Phentolamine 5–15 mg IV bolus, onset action - 1-2 minutes, duration of action - 3-10 minutes •• Bendazole 50-70 mg IV bolus, onset of action - 10-15 minutes, duration of action - 1 hour or more •• Clonidine 0.075-0.150 mg IV c slowly, onset of action - 10-20 minutes, duration of action - 4-8 hours •• Captopril 6.25-50 mg orally, onset of action - 15 minutes, duration of action - 6-8 hours •• Furosemide 20-120 mg c /in bolus, onset of action - 5 minutes, duration of action - 2 hours • Recommendations for the treatment of conditions requiring a decrease in blood pressure within 1 hour •• Hypertensive encephalopathy: sodium nitroprusside •• Subarachnoid hemorrhage: nimodipine, sodium nitroprusside •• Ischemic stroke: nitroprusside sodium •• MI: nitroglycerin, sodium nitroprusside •• Acute left ventricular failure: sodium nitroprusside, nitroglycerin •• Aortic dissection: b-blockers, sodium nitroprusside •• AKI: sodium nitroprusside •• Eclampsia: magnesium sulfate, hydralazine, slow calcium channel blockers • • Hyperadrenergic conditions (pheochromocytoma, clonidine withdrawal, cocaine use, amphetamines): phentolamine, sodium nitroprusside, clonidine (with clonidine withdrawal syndrome) •• Hypertensive crisis in the postoperative period: nitroglycerin, sodium nitroprusside
Features of reducing blood pressure in various conditions • In case of cerebrovascular accidents, mean blood pressure should be reduced by no more than 20–25% of the initial level or diastolic blood pressure should not be lower than 105–110 mm Hg. It is recommended to maintain this level of blood pressure for several days from the moment it increases. • In older people, even small doses of antihypertensive drugs when taken orally can significantly reduce blood pressure and lead to arterial hypotension.
Course and prognosis. With adequate therapy, the prognosis is favorable. In severe cases, the crisis is complicated by coma, pulmonary edema, stroke, thrombosis and embolism of various arteries, acute renal failure. A sharp decrease in blood pressure can lead to acute disruption of cerebral and coronary circulation.