The myocardium is a muscle that controls the contractions of the heart and regulates blood supply to the entire body. For uninterrupted operation, it needs regular nutrition and oxygen, supplied through the coronary arteries.
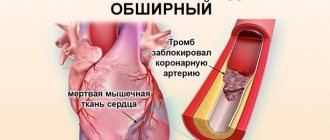
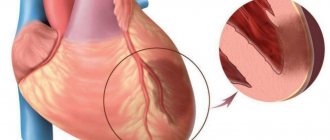
If for some reason the breathing and nutrition of the myocardium are disrupted, muscle cells begin to die. Necrosis of one or another part of the heart muscle is called myocardial infarction .
Myocardial infarction often entails complete or partial disability, and this is not the worst thing. In 10-12% of cases it threatens the patient’s very life!
17.5 million - according to statistics, this is how many people die every year in the world from heart and vascular diseases. And by 2030, according to WHO experts, this figure will reach even more terrible figures - 23.6 million deaths from CVDs per year.
Causes of myocardial infarction
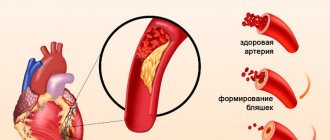
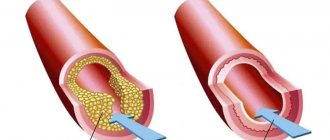
In most cases, necrosis of myocardial tissue occurs due to thrombosis of the coronary artery, which is provoked by atherosclerosis - atherosclerotic plaques clog the artery, disrupting the blood supply.
Other common causes of heart attack are coronary vasospasm and coronary thrombosis.
1 Ultrasound of the heart during a heart attack
2 Diagnosis of heart attack
3 Diagnosis when there is a threat of a heart attack
Drug therapy
When administering drug therapy to extensive myocardial infarction, it is important to comply with the following conditions:
- prolonged bed rest;
- complete psycho-emotional calm;
- special food;
- constant monitoring of the functioning of absolutely all body systems.
If detected in time, infarction of the posterior wall of the heart can be cured. The attending doctor establishes a list of necessary medications aimed at preventing the symptoms of myocardial rupture and normalizing the well-being of the patient and his blood vessels:
- antiplatelet therapy - special substances to thin blood clots and improve blood flow (acetylsalicylic acid); anesthesia (Nitroglycerin);
- relief from arrhythmia (Cordarone, Lidocaine);
- prevention of blood clot formation (anticoagulants - Polysaccharide, Lovenox, Heparin, as well as antiplatelet agents - Lyoton, Plavix);
- means that dissolve blood clots in the body (thrombolytic drugs - Fibrinolysin, Alteplase).
Who is at risk of myocardial infarction
Risk factors are:
- hypertonic disease;
- previous heart attack;
- smoking;
- sedentary lifestyle;
- hereditary predisposition;
- increased levels of “bad” cholesterol in the blood;
- obesity;
- diabetes;
- elderly age;
- postmenopausal state (in women);
- regular stress;
- excessive stress (physical and emotional);
- bleeding disorders.
Surgical methods of treatment
If an extensive myocardial infarction does not respond to drug therapy, the doctor decides in favor of the following operations:
- angioplasty of coronary vessels with stenting, which involves installing a stent in the artery to maintain the natural lumen in it;
- coronary bypass surgery. A complex surgical intervention in which the surgeon creates a bridge from an intact vein, providing natural blood flow above the narrowing.
There are cases when surgical intervention does not give positive dynamics and the lesion continues to increase in size. This situation involves a heart transplant.
Types of myocardial infarction
Since areas of muscle tissue of different sizes can undergo necrosis, cardiologists distinguish between small-focal and large-focal myocardial infarction.
Also, heart attacks are divided, depending on the depth of damage to the heart wall, into:
- transmural - pathological changes cover the entire thickness of the muscle layer;
- intramural - necrosis lies deep in the heart muscle;
- subepicardial - areas of the myocardium close to the epicardium are affected;
- subendocardial - the necrotic process is concentrated in the area of contact between the myocardium and the endocardium.
Depending on the location of the lesion, there are 2 types of myocardial infarction:
- right ventricular;
- left ventricular.
Based on clinical manifestations, cardiologists distinguish between typical and atypical myocardial infarction.
1 ECG for heart attack
2 IVF-KG for heart attack
3 Blood test for markers of heart attack
Nosological features of myocardial damage: review of the symposium
Summary. The main topic of the symposium was “Nosological features of myocardial damage: how to recognize and what to do?” became cardioprotective therapy and the use of safe and highly effective metabolically active drugs for energy support of the myocardium.
On April 22-24, 2021, with the support of the European Society of Cardiology, the VIII International Educational Forum “Russian Heart Days” was held. As part of one of the most significant events for the cardiology community, leading specialists from Russia and Europe discussed the most pressing problems of cardiology in offline and online formats, including the difficulties of using common therapeutic and surgical treatment tactics and the features of introducing innovative methods of treating cardiovascular diseases.
The symposium “Nosological features of myocardial damage: how to recognize and what to do?”, held on the first day of the Forum with the support of , was devoted to cardiometabolic disorders and the possibilities of pharmacological support of the heart muscle for the purpose of primary and secondary prevention of cardiovascular diseases (CVD) with various comorbid pathologies .
| Sergey Anatolyevich BONDAREV , Doctor of Medical Sciences, Professor of the Department of Sports Medicine and Rehabilitation of the First Moscow State Medical University named after. I. M. Sechenov Ministry of Health of Russia |
The first speaker, Sergey Anatolyevich Bondarev, Doctor of Medical Sciences, Professor of the Department of Sports Medicine and Rehabilitation of the First Moscow State Medical University named after. I.M. Sechenov Ministry of Health of Russia , dedicated his lecture to the topic “Excess or necessity? Correction of myocardial metabolism in cardiac rehabilitation after COVID-19.”
Sergei Anatolyevich drew the attention of his colleagues to the fact that despite the fact that in recent weeks the number of people infected with the new coronavirus infection has been decreasing, the problem remains acute. It is now known that large enveloped non-segmented positive-sense RNA viruses, such as SARS-CoV-2, can lead not only to severe pneumonia, but also to distress and cardiac damage. SARS-CoV-2 enters human cells through the angiotensin-converting enzyme receptor (ACE2), causing an abundance and diversity of cardiovascular manifestations.
Myocardial damage during COVID-19 is caused directly by blockade and damage to ACE2 receptors in the endothelium of the coronary arteries, which lead to an acceleration of the onset and development of CVD. In addition, the pathological process is aggravated by hypoxemia caused by viral infection, hypoxia provoking inflammatory reactions, as well as acidosis and the formation of oxygen free radicals during hypoxia and reperfusion.
To date, more than 2/3 of patients with COVID-19 require pulmonary, cardiovascular and psychological rehabilitation. Due to the relevance of the problem and the peculiarities of the pathogenesis of myocardial damage during coronavirus infection, cardioprotective therapy for such patients is attracting increasing attention from cardiologists. The range of possibilities of cardioprotective therapy includes replenishing energy costs, stabilizing cell membranes, restoring cell protein structures, and providing an antioxidant effect.
A number of drugs have such properties, including meldonium, trimetazidine, vitamins B and C. However, meldonium and trimetazidine, having the effect of stimulating the formation of ATP, require an initial expenditure of energy for the transport of fatty acids in order to block entry into the cell or accumulation. In this regard, the use of phosphocreatinine sodium salt (Neoton) in the complex therapy of myocarditis and/or myocardial damage associated with viral infection is of particular interest. Domestic guidelines for 2021 on anesthesiological and resuscitation care for patients with the new coronavirus infection COVID-19, as well as foreign guidelines, prescribe the prescription of phosphocreatinine at the rate of 1 g twice a day for 7-10 days. Phosphocreatinine sodium salt improves microcirculation in the ischemic zone, stabilizes the cardiomyocyte membrane, participates in the energy transport system, maintaining the level of ATP in the ischemic myocardium.
A meta-analysis of the possibility of using phosphocreatinine, combining data from 41 studies and almost 3.5 thousand observations, showed that in patients with myocardial damage, the use of the drug can reduce mortality by more than 3 times.
Professor Bondarev also shared his own observations on this issue. A survey of 25 patients who had viral pneumonia was performed. The entire group, according to the Temporary recommendations, was prescribed aerobic breathing exercises. In addition, 15 patients received medicinal support in the form of the drug Neoton at a dose of 4 g per 100 ml of saline solution for 7 days. The results of therapy were assessed using a 6-minute walk test. If before rehabilitation patients walked an average of 200 m in 6 minutes, then in patients after exercise therapy this figure improved to 270 m, and in the group with additional use of Neoton - up to 300 m. Patients in both groups noted an improvement in mobility indicators, a decrease in shortness of breath, and anxiety . However, the improvement in daily activity and reduction in shortness of breath in the Neoton group was more pronounced.
In conclusion, Sergei Anatolyevich emphasized that the treatment of comorbid patients with SARS-CoV-2 requires maximum effort and effort of a multidisciplinary team. It is extremely important to select safe and highly effective drugs to restore energy exchange in the myocardium, as well as patient motivation and compliance with medication prescriptions.
| Yuri Aleksandrovich VASYUK , Doctor of Medical Sciences, Professor, Head of the Department of Clinical Functional Diagnostics of FPDO, Scientific Secretary of the Federal State Budgetary Educational Institution of Higher Education MGMSU named after. A. I. Evdokimova Ministry of Health of Russia |
The topic of the need for cardiometabolic support was continued by Yuri Aleksandrovich Vasyuk, Doctor of Medical Sciences, Professor, Head of the Department of Clinical Functional Diagnostics of FPDO, Scientific Secretary of the Federal State Budgetary Educational Institution of Higher Education MGMSU named after. A. I. Evdokimov of the Ministry of Health of Russia , in his speech “Interrupt or continue? Cardiac complications of chemotherapy."
Yuri Alexandrovich noted with regret that the number of cancer patients is steadily growing. If in 2021 the incidence of cancer worldwide was 17 million people and 10 million needed chemotherapy, then, according to experts, by 2040 the incidence will be 26 million people and 15 million will need chemotherapy. Thus, the relative increase in the need for cancer treatment will be 53%.
Chemotherapy, targeted therapy and radiation therapy have provided significant improvements in survival with preserved social adaptation for many years. But, unfortunately, these drugs have a number of serious cardio- and vasotoxic side effects, the development of which significantly increases the mortality of patients. Even if patients achieve recovery from the underlying disease, the first cause of mortality in the long-term period is CVD: chronic heart failure (CHF), coronary heart disease (CHD), arterial hypertension, myocarditis, pericarditis, valvular lesions, thromboembolism, conduction disorders, etc. .
A study of the causes of mortality in cancer patients, conducted according to 7-year follow-up of 1807 patients, showed that the cause of death in 51% was cancer, and in 33% - CVD. In a longer period, the proportion of mortality due to cardiovascular causes increases to 50%. In most cases, the cause of death is CHF, which develops against the background of cardiotoxicity, which all 9 types of antitumor agents have to one degree or another. Today, about 1,500 new chemotherapy drugs are being developed around the world, but almost all of them also have cardiotoxicity.
The risk of cardiotoxicity depends on the antitumor treatment (type, dose, regimen and route of administration) and on the patient (age over 65 or under 15, presence of cardiovascular risk factors or concomitant cardiovascular or other pathology, characteristics of the tumor itself). Professor Vasyuk emphasized that this risk must be carefully assessed and controlled, and patients must be regularly monitored. Quite effective monitoring tools are echocardiography, two- and especially three-dimensional new methods for assessing myocardial deformation (in particular, global longitudinal), as well as MRI and assessment of a number of laboratory parameters, including natriuretic peptides and high-sensitivity troponin.
Today, there are many algorithms for the management of patients with identified cardiotoxicity and even the management of patients undergoing chemotherapy for the purpose of primary prevention of cardiotoxicity. They include limiting the dose or duration of infusion of anthracyclines, the use of dexrazoxane, cardioprotectors, beta blockers, RAAS inhibitors, and statins. In recent years, myocardial cytoprotectors have been widely prescribed, since their mechanism of action makes it possible to correct the adverse effects of anthracyclines: if antitumor drugs disrupt ATP synthesis, then myocardial cytoprotectors normalize the synthesis and transport of energy.
Thus, one of the most promising cardioprotective drugs, phosphocreatinine, maintains the structural integrity of the cardiomyocyte membrane, ensures ATP resynthesis in mitochondria, energy transport to places of consumption, and supports the functioning of ion channels and the contractile function of the heart in conditions of ischemia, toxic and infectious myocardial damage. The use of phosphocreatinine for toxic effects on the myocardium due to membrane protection reduces the number of dead cardiomyocytes by 2 times.
Studies show that phosphocreatinine improves myocardial contractility in patients with myocardial damage during treatment with epirubicin and docetaxel, increasing ejection fraction by 5%. Other work has demonstrated that the use of phosphocreatinine throughout 6 cycles of chemotherapy in breast cancer patients reduces myocardial damage, as evidenced by lower levels of cardiac troponin T and C-reactive protein. As a consequence, phosphocreatinine improves the quality of life and tolerability of anthracycline therapy by reducing their cardiotoxic effect. Professor Vasyuk emphasized that early initiation of cardioprotective therapy in patients undergoing chemotherapy treatment increases its effectiveness and reduces the risk of complications.
| Igor Aleksandrovich KOZLOV, Doctor of Medical Sciences, Professor of the Department of Anesthesiology and Reanimatology of the State Budgetary Institution of Healthcare of the Moscow Region MONIKI named after. M. F. Vladimirsky |
In the next speech “Operate or postpone? We identify and reduce perioperative cardiac risks" Igor Aleksandrovich Kozlov, Doctor of Medical Sciences, Professor of the Department of Anesthesiology and Reanimatology of the State Budgetary Institution of Healthcare of the Moscow Region MONIKI named after. M. F. Vladimirsky , drew the attention of colleagues to one of the most pressing problems - the high cardiovascular risks of non-cardiac operations. According to the speaker, the question of whether to operate or not has become increasingly pressing in recent years due to the increase in the number of elderly and senile patients, among whom there are many patients with high cardiac risk.
Among the 100 million patients over 45 years of age who undergo major noncardiac surgery each year worldwide, 3 million experience perioperative myocardial infarction. A targeted study to identify and predict the risks of cardiac complications in elderly and senile patients, conducted at the Russian Institute of General Reanimatology, showed that the overall incidence of cardiac complications is approximately 9%. This figure in itself is large, but the mortality rate for the development of cardiac complications in such patients turned out to be much more dramatic - 45.5%.
A very recent study, carried out jointly with specialists from Yaroslavl, was also devoted to assessing the incidence of cardiac complications after non-cardiac surgery within 12 months after discharge from the hospital. The results showed that cardiac mortality among patients 45-83 years old reaches almost 3%, and the frequency of the combined endpoint, which includes cardiac mortality, heart attack, stroke, hospitalization due to exacerbation of CVD, was almost 28%.
Thus, the relevance of the problem is extremely high, and accordingly there is a high need to implement a risk-reducing strategy, which should consist of predicting the risk of complications, optimizing perioperative monitoring and timely diagnosis of complications, as well as pharmacological cardioprotection during the perioperative period.
However, the implementation of such a strategy in Russia faces serious difficulties. Professor Kozlov noted that today, unfortunately, we cannot confidently predict complications, since modern indices recommended by foreign and domestic experts do not provide sufficient predictive power of the models. However, the very fact that a patient has IHD or CHF should alert the doctor.
The situation with diagnostics in our country, unfortunately, is also far from ideal. A survey of 125 hospitals in 59 cities showed that the use of the widely recommended V chest lead is implemented only in 37% of hospitals, routine ECG after non-cardiac operations is implemented in 26% of hospitals, and not a single hospital uses routine monitoring of cardiac-specific troponins. Therefore, the third component of the risk-reducing strategy—pharmacological cardioprotection—is of particular interest.
The idea of cardioprotection attracts close attention from the international medical community - research is constantly being conducted, papers are being published, and recommendations are being updated. However, so far most of the updates come down to the abandonment of certain measures of pharmacological cardioprotection. Thus, alpha2-adrenergic receptor agonists, calcium channel blockers, nitrates have been tested and are not recommended for prophylactic use on the eve of and/or during surgery; the use of beta blockers is also questioned. In this regard, there is a natural interest in cardioprotection through metabolic modulation of the myocardium. Exogenous phosphocreatinine occupies a worthy place in the cohort of metabolically active drugs.
When considering the state of myocardial bioenergetics against the background of heart disease and heart failure, it turns out that it is phosphocreatinine and the components of the phosphocreatinine kinase system that are most inhibited. This creates undoubted prerequisites for the use of exogenous phosphocreatinine, a biologically active substance capable of regulating sarcolemmal and intracellular enzyme systems, capable of zwitterionic interactions, and also indirectly affecting oxygen transport by improving blood rheology.
As a result of a number of studies, it has been proven that the addition of phosphocreatinine to standard therapy reduces the degree of myocardial damage, prevents the development of arrhythmias, reduces cardiac remodeling, improves EchoCG indicators of systolic and diastolic function of the left ventricle, reduces the level of blood BNP, the severity of symptoms of CHF, and increases tolerance to physical activity.
Phosphocreatinine has also been studied for use in noncardiac surgery. One of the first works was to study its use in high-risk vascular operations. It turned out that perioperative one-day use of the drug allows for a significantly higher level of left ventricular ejection fraction and a multiple reduction in the incidence of serious ventricular arrhythmias in the perioperative period according to Holter monitoring.
Data from a study of the use of phosphocreatinine during orthopedic operations in elderly patients under epidural anesthesia demonstrated that the administration of 2 g of phosphocreatinine during the intraoperative period can achieve a multiple reduction in the risk of threatening cardiac arrhythmias and discomfort in the cardiac region.
More recently, a randomized study of the cardioprotective effects of phosphocreatinine during cancer surgery in elderly patients was conducted in Obninsk. It turned out that the administration of phosphocreatinine for 5 days before surgery and 3 days after not only almost completely eliminated the likelihood of developing acute coronary syndrome, but also significantly reduced the overall incidence of complications and shortened the length of the patient’s hospital stay.
More recently, a group of clinicians led by Professor Yavorovsky, as a result of a multicenter prospective randomized study assessing the effectiveness and safety of exogenous phosphocreatinine in patients undergoing general surgery, obtained new interesting data. Preliminary results show that phosphocreatinine can significantly reduce the incidence of intraoperative and postoperative ischemia, as well as the level of cardiac-specific troponin T in the postoperative period.
Thus, answering the question whether to operate on elderly and senile patients with a high cardiac risk or not, we can confidently say that yes, but under conditions of competent cardioprotection.
| Yuri Mikhailovich LOPATIN , Doctor of Medical Sciences, Professor, Head of the Department of Cardiology, Cardiovascular and Thoracic Surgery, Institute of Continuing Medical and Pharmaceutical Education, Volgograd State Medical University, Ministry of Health of Russia |
Yuri Mikhailovich Lopatin, Doctor of Medical Sciences, Professor, Head of the Department of Cardiology, Cardiovascular and Thoracic Surgery of the Institute of Continuing Medical and Pharmaceutical Education of the Volga State Medical University of the Ministry of Health of Russia , devoted his report to the topic “Possibilities of metabolic therapy of CHF in patients with coronary artery disease.”
Yuri Mikhailovich also noted that recently the issue of energy support during the CVD has become very relevant. In his opinion, this seems very logical, since the mechanisms of development of heart failure and ischemia necessarily include a violation of the energetic functions of the heart muscle.
Professor Lopatin emphasized that the study of the cardiometabolic effects of various drugs or food products has been carried out for a long time, but there are still very few drugs with proven effectiveness. The fact is that in this matter there is little understanding of the pathophysiology of energy deficiency and theoretical knowledge of how this or that drug can affect it. It is extremely important to be able to clinically prove their effectiveness, and it is precisely this stage that, despite the abundance of long-term work, many of the promising drugs have not passed.
One of the most interesting products that shows good results in various tests is Neoton. Today there are publications on the effectiveness of using phosphocreatinine in a wide range of conditions. It has proven its capabilities in preventing myocardial rupture, reducing the frequency of arrhythmias, influencing cardiac remodeling and more. A meta-analysis of the use of phosphocreatinine shows a convincing reduction in mortality (3.5% vs. 10.6%) and arrhythmia (12% vs. 22%), an increase in left ventricular ejection fraction (50% vs. 46%), and a decrease in the need for inotropes (17% vs. 35%) compared to the control.
Research on the use of phosphocreatinine for intraoperative myocardial protection seems very optimistic, because cardiac surgery patients certainly need pharmacological support that reliably leads to a reduction in myocardial damage. During the period of exacerbation of CHF, phosphocreatinine is a good potential assistant to the drugs that doctors have at their disposal. Administration of the drug in therapeutic doses and subsequent therapy with maintenance doses allows not only to gain time, but also to create conditions for the beneficial effects of other drugs.
CONFLICT OF INTEREST. The author of the article has confirmed that there is no conflict of interest to disclose.
CONFLICT OF INTERESTS. Not declared.
E. O. Girutskaya
Magazine “Treating Doctor”, Moscow, Russia
Nosological features of myocardial damage: review of the symposium / E. O. Girutskaya For citation: Girutskaya E. O. Nosological features of myocardial damage: review of the symposium // Treating Physician. 2021; 6 (24): 56-59. DOI: 10.51793/OS.2021.24.6.012 Tags: heart, myocardium, energy support, coronavirus infection
Symptoms of myocardial infarction
The severity of signs of a heart attack depends on the stage of the disease.
The pre-infarction period is not observed in all patients; it occurs in the form of exacerbation and increased frequency of angina attacks and can last hours and days, or several weeks.
The most acute period is accompanied by the development of myocardial ischemia and the formation of an area of necrosis, lasting from 20 minutes to 3 hours. The main symptom is burning or pressing pain, which often appears due to physical activity or severe stress. The pain may radiate to the left arm, shoulder, neck, shoulder blade or lower jaw.
Painful sensations vary in duration (more than 30 minutes) and are not relieved even by repeated administration of nitroglycerin.
Other symptoms of myocardial infarction:
- cold sweat;
- fear of death, severe weakness;
- shortness of breath, suffocation;
- sometimes vomiting.
First aid for myocardial infarction: if you detect at least a few of the listed symptoms, you must immediately call an ambulance! The patient must be put down and have access to fresh air. Before the arrival of the medical team, it is possible to take 1 tablet of nitroglycerin (or 1 dose of isoket) under the tongue.
The acute period of myocardial infarction begins from the moment of formation of a focus of necrosis on the myocardium and lasts from 2 to 14 days.
During this period, a person may not experience pain. Due to the formation of an area of necrosis and inflammation of the heart tissue, body temperature rises. The patient's symptoms of cardiovascular failure persist and increase. Blood pressure is low or normal.
First aid is the same: immediately go to an ambulance.
The subacute period is accompanied by the formation of scar tissue and lasts 4-8 weeks. This period of myocardial infarction is not characterized by heart pain and fever.
The patient's condition is normalized, blood pressure and pulse rate are gradually approaching normal, and manifestations of cardiovascular failure are weakening.
Post-infarction period - all symptoms disappear, laboratory parameters gradually return to normal. The body adapts to the consequences of changes in the structure of the heart muscle.
Symptoms of myocardial infarction in atypical forms of the disease:
Abdominal - symptoms are masked as signs of abdominal diseases: pain and bloating in the abdomen, nausea. Asthmatic - the patient experiences shortness of breath and attacks of suffocation. Cerebral - manifestations of brain disorders: headache, dizziness, confusion. Arrhythmic - a person complains of rapid heartbeat or irregular heartbeat. Edema form - there is pronounced peripheral edema of soft tissues.
1 Diagnosis of heart attack in MedikCity
2 Diagnosis of heart attack in “MedicCity”
3 Diagnosis of heart attack in MedikCity
Signs of a major heart attack
The causes and consequences of a massive heart attack are scary in their suddenness, since in most cases it overtakes a person by surprise. Knowing what it is and having an idea of the possible results, you will be able to recognize the pathology and seek medical help in time. A heart attack is characterized by:
- severe pressing pain behind the sternum, which can radiate to the left upper part of the body;
- increased sweating;
- numbness of the left hand;
- changes in skin color (pallor);
- increased heart rate;
- the onset of a feeling of fear;
- decrease in pressure;
- heart rhythm disturbances;
- weakness;
- pain in the abdomen, vomiting that does not bring relief (if the posterior wall of the myocardium is damaged).
The development of an acute heart attack in some cases is not accompanied by pain, but despite this, this condition also requires emergency measures, since a second heart attack can occur several hours (or even minutes) after the first.
To avoid irreversible consequences, the victim must be provided with assistance before the doctor arrives. First, you need to give the person nitroglycerin. After this, the patient should be placed on a flat surface and his head should be tilted up (if a person is vomiting, the person should be turned on his side). In cases where nitroglycerin does not have the desired effect, the patient is given an injection of analgin or promedol.
Be sure to help the patient get rid of removable dentures (if any), since there should be as few obstacles to the maximum supply of oxygen to the lungs as possible. And if a person is unconscious and cannot breathe on his own, he will need artificial ventilation.
Complications of myocardial infarction
The overwhelming majority of deaths from heart attack occur in the first hours and days and are associated with complications of myocardial infarction:
- Life-threatening arrhythmias - ventricular tachycardia, ventricular fibrillation, cardiac arrest;
- Cardiogenic shock is a condition that develops with extensive damage to the left ventricular myocardium and is characterized by a progressive decrease in blood pressure and impaired blood supply to vital organs;
- A cardiac aneurysm and its rupture are thinning of the heart wall and its protrusion under the pressure of blood in the ventricles. If an aneurysm ruptures, tamponade and cardiac arrest occur;
- Cardiac tamponade is a deadly complication of a cardiac aneurysm in which blood leaks into the pericardial cavity after the aneurysm ruptures. As a result of the rapid filling of the pericardium with blood, the heart can no longer carry out its pumping function and stops;
- Rupture of the interventricular septum;
- Acute heart failure (pulmonary edema);
- The occurrence of complete atrioventricular block and a decrease in heart rate to 20-30 per minute.
Myocardial infarction of the posterior wall of the left ventricle
Myocardial infarction of the posterior wall is more difficult to diagnose electrocardiographically than myocardial infarction of the anterior wall.
According to ECG and autopsy comparisons, almost half of these infarctions are not visible on the ECG. The posterior wall of the left ventricle is conventionally divided into 2 parts:
- the diaphragmatic part of the posterior wall, - the basal part of the posterior wall.
Posterior phrenic (posterior) myocardial infarction.
The signs characteristic of such a heart attack are determined in the III standard, aVF and are usually supported by the II standard lead.
The Q wave in leads III and aVF is considered pathological if it exceeds 1/2 of the R wave and is wider than 0.03 s. In transmural infarction, QS is usually recorded in leads III and aVF. The pathological Q wave III, aVF is usually combined with a reduced R in these leads and with characteristic changes in ST and T. Since the Q wave in standard lead III can be present even in healthy people, the pathological Q III during a heart attack is necessarily combined with pathological Q in aVF and a Q wave in the II standard lead, which in it should exceed 10% of the R wave. Myocardial infarction of this localization is also characterized by Q(II)>Q(I) (normally QI>QII). It is also typical for cicatricial infarction that R(aVF)
In the acute stage of a posterior diaphragmatic infarction, reciprocal changes are observed in V1 - V3: ST decreases and a high positive “coronary” T wave appears, and the dynamics of ST and T in the precordial leads occurs faster than in III and aVF. ( See ECG
)
Posterobasal (basal) myocardial infarction.
This high left ventricular myocardial infarction is particularly difficult to diagnose and is often underdiagnosed. This is due to the fact that there are no direct signs in the 12 mandatory leads. For the most part, the diagnosis of posterobasal myocardial infarction is made by reciprocal changes in the electrocardiogram.
Sometimes direct signs of infarction of the basal parts of the posterior wall can be detected in additional chest leads V7 - V9, in the dorsal lead along the Sky. In these leads, a pathological Q wave with typical ST and T dynamics can be recorded. Reciprocal changes are recorded in leads V1 - V3.
The most specific changes are:
— increase in the amplitude of V1 and V2, with R(V1) > S(V1), — decrease in the depth of the teeth S(V1) and S(V2), — R/S ratio in V1, V2 >= 1.0?
- widening of the initial R(V1), when R(V1)>= 0.04 s., - notching of R (V1-2), reminiscent of incomplete blockade of the right bundle branch, - decrease in ST (V1-2) in the acute phase of a heart attack with gradual reverse dynamics - the appearance in the acute phase of high positive “coronary” T waves in V1 - V3-4, and their height gradually increases. ( See ECG
).
Despite numerous indirect signs, all of them may be absent in cases of known basal myocardial infarction.
Often, changes in posterobasal infarction must be differentiated from electrocardiographic signs of right ventricular hypertrophy. Unlike a heart attack, with right ventricular hypertrophy there are characteristic changes in the left precordial leads.
Diagnosis of myocardial infarction
First, the doctor examines the patient and collects information from the patient or his relatives about the nature and duration of pain, the strength and frequency of attacks, medications taken, and their effect on well-being.
Next, laboratory and instrumental diagnostics of myocardial infarction are carried out:
- general and biochemical blood tests (usually in a hospital setting);
- study of cardiac-specific enzymes and markers of damage to the heart muscle (usually in a hospital setting);
- electrocardiography;
- echocardiography (ultrasound of the heart);
- coronary angiography (in a hospital setting).
Diagnosis of extensive infarction
In addition to analyzing clinical manifestations, extensive myocardial infarction can be diagnosed using electrocardiography and a number of laboratory tests. These methods are especially relevant for detecting atypical and ambiguous forms of pathologies of the heart and blood vessels.
The consequences of an extensive heart attack are changes in blood test parameters, namely:
- leukocytosis;
- increased erythrocyte sedimentation rate;
- the appearance of C-reactive protein;
- increased levels of fibrinogen and sialic acids.
When diagnosing the disease, it is very important to exclude the possibility of other abnormalities that are similar to a heart attack in their clinical signs. For example, chest pain can bother a patient if he has acute pericarditis, angina pectoris, intercostal neuralgia, etc.
Treatment of myocardial infarction
Intensive care measures for acute myocardial infarction may include:
- administration of thrombolytic agents to dissolve the blood clot and restore blood flow in the myocardium;
- pain relief (narcotic analgesics are often used);
- stabilization of blood pressure;
- the use of antianginal, antiarrhythmic drugs, anticoagulants, antiplatelet agents, beta blockers, ACE inhibitors, etc.
Surgical techniques are often used in the treatment of myocardial infarction:
- angioplasty (expansion of a narrowed vessel using a balloon catheter);
- coronary stenting (installation of a stent at the site of narrowing of the coronary artery, after its expansion with a balloon);
- shunting (suturing a shunt that bypasses the narrowed area).
Post-hospital treatment of myocardial infarction (outpatient management after discharge from hospital) also includes a number of activities:
- observation by a cardiologist;
- pharmacotherapy;
- blood pressure and heart rate control;
- diet;
- avoiding stress, overwork and strain;
- recommended physical activity;
- rejection of bad habits.
Diagnosis of myocardial infarction and treatment of patients who have suffered a myocardial infarction at MedikCity
At the MedicCity clinic, the diagnosis of myocardial infarction and treatment of patients who have suffered a myocardial infarction, as well as those suffering from other cardiac diseases, are carried out at the highest professional level.
Our cardiologists are armed with the best expert-level equipment, extensive scientific knowledge and the latest developments!
We have reasonable prices and an individual approach. You can find out the schedule of specialists and the cost of services by calling: +7 (495) 604-12-12.
"MedicCity" is the right choice!
Treatment tactics for large infarction
In order for the consequences after a major heart attack to have minimal impact on the further functioning of all body systems, it is necessary to follow the step-by-step treatment of this pathology.
- The prehospital stage is the provision of assistance before the arrival of the medical team and delivery of the patient to a medical facility.
- Hospital - the use of medications in a hospital setting to stabilize the heart rate, eliminate and prevent the formation of new blood clots, etc.
- Rehabilitation procedures.
- Observation and outpatient treatment.
An acute attack must be accompanied by mandatory placement of the victim in a hospital. In order to remove obstacles to the blood flow to the affected area, thrombolytic therapy is prescribed.
These drugs help eliminate plaque in blood vessels and restore blood flow. The optimal time to take thrombolytics is considered to be the first six hours after a major heart attack. This allows you to avoid the most dangerous consequences.
The following drugs have the effect described above:
- Heparin.
- Aspirin.
- Plavix.
- Prasugrel.
- Fraxiparine.
- Alteplase.
- Streptokinase.
In addition, in order to eliminate pain, the following is prescribed:
- Promedol.
- Morphine.
- Fentanyl with droperidol.
Read material on the topic: Serving the elderly: from nurses to robots
You can stabilize the heart rate after a major heart attack using droppers with a magnesium solution. In addition, calcium antagonists, nitrates and β-blockers are prescribed to activate blood supply. The patient's pronounced feeling of fear is suppressed with tranquilizers.
When taking medications is contraindicated or does not have the desired effect, emergency coronary artery bypass surgery comes to the rescue. Sometimes this is the only possible option to improve the patient's condition.
Having suffered a massive heart attack requires mandatory rehabilitation. Part of the treatment and elimination of the consequences of the pathology that has occurred is compliance with bed rest for 14 days after the attack. At the same time, it is worth minimizing all physical stress on the body: you even need to walk with great care. The standard length of stay in a medical facility is approximately 21 days. Staying under medical supervision is also mandatory for those patients who have suffered a heart attack on their legs.
Causes of the disease
- Myocardial infarction almost always develops against the background of atherosclerosis of the heart vessels, the so-called. coronary arteries. When the integrity of an atherosclerotic plaque is disrupted, a blood clot forms in the lumen of the vessel, which leads to a sudden cessation of blood flow in the artery of the heart and myocardial infarction.
- Very rarely, an acute disruption of the blood supply to the heart muscle can occur during prolonged spasm of the coronary arteries, for example, during physical or psycho-emotional overload.
At CELT you can consult a cardiologist.
- Initial consultation – 3,500
- Repeated consultation – 2,300
Make an appointment
Prevention of pathology
Life does not end after a massive heart attack, but such patients should completely change their habits. To reduce the likelihood of relapse, the following recommendations from specialists should be strictly followed:
- Visit your doctor regularly to prevent complications, undergo a full medical examination and strictly follow the specialist’s instructions.
- Taking acetylsalicylic acid.
- Complete cessation of bad habits.
- Long walks in the fresh air.
- Daily therapeutic exercises.
- Balanced diet, low in fat and salt.