Supraventricular extrasystole (SVES) is a deviation of the heart rhythm from the norm, in which additional cardiac impulses occur. As a result of this process, extraordinary and defective contractions of the heart occur. Most often, this pathology occurs in patients with heart problems. In the article we will understand what it is, why frequent manifestations are life-threatening, and what consequences follow from ignoring the symptoms.
What does it represent?
With supraventricular extrasystolic arrhythmia, the source of the spread of extraordinary contractions is localized above the ventricles. With such a deviation, a center of trigger activity is formed, sending periodic impulses out of turn. The ICD-10 code for this violation is 149.3.
Ventricular and supraventricular extrasystole can be determined by the severity of symptoms.
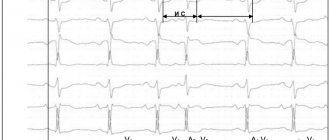
In the first case it will be more intense. To identify characteristic criteria and diagnose signs, it is enough to conduct a standard ECG (pictured). Diagnosis of supraventricular disease is complicated because the ECG will show a wide QRS complex.
Diagnostics
The first thing you should pay attention to when diagnosing supraventricular extrasystole is the clinical signs. This pathology is characterized by unpleasant sensations in the chest, which cause significant discomfort, but cannot be called pain.
To confirm the diagnosis, the patient must undergo an ECG and 24-hour Holter monitoring.
On the ECG, supraventricular extrasystole looks like this:
- expansion and deformation of the atrial P wave ahead of time;
- the P wave is followed by the normal ventricular complex;
- the compensatory pause is incomplete;
- if the origin of the extrasystole is atrioventricular, the P wave may not be detected or may be observed after the ventricular complex.
Reference! Supraventricular extrasystole on the ECG manifests itself clearly and leaves no doubt for making a diagnosis.
Classification
There are several classifications of supraventricular extrasystole. At the location of the source of excitation, the following varieties are distinguished:
- atrial – upper parts of the heart;
- antrioventricular - the septum between the ventricles and the atrium.
Depending on the frequency of extrasystoles in 1 minute: single (single), multiple, group and paired. With a single type, up to 5 additional contractions are observed, with multiple ones – more than 5. The group type involves several extrasystoles at once, which come one after the other, the paired type – 2 extrasystoles come in a row.
Rare and frequent extrasystoles can be distinguished.
Causes
Most often, supraventricular extrasystole occurs against the background of heart disease. However, there are a number of other common reasons that can trigger the development of such a disease. These include:
- drug exposure - uncontrolled use or overdose of diuretic or antiarrhythmic drugs;
- problems with electrolyte metabolism - low concentrations of calcium, sodium and potassium in the blood;
- poisoning or intoxication - excessive alcohol consumption, negative effects of chemicals and smoking, infectious diseases;
- diseases of the nervous system – neurocirculatory dystonia;
- endocrine diseases - diabetes mellitus, increased or decreased activity of the thyroid gland, menopause or the onset of menstruation;
- unhealthy lifestyle – frequent stress, heavy physical activity, increased nervousness, low physical activity.
Reference! In some cases, the cause of the development of the pathological condition cannot be determined.
Sometimes extrasystoles of the supraventricular type occur as an independent disease, but this is very rare - about 5-10% of all cases. In 50% of cases, the reason for the development of such a deviation is the presence of cardiac pathology.
Archives
O. Y. Zharinov, V. O. Kuts National Medical Academy of Postgraduate Education. P. L. Shupika Ministry of Health of Ukraine
Extrasystole (ES) is the most widespread disturbance of the heart rhythm, which can significantly influence the life quality of patients, being a marker of structural and functional changes in the myocardium and indicate the unsafety of life unsafe You have heart arrhythmia. A more refined strategy for the management of ill patients is directly linked to the development of the concept of “stratification of risk”, so that patients are divided into groups according to the level of risk of death from all causes and, among other things, cancers. about cardiac death (CCD). In addition, day-to-day instrumental methods for diagnosing cardiac arrhythmias are being actively promoted, including ambulatory ECG monitoring. In clinical practice, there is an obvious need for the creation of favorable recommendations for the management of cervical diseases, specific diagnostic and therapeutic approaches.
ETIOLOGY
When SHE appears, they can call out any structural illness of the heart. They are especially common in patients with acute myocardial infarction (MI) and chronic ICH. However, extrasystoles can also occur with other myocardial stresses, including subclinical ones. In many patients with extrasystole, no available instrumental methods of investigation can be used to detect any signs of a weakened heart.
Wider causes and factors associated with SE:
- Ailments of the myocardium, endocardium and cerebrovascular arteries: ICH, myocarditis, myocardiofibrosis, cardiomyopathy, blood vessels, arterial hypertension or hypotension, heart failure (HF);
- Electrolyte imbalance (hypokalemia, hyperkalemia, hypomagnesemia, hypocalcemia), impaired acid-salinity;
- Hypoxia: sick leg, pulmonary hypoventilation (for example, during surgery);
- Traumatic injuries: chest injury, heart surgery, empty heart catheterization, brain and spinal cord injuries;
- Impaired autonomic regulation: neurocirculatory dystonia, neuroses, diencephalitis, sympathetic ganglionitis and truncitis, psychoemotional stress;
- Pathological reflexes, diseases of the organs and poisoning (virazkova disease, gum disease, pancreatitis, diaphragmatic clubina, colitis and enterocolitis, especially if they are accompanied by flatulence, constipation or electrolyte disturbances balance); dystrophic changes in the cervical and thoracic lobes of the ridge (osteochondrosis, spondyloarthrosis); bronchial diseases and illnesses, especially those accompanied by a persistent cough; prostate adenoma;
- Diagnostic procedures: endoscopy (bronchoscopy, gastroscopy, laparoscopy, cystoscopy, colposcopy, rectoscopy), puncture, carotid sinus massage, pressure on the apple of the eye, breathing while holding a deep breath;
- Allergies: food, medicinal, microbial, occupational, household;
- Pharmacodynamic and toxic effects of medications such as cardiac glycosides, quinidine, novocainamide, anesthetic agents, morphine, glucocorticoids, potassium, calcium preparations, tricyclic antidepressants, related phenotiases in other words, adrenomimetics.
The main electrophysiological mechanisms of extrasystole are re-entry (return input of awakening) and post-depolarization. The basis for extrasystoles may also be the mechanisms of asynchronous renewal of myocardial alertness and pathological automatism.
COLLABORATION OF THE SICK
Treatment of patients with cervical heart disease includes methods to ensure the diagnosis of cardiac rhythm disturbances, determination of the clinical and prognostic significance of arrhythmia, choice of treatment and assessment of its effectiveness.
Anamnesis.
When examining a patient, provide the following information: subjective manifestations of arrhythmias (heart palpitations, interruptions in the functioning of the heart, problems or a “frozen” heart, discomfort in the chest, due to insufficient wind, shortness of breath, confusion, syn digging camps), ancient history of destruction of the rhythm; factors that provoke arrhythmia (physical stress, psycho-emotional stress, late hour of prey, body position, food intake, alcohol, chicken); endured the remaining hours of illness; background cardiac pathology; advance use of antiarrhythmic drugs (AAP).
Clinically quilted.
Identification of arrhythmias during auscultation of the heart or during palpation of peripheral arteries; presence of clinical signs of HF.
Laboratory methods of investigation.
Valued instead of potassium, sodium, creatinine in blood serum, thyroid-stimulating hormone activity.
EKG.
Main ECG signs of extrasystoles (ES):
- It is preceded by the appearance of a widened and deformed intrabasic rhythm of the QRS complex without the P wave transmitted to it, after late extrasystoles, before which the P wave is registered, which does not impair the electrophysiological connection with the neck;
- Most often, a new compensatory pause is evident.
The shape of SH is not only due to the localization of the extrasystole, but also due to the fluidity and direction of the expansion of the impulse in the shanks. Therefore, the ECG makes it possible to determine the location of the ectopic cavity behind the morphology of the extrasystolic complex. It appears that there is a blockade of the right leg and the left anterior bundle of His, and it should be located in the system of the left posterior bundle of His, or in the posterior wall of the left bundle; It appears that there is a blockade of the right leg and the posterior inferior ganglion of the His bundle, which is located in the left anterior ganglion of the His bundle; If there appears to be a complete blockade of the left branch of the His bundle, then there is a blockage in the right branch of the His bundle. The QRS complex of the left ventral extrasystole in the right thoracic abductions has a mono- or biphasic form: R, qR, RR', RS, Rs and in the left ones - rS or QS. The QRS complex of the right ventricular extrasystole in the right thoracic adducts takes the form rS or QS, and in the left - R (Table 1). This is due to the dilation of the interstitial septum, as, of course, its length and shape slightly vary in relation to the QRS complex of the main rhythm. The QRS shape of the rSR' type in V1 is typical for extrasystoles from the left half of the interseptal septum, and the R or qR type in V6 is typical for extrasystoles from the right half of the septum. The directness of the QRS complex of the extrasystolic complex in all thoracic abductors allows localization of the cerebral muscle in the basal lobes of the heart, and the directness of the QRS complex in the lower abdomen allows for localization of the thoracic abductor in the basal lobes of the heart. In cases that are difficult for topical diagnostics, it is more precise that extrasystoles are not indicated, surrounded by a warning about the presence of E.
Table 1. Characteristic forms of NEC complexes in thoracic ECG leads with basal, perineal and superior localization
| Localization of extrasystoles | Forms of NHE complexes in ECG extensions | ||||||
| V1 | V2 | V3 | V4 | V5 | V6 | ||
| Right lunochkovi | Basal | Rs, Rs | R.S. | R | R | R | R |
| Crotch | rS, QS | rS | rS | rS, RS | R | R | |
| Livoshlunochkovi | Verkhivkov | rS, QS | rS, QS | rS | rS | rS, RS | Rs, Rs |
| Basal | R | R | R | R | Rs | RS, Rs | |
| Crotch | R, qR, RR', RS, Rs | R, Rs | R.S. | RS, RS | rS | rS, QS | |
| Verkhivkov | RS, Rs | rS, RS | rS | rS | rS | rS | |
| Basal | R | R | R | R | R | R | |
| Verkhivkov | rS | rS | rS | rS | rS | rS | |
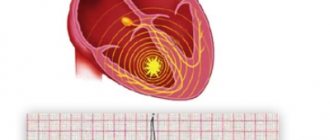
The intervals of aggregation of monotopic HE are, however, regardless of the fact that their form may be different (in this type the stench is polymorphic). The intervals for the accumulation of monotopic extrasystoles should not exceed 0.06–0.10 s. Floods may vary over the course of the consolidation interval and, as a rule, have different shapes of QRS complexes. Two extrasystoles are called guy (Fig. 1), and three to five are called group, “volley” (Fig. 2), or runs of ventral tachycardia - PC. You can also see early and even early SH („R to T”) (Fig. 3). Extrasystoles may be irregular (monotopic or polytopic), and their appearance with regularity is designated as an arrhythmia (bigeminia, trigeminia, quadrigeminia, etc.). Interpolations are registered between two normal QRS complexes, especially against the background of bradycardia.
Picture 1.
Alone and paired polytopic extrasystole.
Figure 2.
Group polytopic shlunochkova extrasystole.
Figure 3.
Early shlunochkova extrasystole “R to T”.
Scholochkovy extrasystole against the background of anterior fibrillation must be differentiated from aberant sluchkovy complexes. The shortening of the cardiocycle during atrial fibrillation, which ends with an aberrant scapular complex, is not accompanied by a compensatory pause, and is transferred to an extended RR interval. Aberrant QRS complexes, as a rule, take the form of blockade of the right leg of the His bundle of varying degrees of severity in the output V1 (rSR', rSr'), and left ventricular extrasystoles - the form R, RS, Rs, qR, RR' or Rr' (Table 2 ).
Table 2. Differential diagnosis of supraventricular extrasystoles with aberation of the internal sac conductivity and sac extrasystoles
| Signs | Supraventricular extrasystole with aberration | Shlunochkova extrasystole |
| QRS morphology in advanced V1: | ||
| rSR', rsR' | Characteristic | Not typical |
| qR, R, rR' with splitting on the output column | Very rarely | Not typical |
| qR, R, RS, Rsr', RR' with splitting on the downstream column | Not typical | Characteristic |
| rS, QS | Not typical | Characteristic |
| QRS morphology in advanced V6: | ||
| qRS | Characteristic | Not typical |
| rS, QS | Not typical | Characteristic |
| Importance of positive and negative teeth of the QRS complex in all chest muscles | Not typical | Characteristic |
OTHER METHODS OF INSTRUMENTAL DIAGNOSTICS
Holter monitoring (HM) of the ECG allows recording of the ECG without compromising the patient's roach mode for 24 years or more with the subsequent automated analysis of the recording. The number of extrasystoles per hour of exercise is assessed, their distribution of activity, connections with physical or emotional stress, heart rate, body intake, changes in body position, transitional episodes, etc. ii myocardium.
HM ECG is a “standard” method for diagnosing apparently infrequent extrasystoles, as well as assessing the severity of ECG detected during ECG registration. CM ECG allows more precise, shorter-term ECG recording to provide a clear and comprehensive assessment of the disturbance of heart rhythm due to a significantly larger number of assessed ectopic complexes. Alone, it is common to find ECG with CM in apparently healthy individuals.
The equalization of circadian changes in the number of extrasystoles and the frequency of heart rate (HR) allows for the increase in fluid intensity of such and bradyseal forms of extrasystoles. One of the broadest types of extrasystoles is the “vagal” (vagal, or “low”), when the frontal complexes are registered 1.5 times less often in the passive period of dob, against the background of sleep Synchronous with sinus rhythm. Vagozalezhnaya is more often diagnosed in young people without signs of heart pathology, it often has an episodic sign and is not considered sick. This form of extrasystole importantly does not require antiarrhythmic therapy. With the “adrenergic” (sympathostatic or “day” type), the average number of extrasystoles per year is 1.5 times greater during the active period of stimulation, and extrasystoles are often associated with accelerated sinus rhythm. The “adrenergic” type is more typical for summer people, especially those with IHD, hypertensive illness, heart disease, dilated and hypertrophic cardiomyopathies, myocardial fibrosis. In contrast to the “vagal” type, such extrasystole is not benign and often requires the use of AAP, beta-blockers and amiodarone. Even often, the daily connection between the number of extrasystoles and the period of increase and heart rate. You can also watch out for the “hectic” type of subdivision of extrasystoles with significant fluctuations from year to year. Such high ectopic activity over a short period of time may be associated with recurrent myocardial ischemia. The use of the HM ECG has significantly increased the possibility of detecting extrasystole and parasystole, establishing the variability of their forms and options.
The HM ECG method allows you to evaluate changes in heart rate variability per day. Zocrema, a decrease in the standard indicator of heart rate variability - standard variation of RR intervals by stretching (SDNN) - below 50 ms indicate an imbalance in the autonomic regulation of heart rate and one of the predictors of guilt RSS in patients with post-infarction cardiosclerosis, left systolic dysfunction (LS) and heart failure and save sinus rhythm. The strongest predictor of the risk of life-threatening arrhythmia was the result of low heart rate variability due to decreased heart rate fraction (EF) and impaired baroreflex sensitivity (follow-up). ATRAMI, 1998). It is clear that measurements are often used to assess hourly and spectral indicators of heart rate variability.
With CM ECG, attention is also paid to the variability and variability of the consolidation interval, as well as the variability of the QT interval. It is important to evaluate the additional fluctuations of the adjusted QT interval, and even with this significant increase, the severity of the “discharge” period of the cardiac cycle and the delay before the onset of paroxysms may increase „pirates-tachycardia”.
Repeated HM ECG against the background of treatment makes it possible to assess the effectiveness of the prescribed therapy. Based on the changes in the spontaneous fluctuations in the frequency of culprit arrhythmias of the heart, the following criteria for the effectiveness of antiarrhythmic therapy in patients with cerebral hypertension have been developed: a) a change in the number of cervical arrhythmias for an additional 50– 75%; b) a change in the number of young and early children by 90% or more; c) externally suspended episodes of ST; d) with polymorphic cerebral neck - a change in the number of morphological types of extrasystoles to 1–2. Assessing the adequacy of treatment with an antiarrhythmic drug, in addition to exceeding the criteria, also requires taking into account the specificity of its effect on sinus rhythm, conductivity, and the frequency of ischemic episodes.
Interpretation of HM ECG data to assess the effectiveness of antiarrhythmic therapy in case of high blood pressure. When the AAP is assigned to the 1st class under classification V. Williams, the effectiveness of the specified clinical criteria does not allow for an improvement in the prognosis of survival of patients with treatment. Moreover, the use of certain drugs (flecainide, encainide) in controlled studies was associated with significant increases in the prevalence of PCC. It is important that the treatment of patients with severe structural disorders of the myocardium (dysfunction of the myocardium after myocardial infarction or dilated cardiomyopathy, with/without heart failure) begins with the therapy of etiopathogenetic Direction: correct ischemia and hemodynamic disturbances. For evidence of LS dysfunction and partial symptomatic ES, amiodarone or sotalol should be added before basic preventive therapy (angiotensin-converting enzyme (ACE) inhibitors, β-blockers, aspirin, statins) - methods with proven effectiveness This is for the prevention of malignant sac arrhythmias. It is significant that beta-blockers and amiodarone can be used empirically, based on the established availability of these drugs, to predict the survival of patients and, regardless of changes in heart rhythm disturbances. In these situations, the HM ECG is completely dynamic to assess the interruption of heart rhythm disturbances against the background of antiarrhythmic therapy. And in situations where the stagnation of AAP is determined by the clinical manifestations of the rhythm disturbance, and not by their prognostic values, the initial criterion for the effectiveness of the drug is a change in symptoms causing arrhythmia. It is also agreed that the most effective way to prevent RSS in patients with high risk criteria is implantation of an internal cardioverter-defibrillator.
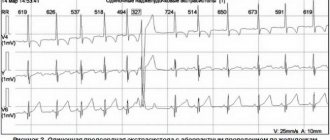
Trying out physical skills
(Master's test, step test, veloergometry, treadmill test) can provoke the appearance of WHILE under the hour of desire and in the early adolescence period due to increased activity of the sympathoadrenal system, an increase in catecholamines , development of tissue hypoxia, acidosis. In patients with chronic ICH, bicycle ergometry under one hour reveals HI in 60% of patients, and its frequency often correlates with displacements of the ST segment (Fig. 4). Under the infusion of physical exercise, the number and gradation of extrasystoles may change: an increase in the number of extrasystoles during the hour of exercise at high heart rate or in the first half after the end of the exercise Consider this possible connection with IHS; “Good” extrasystoles usually appear at the hour of exercise and renew 3–5 hours after its completion. It is necessary to call for diagnostic tests due to the following reasons: in some patients it is not possible to provoke an extrasystole that was previously diagnosed; in 11–40% of patients with a healthy heart, during physical exercise there is a single extrasystole, and in 5% - a pardy; In some patients, with physical stimulation, group and early extrasystoles may occur.
Figure 4.
Right-sided extrasystole against the background of horizontal depression of the ST segment.
Orthoclinostatic test
allows you to clarify the nature of extrasystolic arrhythmia: stable extrasystole occurs at rest during functional tests; Labile extrasystole of voltage appears or becomes stronger during an orthostatic test and a standard applied pressure of 50 W; Labile extrasystole calmly appears during an orthostatic test and physical exertion with a pressure of 50 W and appears after the transition to a horizontal position. It is important that labile extrasystole of stress and stable extrasystole are more likely to be associated with the presence of heart disease and/or a stable substrate of arrhythmia, and labile extrasystole of calm, as a rule, є functional (vagal).
Echocardiography
It is necessary to clarify the infusion of both SE and AAP on the hemodynamic stage. The method allows you to estimate the size of the empty heart in systole and diastole, the vascular fraction, the thickness of the heart walls, the mass of the myocardium of the heart, the relationship between the end-diastolic volume and the mass of the myocardium of the heart, and zones of hypo- and akinesia, local hypertrophy, valvular valves, the phenomenon of “post-systolic “strengthening”, myocardial dysplasia of the right shank. A change in LVEF of less than 40% in patients with IHS is associated with an increased risk of RSS. Cardiac dysfunction can be more accurately determined using radioisotope ventriculography or coronary ventriculography.
Inner-Heart EED
It is a routine method for diagnosing disturbances in cardiac rhythm and conductivity, an important indication for cardiac pacing, radiofrequency catheter ablation and implantation of a cardioverter-defibrillator. The investigation is carried out in specially equipped laboratories. There are no absolute indications for performing intracardiac EPD in patients with SHE. This investigation may be even more useful if it is necessary to establish a connection between the heart rhythm and syncope and presyncope. If you are ill with asymptomatic excess of extrasystole, EPD is not indicated.
CLINICAL AND PROGNOSTIC VALUE
The clinical significance of IE is mainly determined by its type and gradation, the severity of symptoms, the nature of the underlying illness, the stage of heart disease and the functional state of the myocardium.
Schlunoch's extrasystoles, especially without a structural disturbance of the heart, are not dangerous for life. They are detected during ECG HM in most practically healthy individuals of all age groups, and in 10% the stench is polytopic and rarely group. Zagalom SH does not necessarily indicate a concomitant cardiac pathology, and in the absence of cardiac disease is not a predictor of progression of illness and mortality. On the other hand, in patients with severe structural disorders of the heart and myocardial dysfunction, especially against the backdrop of post-infarction cardiosclerosis or heart failure, frequent heart failure is detected and is an additional prognostic factor.
Ectopic activity of the scutulae is detected in 75–90% of patients with acute myocardial infarction in the first 72 years of illness and results in a high frequency of RSS at this time, but does not correlate with mortality over time. u. The presence of illness at a later stage indicates an unfavorable prognosis. Thus, the frequency of IE less than 1 per year is observed in 50% of patients upon discharge from the hospital and indicates a mortality rate of approximately 5%. In most cases (1–10 per year), which occurs in 20% of patients, the mortality rate reaches 20%. Short paroxysms of ST occur in 12% of patients, and mortality from all causes falls to 30% during the first period after suffering MI. The emergence of serious cardiac arrhythmias after MI is associated with the presence of recurrent ischemia with metabolic and electrolyte disorders. Important factors that contribute to arrhythmogenesis are HF and stenosing coronary atherosclerosis.
Children and polytopes are affected in 70–90% of patients with HF, and short episodes of HF – in 40–80%. In this type of heart failure, heart rhythm disturbance is an unfavorable prognostic factor, and 33–47% of all deaths in patients with HF occur in RSS. Arrhythmogenic factors in HF include dysfunction of the left ventricle (EF < 45%), myocardial ischemia, hypoxia, electrolyte disorders, as well as arrhythmogenic effects of congested therapeutic drugs, especially cardiac glycosides, etc. Iuretics and peripheral vasodilators.
The frequency of SE in patients with dilated cardiomyopathy is very high. Thus, frequent and polytopic SH are observed in 80–90% of patients, short episodes of SH are observed in 20–60%. The frequency of RCC is 10% per year and accounts for half of all deaths. In approximately 50% of patients, anterior extrasystoles are detected. The formation of arrhythmias is associated with the presence of severe dysfunction of LS and HF.
Scholastic extrasystoles are recorded in 50–65% of patients with hypertrophic cardiomyopathy with obstruction of the outflow tract of the left cord, including in 32% of patients, and in 14–25% of paroxysms of pharyngitis. The frequency of RCC in these patients is 2.5–9% per river. The atrial extrasystole occurs earlier, lower than the cardiac rhythm. Causes and factors that contribute to arrhythmogenesis: cellular disorganization in different sections of the myocardium, hypoxia, hypokalemia, obstruction of the outflow tract of the left ventricle, diastolic dysfunction of the left ventricle, heart failure, arrhythmogen no infusion of drugs, intense physical exercise.
The risk of RSS due to sulcus rhythm disturbances especially increases in patients with arrhythmogenic dysplasia of the right sac, congenital or inborn QT syndrome, valvular heart disease (including mitral valve prolapse), arterial hypertension єyu.
The level of concern associated with the ECG can be seen in the following specific features of the ECG. As a matter of fact, there are no dangerous extrasystoles with the configuration of the blockade of the left leg of the His bundle and the vertical position of the electrical axis transmitted to the QRS complex (Rosenbaum type) or if the QRS complex of extrasystoles in all thoracic abductions is superior and predicts the graphic for Wolff-Parkinson-White syndrome type A (type Wolf). The QRS complex of such extrasystoles does not have additional splitting, its amplitude becomes 20 mm or more, duration can be up to 0.12 s, and the ST segment and asymmetrical T wave are straightened discordantly to the main tooth of the socket complex. Septal cords with narrow QRS complexes are more often seen in young people due to structural heart disease and are rarely symptomatic. Potziyno groomed, the marshmallow vinike on the fountains of the structural Uzhennnya Cherzi, the form of the block of law of the bunch of Gis, the amplitudu is not the amplitud complex of the QRS (often up to 10 mm) Сdodatki rodsheshchelni, and the triviality of the yogo is more than 0.12–0.14 s. Anomalies of repolarization may be observed: horizontal depression of the ST segment and concordant straightening of the symmetrical, constricted T wave.
CLASSIFICATIONS OF SLUNOCHKOV'S EXTRASYSTOLES
According to the recommendations of the Association of Cardiologists of Ukraine, created on the basis of the International Classification of Diseases X review, the following types of extrasystoles are seen: atrial, atrioventricular, scapular (one by one - up to 30 per year, often - 30 or more per year, arrhythmia, polymorphic, paired, early - type “R to T”).
In Ukraine, when interpreting HM ECG data in patients with sutular rhythm disorders, the classification of B. Lown and M. Wolf (1971) is traditionally used. Based on this classification, there are 5 classes of extrasystoles: 1) monomorphic, < 30 per year; 2) monomorphic, > 30 per year; 3) polymorphic; 4) pairing (4a) and running of ventral tachycardia (4b); 5) early (“R to T”). This classification was developed to systematize heart rhythm disturbances in patients with acute myocardial infarction, but does not meet the needs of stratification of risk and choice of tactics for differential treatment in post-infarction patients ientiv. The reported variants of sulcular disturbances in the cardiac rhythm of the image according to the classification of R. Myerburg (1984), which can be easily recognized when interpreting the results of the ECG HM (Table 3). It is clear that when stratifying the risk in post-infarction patients, it is already about 10 per year. Before arrhythmias of “high gradations”, protect against paroxysms of any kind. Moreover, persistent CT, regardless of the clinical symptoms and the nature of structural heart disease, is seen as a malignant disruption of the rhythm, so the prognostic value of unstable CT lies heavily behind the underlying disease of the heart and function central state of the myocardium. The morphological type of CT also signifies the essential features of the mechanisms of guilt and tactics for managing the sick, sedation, stagnation of AAP and catheter methods of debridement.
Table 3. Systematization of heart rate disturbances according to R. Myerburg (1984)
| Number of extrasystoles | Forms of shunt arrhythmias | Morphology of shunt tachycardias | ||
| Level of severity | Quantity | Level of severity | Characteristics | |
| 0 | No | 0 | No | •Monomorphic •Polymorphic • “Feasting” • From the outflow tract of the right sac •Double-straightened |
| 1 | Rarely (<1 per year.) | 1 | Alone, monomorphic | |
| 2 | Infrequently (2–9 per year.) | 2 | Alone, polymorphic | |
| 3 | Promizhna (10–29 per year.) | 3 | Guys, jogging (2 or 3–5 complexes) | |
| 4 | Often (30–59 per year.) | 4 | Unstable schular tachycardia (6 complexes up to 29 s) | |
| 5 | Very often (≥ 60 per year.) | 5 | Stable tachycardia (≥ 30 s) | |
A well-known prognostic classification of sac arrhythmias was established by JT Bigger (1993), which divides sac arrhythmias into harmless (benign) and unsafe for life (malignant, lethal) and potentially unsafe (potentially lethal).
- Harmless (benign) arrhythmias - be it any kind (rare, frequent, polytopic, young), as well as short episodes of ST for the presence of cardiac pathology, which do not cause hemodynamic impairment . The prognosis for cirrhosis is the same as for a healthy population. There is no indication for antiarrhythmic therapy.
- Unsafe for life (malignant) sculular arrhythmias are episodes of ST that lead to disruption of hemodynamics or fibrillation of the sacs (FS). These arrhythmias, as a rule, are avoided in patients with manifestations of structural disorders of the heart (ICS, persistent HF, cardiomyopathies, heart failure) and impaired speed of heart rate. In these patients, SHE is only part of the spectrum of shlunochkovyh disturbances to the rhythm. They often also show instability and stability.
- Potentially unsafe (potentially malignant) ventricular arrhythmias - frequent, polytopic, partial, short episodes of cardiac arrest in patients with structural heart disorders (ICS, HF, cardiomyopathies, di heart), so as not to disrupt the rhythm until changes in hemodynamics occur. A marker of greater prevalence of life-threatening cardiac arrhythmias in these patients is systolic dysfunction of the heart valve (LV EF <45%).
PRINCIPLES OF ILLNESS MANAGEMENT
Tactics for treating sick people who are suffering from: a) structural heart disease; b) the frequency of extrasystoles, the presence of group extrasystoles or concomitant paroxysms of tachyarrhythmia; c) clinical symptoms associated with arrhythmia. Indications for the use of β-blockers and/or other AAPs are the following clinical situations: 1) progressive progression of heart disease with a significant increase in blood count; 2). 3) arrhythmia (bi-, tri-, quadrigeminia), short runs of ST, which are accompanied by signs of CH; 4) against the background of illness, which is accompanied by an increased risk of life-threatening arrhythmias (mitral valve prolapse, low QT syndrome, etc.); 5) guilt or increase in the frequency of attacks of angina or acute myocardial infarction; 6) saving the SH after an attack of ST and FS; 7) extrasystoles against the background of abnormal conduction patterns (Wolf-Parkinson-White and Clerk-Levy-Kristesko syndromes).
Patients with good health will not require special antiarrhythmic therapy, but dynamic caution is necessary, because in some of them, according to the Framingham investigation, they may be the onset of cardiac disease. In case of extrasystole in a young age without a structural stress of the heart, especially one that appears at the hour of physical exertion, AAP is absolutely not prescribed. In case of subjective intolerance to extrasystole, rational psychotherapy, sedatives, tranquilizers or antidepressants are indicated. The effectiveness of treatment depends on medical indications and varies over three days up to 2–3 months. When a persistent sedative and antiarrhythmic effect is achieved, the dose of the drug over a skin period of 6–7 days is changed by one third to the full dose. As extrasystole occurs against the background of autonomic dysfunction with signs of sympathoadrenal activation, indications of β-blockers, and with dominant vascular-insular symptoms - M-cholinergic drugs (atropine, beladonium preparations, etrop ). Sicknesses with diseases of the internal organs and extrasystole will first require adequate treatment of the underlying disease. In all types of colds, it is aimed at identifying and reducing potential provoking factors of extrasystoles (such as caffeine intake, life situations), as well as accompanying disorders (arterial hypertension).
In case of single monofocal cerebral palsy in patients with cardiac-vascular diseases without impairment of hemodynamics and coronary blood flow, there is no need to prescribe AAP. The approach to the recognition of AAP is that the risk of side effects with drug treatment of “benign” arrhythmias is greater, and the results of treatment are less positive. The management of such patients requires treatment for the underlying illness, as well as the use of sedatives and psychotherapy methods for subjective intolerance to arrhythmia.
Potentially malignant splanchnic arrhythmias often occur against the background of structural heart disease, for example, ICHS or after a history of myocardial infarction. In such patients, in different gradations, there is a danger of further paroxysms of pharyngitis, tremors or fibrillation of the sac. However, patients with potentially malignant splanchnic arrhythmias will require adequate treatment of the underlying illness. This involves the correction of standard risk factors for ICHS (arterial hypertension, chicken, hypercholesterolemia, celiac diabetes). irin, β-blockers, statins) and for heart failure (ACE inhibitors, β-blockers , aldosterone antagonists). In case of established cardiac pathology, often in high grades, obtain adequate antiarrhythmic therapy. The drugs of choice are most often β-blockers, especially for the presence of additional indications: IHS, arterial hypertension, sinus tachycardia. The high effectiveness of these drugs is associated with their antianginal, antiarrhythmic and bradycardic action. If necessary, beta-blockers can be used with class I AAPs (propafenone, ethmozin, etacizin, disopyramide) to ensure their effectiveness.
The hypothesis about the preventive effectiveness of class I AAP in ES in preventing rapto-related death was revised after the results of the CAST study (1989) were published. The use of flecainide and encainide in post-infarction patients with asymptomatic high grades was associated with a significant increase in the risk of raptic death compared with placebo. The phenomenon is believed to be associated with the arrhythmogenic and negative inotropic action of class I AAP. At the same time, the negative evidence from the CAST study and other studies on the effectiveness of the AAP class I do not exclude the possibility of their effective non-invasive treatment for the treatment of ICH in patients with ICD, as well as for other causes of stenosis. arrhythmia.
If β-blockers and class I AAPs are insufficiently effective, amiodarone is prescribed - the most potent antiarrhythmic agent with the lowest level of arrhythmogenic effects. Amiodarone stagnates in case of resistance to other AAPs; In addition, it is the drug of choice in patients with life-threatening and clinically manifested arrhythmias against the background of severe structural heart disease. Encouraging results were obtained with amiodarone in patients with frequent cervical cancer after suffering from myocardial infarction in a meta-analysis of ATMA (1997). In groups of patients who were treated with amiodarone, the prevalence of RCC did not change significantly, but there was no significant change in overall mortality. Amiodarone is the drug of choice for the treatment of ventricular arrhythmias and their use in patients with systolic myocardial dysfunction and HF. Vicristan amiodarone in small doses (200 mg per dose) allows you to minimize the number of non-cardiac side effects. An alternative way to treat patients with splanchnic arrhythmias against the background of IHS is sotalol, a class III AAP with β-blocking agents.
The high effectiveness of amiodarone and sotalol in the treatment of patients with malignant splanchnic arrhythmias does not indicate the existence of safety problems for these patients. Class III AAP will correct the QT interval, and it is safe to set the interval to 440–460 ms. If indicators of the Q-T interval exceed the indicated limits, prolonged QT interval syndrome is diagnosed. A characteristic and specific manifestation of this is the polymorphic CT (pyrating tachycardia), which can be transformed in FS. The risk of developing arrhythmogenic effects with sotalol is greatest in the first three days of taking the drug. The arrhythmogenic effects of sotalol are avoided more often than with amiodarone.
BAGS
Slunochkova extrasystole is the most widespread in clinical practice of heart rhythm disturbances. You may suffer from a large number of cardiac and extracardial illnesses, which can be a common finding in otherwise healthy individuals. A set of current instrumental and laboratory methods for treating patients with directives to identify the causes and mechanisms, quantity and gradation, clinical and prognostic significance, and stratification. this riziku. A comprehensive strategy for the management of sick patients from the neck, sedation, and the effectiveness of arrhythmias with additional anti-arrhythmias are indicated in advance as a result of the development of the potential cortex, treatment for the reduction of arrhythmias, an improvement in the prognosis. annuity and the risk of arrhythmogenic and other side effects of therapy.
RECOMMENDED LITERATURE
- Outpatient ECG monitoring. Current technologies, diagnostic capabilities, indications: Method. Pos_bnik / Bobrov V. O., Zharinov O. Y., Kuts V. O. and spivat. - Lviv: Medicine of the World, 2004. - 68 p.
- Bobrov V. O., Zharinov O. I. Schlunchar arrhythmias (mechanisms of development, influx of myocardial dysfunction, prognostic assessment, differential therapy). - Lviv, 1995. - 122 p.
- Dabrowski A., Dabrowski B., Piotrovich R. Daily ECG monitoring. - M.: Medpraktika, 2000. - 208 p.
- Investigation of heart rate variability in cardiological practice: Method. rec. / Bobrov V. O., Chubuchny V. M., Zharinov O. Y. and spivat. - K: Ukrmedpatentinform, 1999. - 25 p.
- Kushakovsky M. S. Cardiac arrhythmias. - St. Petersburg: IKF “Foliant”, 1998. - 640 p.
- Orlov V.N. Guide to electrocardiography. - M.: Medical Information Agency, 2003. - 526 p.
- Risk stratification and prevention of cardiac death: Method. rec. / Bobrov V. O., Zharinov O. Y., Sichov O. S. and spivat. - K: Ukrmedpatentinform, 2002. — 39 p.
- Functional diagnostics in cardiology / Ed. L. A. Bockeria, E. Z. Golukhova, A. V. Ivanitsky. - M.: Publishing house NTsSSKh im. A. N. Bakuleva RAMS, 2002. - T. 1 - 427 p., t. 2 - 296 p.
Symptoms
With supraventricular extrasystole, the patient feels “interruptions” in the work of the heart. A healthy person does not feel his own heartbeat at all. Other symptoms include:
- weakness;
- dizziness;
- dyspnea;
- constant feeling of anxiety;
- feeling of lack of air;
- panic;
- fear of dying.
The exact signs of the pathological condition will depend on the underlying disease. For example, with neurosis and vegetative-vascular dystonia, the patient's sweating increases and the feeling of anxiety increases. If the cause of the disease is cardiac pathology, then heart pain is observed.
Consequences and complications
With timely detection of pathology, adequate therapy and lifestyle changes, the prognosis for supraventricular extrasystole is favorable. If the patient does not have concomitant illnesses, death from extrasystole cannot occur. But if the clinical picture is ignored and treatment is refused, the following complications may develop - coronary heart disease, atrial fibrillation and other life-threatening diseases.
Important! Despite the fact that supraventricular extrasystole, as an independent pathology, does not pose a threat, consultation with a doctor should be mandatory.
LiveJournal
Features in children
If a child has been diagnosed with supraventricular extrasystole, then you should first of all monitor his lifestyle and follow a daily routine. It is important to explain to the child that if he does not follow all preventive measures, serious complications may arise that will negatively affect his health.
The child's diet should be varied and balanced. Food should be rich in amino acids, vitamins, proteins, fats, carbohydrates and minerals. The diet should include fruits, vegetables, dairy products, fish and meat. You should minimize the consumption of sweets and junk food.
In order to prevent further development of the pathological condition, it is necessary for the child to have rational physical activity and spend as much time as possible in the fresh air. The baby's condition may worsen due to a cold or infectious disease.
Important! If the child’s condition worsens, you should immediately contact a pediatrician or cardiologist. In some cases, hospitalization is required.
Treatment
How to change your lifestyle?
If extrasystole of the supraventricular type occurs, you should especially carefully monitor your daily routine. For adults, this means that it is recommended to have a normal work schedule and work no more than 8 hours a day. Stress, psycho-emotional stress, and night work should be excluded.
It is necessary to give up bad habits. The body must have proper rest, so you need to sleep at least 8 hours, and it is recommended to spend your rest time as actively as possible.
To prevent the condition from worsening, the patient should review his diet. It is recommended to exclude foods high in cholesterol and animal fats from the diet. The basis of the diet is plant foods, dietary meat, nuts and dried fruits. Oils that are especially useful are sunflower, olive and flaxseed.
Drug therapy
Treatment of ventricular extrasystole begins with drug therapy - drugs are selected depending on the presence of additional disorders, the degree of deviation from the normal heart rhythm and the type of cardiac pathology. Therapeutic effect of antiarrhythmic drugs:
- prevention of the occurrence of organic systolic murmurs;
- decreased conductivity levels in the heart;
- decreased force of myocardial contractions;
- normalization of heart rate.
To monitor the effectiveness and correctness of therapy, an ECG is prescribed. This procedure allows you to see all the changes in the body, which gives the doctor the opportunity to timely adjust the course of treatment.
Antiarrhythmic drugs can cause problems with the respiratory system. Therefore, treatment should only be carried out under the supervision of a specialist. To minimize the risk of complications, the doctor periodically performs urine and blood tests. This is necessary in order to establish the concentration of medicinal substances in the patient’s body.
Surgery
Surgical treatment is prescribed only if conservative therapy has failed. To eliminate extrasystole of the supraventricular type, radiofrequency catheter ablation .
This procedure involves inserting a catheter through an artery. The doctor guides the electrodes through the catheter directly to the parts of the heart from which the impulse comes. This is a closed type of operation, sometimes open surgery is performed.
Open surgery is prescribed if there is a need for intervention in other parts of the heart.
The essence of surgical intervention for supraventricular extrasystole is to eliminate the focus, which generates additional cardiac impulses.