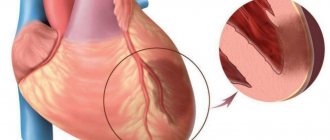
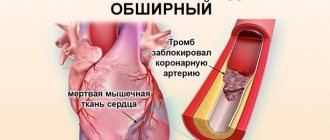
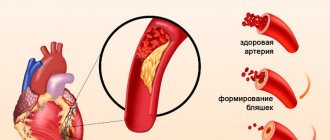
The main and most common cause of myocardial infarction is a violation of blood flow in the coronary arteries, which supply the heart muscle with blood and, accordingly, oxygen. Most often, this disorder occurs against the background of atherosclerosis of the arteries, in which atherosclerotic plaques form on the walls of blood vessels. These plaques narrow the lumen of the coronary arteries and can also contribute to the destruction of vessel walls, which creates additional conditions for the formation of blood clots and arterial stenosis.
Risk factors for myocardial infarction
The main risk factor for myocardial infarction is atherosclerosis of the coronary arteries.
There are a number of factors that significantly increase the risk of developing this acute condition:
- Atherosclerosis. A disorder of lipid metabolism, in which the formation of atherosclerotic plaques on the walls of blood vessels occurs, is the main risk factor in the development of myocardial infarction.
- Age. The risk of developing the disease increases after 45–50 years of age.
- Floor. According to statistics, this acute condition occurs 1.5–2 times more often in women than in men; the risk of developing myocardial infarction is especially high in women during menopause.
- Arterial hypertension. People suffering from hypertension have an increased risk of cardiovascular accidents, since elevated blood pressure increases the myocardial oxygen demand.
- Previous myocardial infarction, even small focal ones.
- Smoking. This harmful habit leads to disruption of the functioning of many organs and systems of our body. With chronic nicotine intoxication, the coronary arteries narrow, which leads to insufficient oxygen supply to the myocardium. Moreover, we are talking not only about active smoking, but also passive smoking.
- Obesity and physical inactivity. If fat metabolism is disrupted, the development of atherosclerosis and arterial hypertension accelerates, and the risk of diabetes mellitus increases. Insufficient physical activity also negatively affects the body's metabolism, being one of the reasons for the accumulation of excess body weight.
- Diabetes. Patients suffering from diabetes have a high risk of developing myocardial infarction, since elevated blood glucose levels have a detrimental effect on the walls of blood vessels and hemoglobin, impairing its transport function (oxygen transfer).
Symptoms of myocardial infarction
This acute condition has quite specific symptoms, and they are usually so pronounced that they cannot go unnoticed. However, it should be remembered that atypical forms of this disease also occur.
In the vast majority of cases, patients experience a typical painful form of myocardial infarction, thanks to which the doctor has the opportunity to correctly diagnose the disease and immediately begin its treatment.
The main symptom of the disease is severe pain. The pain that occurs during myocardial infarction is localized behind the sternum, it is burning, dagger-like, and some patients characterize it as “tearing.” The pain can radiate to the left arm, lower jaw, and interscapular area. The occurrence of this symptom is not always preceded by physical activity; pain often occurs at rest or at night. The described characteristics of the pain syndrome are similar to those during an attack of angina, however, they have clear differences.
Unlike an attack of angina, pain during myocardial infarction persists for more than 30 minutes and is not relieved by rest or repeated administration of nitroglycerin. It should be noted that even in cases where a painful attack lasts more than 15 minutes, and the measures taken are ineffective, it is necessary to immediately call an ambulance team.
Atypical forms of myocardial infarction
Myocardial infarction occurring in an atypical form can cause difficulties for a doctor when making a diagnosis.
Gastritis variant. The pain syndrome that occurs with this form of the disease resembles pain during exacerbation of gastritis and is localized in the epigastric region. On examination, tension in the muscles of the anterior abdominal wall may be observed. Typically, this form of myocardial infarction occurs when the lower parts of the left ventricle, which are adjacent to the diaphragm, are affected.
Asthmatic variant. Reminds me of a severe attack of bronchial asthma. The patient experiences suffocation, cough with foamy sputum (but can also be dry), while the typical pain syndrome is absent or mildly expressed. In severe cases, pulmonary edema may develop. Upon examination, cardiac arrhythmias, decreased blood pressure, and wheezing in the lungs may be detected. Most often, the asthmatic form of the disease occurs with repeated myocardial infarctions, as well as against the background of severe cardiosclerosis.
Arrhythmic option. This form of myocardial infarction manifests itself in the form of various arrhythmias (extrasystole, atrial fibrillation or paroxysmal tachycardia) or atrioventricular block of varying degrees. Due to heart rhythm disturbances, the picture of myocardial infarction on the electrocardiogram may be masked.
Cerebral option. Characterized by impaired blood circulation in the vessels of the brain. Patients may complain of dizziness, headache, nausea and vomiting, weakness in the limbs, and consciousness may be confused.
Painless option (erased form). This form of myocardial infarction causes the greatest difficulties in diagnosis. Pain syndrome may be completely absent; patients complain of vague chest discomfort and increased sweating. Most often, this erased form of the disease develops in patients with diabetes and is very difficult.
Sometimes the clinical picture of myocardial infarction may contain symptoms of different variants of the disease; the prognosis in such cases, unfortunately, is unfavorable.
Localization of infarction with ST elevation
Changes in cardiograms during a heart attack with ST segment elevation vary depending on which part of the heart the heart attack develops in. The location of the infarction can be determined by the ECG leads in which ST elevation is recorded and in which leads reciprocal ST depression appears. In this regard, remember which leads correspond to different parts of the myocardium. Look at diagram 6.
Scheme 6. Correspondence of cardiogram leads to different areas of the myocardium.
Schema source.
Diagram 7 below shows the location of large coronary arteries, the occlusion of which can lead to transmural infarction with appropriate localization.
Scheme 7. Large coronary arteries
| Localization of infarction | ST elevation leads | Leads with reciprocal ST depression |
| Interventricular septum | V1-V2 | |
| Front wall | V3-V4 | |
| Lateral wall of the left ventricle | I, aVL, V5-V6 | III, aVF |
| Bottom wall | II, III, aVF | I, aVL |
| Back wall | V7-V9 | V1-V3 (and high R in V1-V3) |
| Right ventricle | V1, III, II (STIII > STII), V3R - V5R | V2 |
The table above shows which leads show ST elevation or depression depending on the location of STEMI. In practice, ST elevation infarction usually affects more than one area. For example, an infarction of the interventricular septum is usually combined with an infarction of the anterior wall of the left ventricle. In this case, ST elevation will be not only in leads V1-V2, but also in V3-V4.
Let's consider STEMI options with different localizations.
Interventricular septal infarction
As mentioned above, isolated septal infarction is a rare occurrence (usually septal and anterior wall infarction). Septal infarction develops as a result of occlusion of the left anterior descending artery (LAD). The cardiogram records ST elevation in leads V1-V2.
Scheme 8. Infarction of the interventricular septum
ECG 2. Myocardial infarction of the interventricular septum
ECG source.
On ECG 2, an infarction of the interventricular septum is indicated by pathological Q waves in leads V1-V2 and moderate ST elevation in the same leads. Judging by the ST height and the presence of Q waves, this is a subacute stage of infarction. In addition, in this case there is diffuse ST segment depression in leads I, II, V4-V6 in combination with ST elevation in aVR. This indicates subendocardial myocardial ischemia.
Left ventricular lateral wall infarction
Left ventricular lateral wall infarction with ST elevation, as discussed above, is usually associated with anterior wall infarction. In addition, it can be combined with infarction of the lower or posterior wall. It develops as a result of occlusion of the left anterior descending artery (LAD) and/or the circumflex coronary artery (LCX).
Isolated lateral wall infarction is less common and is associated with occlusion of the small branches of the LAD or the marginal branch of the LCX.
Scheme 10. Infarction of the lateral wall of the left ventricle
On the cardiogram with a lateral wall infarction, ST elevation is recorded in leads I, aVL, V5-V6. If ST elevation is only in leads I, aVL, but not in leads V5-V6, they speak of a high lateral infarction. A reciprocal decrease occurs in leads III, aVF.
Examples of lateral wall infarction combined with anterior wall infarction were shown above (see ECG 3-5).
ECG 6. High lateral left ventricular infarction
ECG source.
ECG 6 shows ST elevation in leads I and aVL, as well as reciprocal depression in leads III, aVF. There is no ST elevation in leads V5-V6. These are signs of high lateral left ventricular infarction.
Posterior wall infarction
An infarction of the posterior wall, as a rule, develops in combination with an infarction of the lower or lateral wall of the left ventricle. Isolated posterior wall infarction occurs in no more than 10% of cases. However, isolated posterior wall infarction is not always recognized in a timely manner, since it develops infrequently and there is no ST segment elevation on a standard 12-lead cardiogram. To confirm this diagnosis, it is necessary to use additional posterior leads: V7-V9. Posterior wall infarction can be suspected from a 12-lead ECG based on the following signs:
- ST segment depression in leads V1-V3. This ST depression is reciprocal to ST elevation in the accessory posterior leads (V7-V9).
- Tall and usually widened R waves in leads V1-V3.
- The R/S ratio in V2 is greater than 1.
- Positive T wave in leads V1-V3.
ECG 8. Infarction of the posterior and inferior wall of the left ventricle with ST elevation
ECG source.
On ECG 8, ST segment depression, as well as a tall and wide R wave in leads V2-V3, indicate infarction in the posterior wall of the left ventricle. To confirm this diagnosis, a cardiogram was recorded using additional leads V7-V9, where ST elevation was recorded. In addition, in leads III, aVF, slight elevation of the ST segment was also recorded, which indicates involvement of the lower wall of the left ventricle in the process.
ECG 9. Infarction with ST elevation of the lateral and posterior wall of the left ventricle
ECG source.
On ECG 9, ST elevation in leads I, aVL, V5-V6 and reciprocal ST depression in leads III, aVF reflect infarction of the lateral wall of the left ventricle. In addition, there is a decrease in ST in leads V1-V3, which, in combination with high R waves in these same leads, may indicate posterior wall damage. Thus, in this case there is an infarction of the lateral and posterior wall of the left ventricle. To confirm posterior wall infarction, an ECG should be recorded in additional posterior leads (V7-V9).
Treatment
All efforts of doctors are aimed at removing the clot and restoring normal blood flow. If therapeutic methods do not produce results, they resort to the services of a cardiac surgeon. The main thing is to help the patient as quickly as possible. This significantly increases the chances of rescue and recovery.
Warning: Undefined array key “module” in /customers/0/e/9/germanklinik.de/httpd.www/control/config/inc/templates_c/front^7198fc69815638cccb44869b7c86cae91ff823b0_0.file.DefaultGK.tpl.php on line 488 Warning: Attempt to read property “value” on NULL in /customers/0/e/9/germanklinik.de/httpd.www/control/config/inc/templates_c/front^7198fc69815638cccb44869b7c86cae91ff823b0_0.file.DefaultGK.tpl.php on line 488 Warning : Undefined array key “extension” in /customers/0/e/9/germanklinik.de/httpd.www/control/config/inc/templates_c/front^7198fc69815638cccb44869b7c86cae91ff823b0_0.file.DefaultGK.tpl.php on line 490 Warning: Attempt to read property “value” on NULL in /customers/0/e/9/germanklinik.de/httpd.www/control/config/inc/templates_c/front^7198fc69815638cccb44869b7c86cae91ff823b0_0.file.DefaultGK.tpl.php on line 490
Thank you! We have received your request for consultation.
If you want to fill out a Request for Treatment, continue filling out. Having all the necessary data, we will be able to find the best solution to your problem in the shortest possible time
Anterior wall infarction
ST elevation infarction in the anterior wall region develops as a result of occlusion of the left anterior descending artery (LAD). The cardiogram records ST elevation in leads V3-V4. A reciprocal decrease in ST occurs in the inferior leads: III, aVF. Subsequently, pathological Q is formed in V3-V4.
Scheme 9. Infarction of the anterior wall
An infarction of the anterior wall, as a rule, is not isolated and is most often combined with an infarction of the interventricular septum and/or an infarction of the lateral wall of the left ventricle. This is determined by the fact that the interventricular septum and lateral wall are also supplied by the left anterior descending artery (LAD).
ECG 3. Infarction of the septum, anterior wall and partly the lateral wall of the left ventricle
ECG source.
On ECG 3, ST elevation in leads V1-V4, as well as deep Q waves in V1-V2, indicate infarction in the area of the interventricular septum (ST elevation in V1-V2) and the anterior wall of the left ventricle (ST elevation in V3-V4). There are tall coronary T waves in V2-V4. There is also slight ST elevation in leads I, aVL and V5, which may indicate extension of the infarction to the lateral wall of the left ventricle.
There is a reciprocal decrease in ST in lead III. These are signs of the acute phase of myocardial infarction with ST elevation.
ECG 4. Infarction of the anterior and lateral walls of the left ventricle
ECG source.
On ECG 4 there is ST elevation in leads V2-V6, I, aVL. Elevation in V3-V4 with maximum elevation in V3 indicates an infarction of the anterior wall, and ST elevation V5-V6, I, aVL indicates an infarction of the lateral wall of the left ventricle. In III and aVF there is reciprocal ST depression.
ECG 5. Extensive infarction of the interventricular septum, anterior and lateral walls of the left ventricle. “Tombstoning” pattern
ECG 5 shows massive ST segment elevation in leads V1-V6, I, aVL, reciprocal ST decrease in leads III and aVF. This morphological pattern on the cardiogram is called the “tombstoning” pattern and indicates occlusion of the proximal LAD. A prognostically unfavorable option with a high probability of damage to a large part of the myocardium with a sharp decrease in cardiac contractility and the development of cardiogenic shock.
How does an atypical heart attack occur?
In addition to the usual course of the disease, which occurs in most cases, medicine also knows atypical variants of pathogenesis. For example, such as:
- Asthmatic. Typical for older people, the pain syndrome is mild, but the heartbeat is rapid, shortness of breath is observed, and the pulse is increased;
- Gastralgic. With this option, there is pain in the upper abdomen, belching, hiccups, vomiting are observed, and the abdomen is swollen. ;
- Arrhythmic. The heartbeat is abnormal, but the pain is minor. The percentage of patients with arrhythmic infarction is up to 5%;
- Cerebrovascular is characterized by a person’s disorientation in space, loss of consciousness and vomiting occur;
- Asymptomatic - practically does not make itself felt. As a rule, it is discovered when a patient is prescribed an ECG for preventive purposes.
However, doctors warn that only the first, most acute period is atypical. Then the disease takes its toll and the picture will be the same as with the normal course of a heart attack.