Infarction-pneumonia is an inflammation that occurs after a local persistent disturbance of blood circulation in the lung tissue. The main cause of this phenomenon is considered to be thromboembolism of the branches of the pulmonary artery. When massively spread, it leads to instant death. When small branches are affected, only local infarctions of the pulmonary parenchyma are observed.
First symptoms
A pulmonary infarction does not manifest itself immediately. For the first two to three days after a vessel is blocked, a person may not be aware of the problems. Many people confuse the first symptoms with the discomfort that occurs with angina pectoris. Sometimes pain is possible, as with an acute abdomen. You should be alert to the following symptoms:
- acute chest pain;
- increased pain when coughing, rapid breathing, bending the body;
- shortness of breath that occurs out of the blue, without physical activity;
- when coughing, blood is coughed up (not in everyone, in about half of the cases), complete pulmonary hemorrhage rarely occurs;
- the nasolabial triangle and fingers of the limbs become bluish;
- cold sticky sweat during painful attacks;
- hiccups;
- general malaise, possible fever;
- Some patients vomit.
People suffering from thrombophlebitis and thrombosis, pulmonary hypertension, and frequent relapses of pulmonary embolism are predisposed to pulmonary infarction. Risk factors include age over 60 years, excess weight, pregnancy and childbirth (or caesarean section).
2. Reasons
The direct cause of pulmonary ischemia leading to a heart attack in 15-25% of cases is pulmonary embolism (PE). In this case, the mortality rate, taking into account the insufficient specificity of the observed clinical manifestations and the complexity of intravital diagnosis of pulmonary embolism, can reach 30%.
The pathological basis is a wide range of cardiovascular diseases, including myocardial infarction, infectious carditis, vasculitis, as well as thrombophlebitis of the deep veins of the lower extremities and pelvis.
In addition, pulmonary embolism can develop as a result of complicated childbirth, fractures, and various surgical interventions.
Risk factors are considered to be old age, a hereditary predisposition to thrombosis, taking certain medications (in particular, hormone-containing contraceptives), excess body weight, hypertension and symptomatic hypertension, malignant tumor processes, and some diseases of the hematopoietic system.
Visit our Thoracic Surgery page
Why is a pulmonary infarction dangerous?
When a large artery is blocked, the patient's condition quickly deteriorates. Pain and fever intensify, panic attacks appear, and attacks of suffocation occur. If a person is not taken to the hospital, he will face serious consequences, including death.
If there is a problem with a small or medium vessel, the pathological condition develops more slowly, and at first the symptoms are not pronounced. But if treatment is left untreated, complications arise:
- post-infarction pneumonia is associated with congestion in those parts of the lung where the blood supply has been disrupted;
- lung abscess - an advanced stage of the infectious process, purulent melting of tissue, subsequently - the formation of a cavity in the lung;
- necrosis of affected tissues due to developing ischemia and cessation of nutrition of a part of the organ.
3. Symptoms and diagnosis
Pulmonary infarction does not have a distinct specificity that allows “diagnosis at a glance.” It is known, however, that the patient’s condition most often deteriorates suddenly or quite quickly. Most patients note sharp chest pain, which can easily be mistaken for angina pectoris, an increase in body temperature to subfebrile values (in the case of reactive post-infarction pneumonia, the temperature can reach 39°C or more), unexplained shortness of breath, increased breathing and pulse, cyanotic pallor of the skin, arrhythmic symptoms, a sharp decrease in blood pressure, nausea, vomiting, diarrhea.
In severe cases, these symptoms can take the form of vascular collapse, acute abdomen, atrial fibrillation, disorders of higher nervous activity, including hemorrhagic stroke, cerebral edema and coma. From a third to half of patients note hemoptysis, which, with malignant dynamics, can transform into pulmonary hemorrhage, which, however, is rare. Infection of a necrotic focus can result in gangrene, lung abscess, and sepsis.
As shown above, the clinical picture of pulmonary infarction is very polymorphic and, at the same time, not very specific, therefore, only a detailed analysis of clinical manifestations in comparison with the results of objective studies allows us to suspect the true cause and exclude symptomatically similar conditions. Of the instrumental methods, the most important are ECG, various, especially angiographic modifications of contrast-enhanced radiography, as well as MSCT, ultrasound examinations of the heart and great vessels in Doppler mode, and lung scintigraphy. A battery of laboratory tests is prescribed.
About our clinic Chistye Prudy metro station Medintercom page!
How to diagnose
If a pulmonary infarction is suspected, the patient is examined by a pulmonologist and a cardiologist. At the first stage, the doctor interviews the patient and listens to him using a phonendoscope. Small wheezing, pleural flapping noise, systolic murmurs and other specific signs should alert you. The patient experiences rapid breathing, and palpation of the abdominal area reveals an enlarged and painful liver.
An important test is an x-ray of the lungs. Photographs are taken in frontal and lateral projections, effusion in the pleural cavity, deformation and expansion of the lung root are detected. The state of pulmonary circulation is assessed using angiopulmonography - x-ray with contrast injected into the arteries.
To complete the clinical picture, it is necessary to take a general blood test and undergo an ECG. The patient may also be sent for Doppler ultrasound of the lower extremities to assess the condition of the veins and the presence of thrombosis.
Treatment of heart attack-pneumonia
If the cause of pneumonia after a pulmonary infarction is thromboembolic complications, then therapy begins with fibrinolytic agents and anticoagulants.
Symptomatic treatment involves reducing pain by taking analgesics. Etiotropic treatment involves a course of antibiotics depending on the nature of the pathogen. The principle of therapy after myocardial infarction is based on the use of steroid hormones, which contribute to the rapid improvement of general well-being.
Only an experienced doctor can prescribe treatment, based on the results of the studies obtained, and taking into account the individual characteristics of each patient’s body. Pulmonologists, cardiologists, therapists, neurologists and other doctors at the Yusupov Hospital always prescribe a course of treatment for their patients on an individual basis. In this case, the general condition of the patient, age factor, the presence of concomitant diseases and much more are taken into account. Doctors at the Yusupov Hospital are putting back on their feet even those patients who were abandoned in other medical centers.
You can make an appointment with a doctor at the Yusupov Hospital by phone and by filling out the feedback form on the website.
Treatment and prevention
To eliminate pain, the patient is prescribed non-narcotic (less often narcotic) analgesics. Coagulants are used to prevent further thrombosis. And to stimulate the dissolution of already formed blood clots - streptokinase and urokinase, tissue plasminogen activator.
If there is a suspicion of post-infarction pneumonia, antibiotics are prescribed. The drugs are prescribed orally and in the form of droppers. In cases where conservative treatment does not give the expected effect, surgical intervention is indicated - pulmonary embolectomy.
To avoid problems in the future, it is recommended not to start and treat thrombophlebitis in a timely manner. Since pulmonary infarction in the vast majority of cases develops precisely against their background. Therefore, for prevention it is necessary:
- wear compression stockings;
- do therapeutic exercises;
- Visit a phlebologist regularly if you are prone to varicose veins and thrombosis.
If you experience symptoms of a pulmonary infarction, consult your doctor immediately. At the medical center you will receive a consultation with a pulmonologist. If necessary, you will be examined by a surgeon and a cardiologist. At the clinic you will also be tested and undergo the necessary examinations. If therapy is started in a timely manner, the prognosis is favorable.
1.General information
According to the definitions existing in modern medicine, a heart attack is a rapid, one-stage focal necrosis (death, death) of a large number of parenchymal, i.e. the main, functionally specialized cells of any tissue or organ. The cause is ischemia, a pathological state of oxygen and trophic starvation due to a lack of blood supply. Outside of medicine, the most famous example of such a scenario is myocardial infarction, while in clinical practice, infarctions of the spleen, brain (stroke), kidneys and other organs are also encountered.
Due to the peculiarities of the anatomical structure and vasculature (blood supply) of the organs of the human respiratory system, pulmonary infarction in most cases develops on the right side and in the lower lobes.
A must read! Help with treatment and hospitalization!
How to treat pulmonary infarction
Treatment of pulmonary infarction in children and adults involves the use of:
- non-narcotic or narcotic analgesics for pain relief;
- direct (Frakiparin, Heparin) and indirect coagulants to prevent further thrombus formation (coagulants are contraindicated in cases of bleeding, duodenal/gastric ulcers, hemorrhagic diathesis, malignant tumors);
- fibrinolytic therapy with Urokinase, Streptokinase or tissue plasminogen activator to dissolve existing blood clots.
If a pulmonary infarction is complicated by arterial hypertension, vasopressors (Dopamine, Norepinephrine), Reopoliglucin are administered intravenously. At the first symptoms of heart attack-pneumonia, antibiotics are prescribed. Also, patients with pulmonary embolism require oxygen inhalation through a special nasal catheter.
If conservative treatment does not provide improvement in well-being, thromboembolectomy is performed from the pulmonary artery - a vena cava filter is installed in the inferior vena cava system.
Causes of pulmonary infarction
Most often, pulmonary infarction develops in people who suffer from diseases of the cardiovascular system:
- mitral stenosis;
- atrial fibrillation;
- coronary heart disease;
- myocardial infarction;
- infective endocarditis;
- cardiomyopathy;
- vasculitis;
- heart failure;
- atrial maxomas, etc.
In this case, blood clots form in the appendage of the right atrium and are carried with the blood flow into the arteries of the pulmonary circle.
Also, the causes of pulmonary infarction can be:
- thrombophlebitis of the deep pelvic veins;
- thrombosis of leg veins.
In these two diseases, floating thrombi that are attached to the distal part of the venous vessel are dangerous.
Other causes of pulmonary embolism include:
- fracture of tubular bones, due to which the patient is forced to remain in bed for a long time;
- caesarean section, natural childbirth;
- extensive thoracic, abdominal and gynecological operations;
- hemorrhoidectomy.
The risk of pulmonary infarction is high in people over 60 years of age, as well as in:
- recurrent venous thrombosis;
- hereditary burden of pulmonary embolism;
- taking hormonal contraceptives;
- the presence of a pancreatic tumor;
- obesity;
- pulmonary hypertension.
Dangerous background pathologies are considered:
- DIC syndrome;
- sickle cell anemia;
- polycythemia;
- heparin-induced thrombocytopenia.
Myocardial infarction (heart attack) - symptoms and treatment
A patient with an acute heart attack must be promptly transported to the hospital to prevent complications and increase the chances of survival. The system of care for patients with myocardial infarction includes the following stages:
- Pre-hospital stage. Ambulance teams provide assistance and transport the patient to the hospital.
- Hospital stage. Help is provided in specialized vascular departments.
- Rehabilitation stage. Rehabilitation is carried out in special departments of hospitals or specialized cardiological sanatoriums.
- Dispensary observation and outpatient treatment. Clinical examination in the post-infarction period is carried out in regional or city cardiology centers or in cardiology offices of clinics [6].
At the prehospital stage, the following tasks are solved:
- an accurate diagnosis is established. If this fails, it is permissible to establish a tentative syndromic diagnosis as soon as possible;
- The patient is given a nitroglycerin tablet under the tongue (or use a nitro-containing spray) and 0.25-0.35 g of aspirin;
- pain is relieved by administering painkillers;
- acute circulatory failure and heart rhythm disturbances are eliminated;
- the patient is brought out of the state of cardiogenic shock;
- in case of clinical death, resuscitation measures are performed;
- transport the patient to the hospital as soon as possible.
Further therapy is determined by the stage (period) of myocardial infarction. In the acute and very acute period, the goal of treatment is to prevent an increase in the focus of myocardial necrosis, eliminate pain and other symptoms. It is important to restore blood flow through the heart arteries and relieve pain. The intensity of pain during this period is so great that the patient may die due to cardiac arrest. It is necessary to prevent severe complications. When the disease passes into the subacute stage and in the post-infarction period, the goal of therapy is to reduce the risk of attack recurrence and possible complications.
For the treatment of acute myocardial infarction, drugs from various pharmacological groups are used:
Painkillers. Analgesics from the group of narcotic painkillers (morphine, promedol, omnopon) in combination with analgin, antihistamines (diphenhydramine). Neuroleptanalgesia is most effective when a combination of the analgesic fentanyl with the strong antipsychotic droperidol is used. The effectiveness of these drugs is noticeable within a few minutes. Not only pain disappears, but also fear of death, unmotivated anxiety and psychomotor agitation. Tranquilizers (diazepam) can be used to relieve psychomotor agitation. To reduce hypoxia (decreased oxygen in tissues), oxygen inhalation is used using a nasal catheter.
Thrombolytic therapy. It is important to restore blood flow and dissolve blood clots so that the death of the heart muscle does not spread further. The smaller the area of necrosis, the higher the patient’s chances of successful rehabilitation and the lower the risk of life-threatening complications. Immediate use of drugs (preferably within the first hour after an attack) allows you to achieve maximum effectiveness of treatment. A time limit of three hours is allowed. To dissolve a blood clot, thrombolytic drugs are administered intravenously, for example, streptokinase, urokinase, alteplase. The dose depends on the patient's weight.
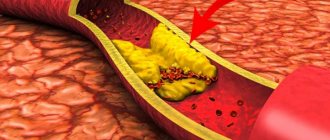
Restoration of coronary blood flow is also possible with the help of surgical treatment - stenting or coronary artery bypass grafting. A balloon catheter is inserted into a narrow section of the artery under fluoroscopic guidance. In this case, the atherosclerotic plaque is “crushed”, and the lumen of the heart artery increases. Then a stent (metal frame) can be installed into the lumen of the vessel.
Antiplatelet agents. Drugs from this group affect blood cells (platelets and red blood cells). The action of antiplatelet agents prevents platelet aggregation, improving blood flow. The main drug used is aspirin (acetylsalicylic acid). Contraindications to the use of aspirin: bleeding from the gastrointestinal tract, exacerbation of gastric or duodenal ulcers.
P2Y12 platelet receptor inhibitors are also used , which block platelet activation. The main blockers are ticagrelor, prasugrel and clopidogrel.
Intravenous/subcutaneous anticoagulants. , unfractionated heparin intravenously, is used to prevent deep vein thrombosis (DVT) and pulmonary embolism (PE) . Enoxaparin , which is also used to prevent venous thromboembolism, is administered subcutaneously.
To limit the area of myocardial ischemia and necrosis, it is necessary, in addition to restoring blood flow in the arteries of the heart, to reduce the hemodynamic load on the heart. Nitrates and beta blockers are used for this purpose.
Nitrates. They have an analgesic effect, reduce myocardial oxygen demand, increase coronary and collateral (bypass) blood flow, reduce the load on the heart muscle, and limit the size of the myocardial lesion. Their combination with beta blockers is especially effective, leading to rapid positive ECG dynamics and reducing the risk of sudden death [10].
Beta-blockers have an antiarrhythmic effect. The purpose of using beta-blockers (propranolol, metoprolol, atenolol) is to reduce the frequency and force of heart contractions, which will help reduce the load on the heart and the myocardial oxygen demand. Beta blockers continue to be used indefinitely in the absence of side effects and contraindications [1].