Development mechanism
At the time of the development of an acute infarction, a sharp disruption of the blood supply to the myocardium occurs for the following reasons:
- Rupture of an atherosclerotic plaque under the influence of a sharp jump in pressure, increased heart rate and acceleration, and accelerated blood flow through the coronary vessels.
- Blockage of blood vessels due to blood thickening (acceleration of platelet aggregation, activation of the coagulation system, decreased rate of blood clot lysis).
- Spasm of the coronary artery (vasoconstriction).
I often observed patients in whom several factors were identified as the cause of the disease with myocardial damage. In young patients, vasospasm is often the basis of pathological disorders, which is not possible to determine after the start of treatment.
Expert advice
I strongly recommend starting treatment in a hospital immediately after an acute attack, since only in this case is it possible to limit the further spread of necrosis and minimize irreversible changes in the myocardium.
The study of histological samples confirms the destruction of the cardiac myocyte 20 minutes after the development of ischemia. After 2-3 hours of lack of oxygen, their glycogen reserves are depleted, which marks their irreversible death. Replacement of myocarditis with granulation tissue occurs within 1-2 months.
As my practice and the observations of colleagues show, the scar on the heart is finally consolidated after six months from the moment the first symptoms of acute infarction appear and is a section of coarse collagen fibers.
Classification
Heart scars can be classified according to their location and extent of distribution.
They can be located along the coronary vessels:
- Impairment of blood flow in the anterior interventricular artery leads to ischemia with the subsequent appearance of a scar in the area of the septum between the ventricles, involving the papillae and lateral wall, as well as on the anterior surface and apex of the left ventricle.
- The infero-posterior and lateral part is affected when the left circumflex coronary artery is blocked.
- Problems with the blood supply to the myocardium in the right artery results in irreversible changes in the right ventricle and can affect the posterior inferior part of the left ventricle and the septum. But such a violation is extremely rare.
According to the type of distribution, scars can be local (focal), which can be compared to a scar on the body, or diffuse (multiple). Experts call the second option dystrophic changes in the myocardium.
How does a scar manifest itself?
The acute period of a heart attack is characterized by a variety of clinical manifestations. The main symptom is pain, which can be relieved exclusively with narcotic analgesics and can be observed from an hour to 2-3 days. Then the pain syndrome disappears and the formation of an area of necrosis begins, which takes another 2-3 days. Then comes a period of replacing the affected area with loose connective tissue fibers.
If the correct treatment tactics are used, the following symptoms are noted:
- development of compensatory hypertrophy;
- rhythm disturbance (which often accompanies the acute period) is eliminated;
- tolerance to stress gradually increases.
If a scar that appears on the heart crosses the conduction paths along which the impulse travels, a conduction disorder is recorded, such as a complete or partial blockade.
In the case of successful recovery after a primary small-focal infarction, I did not notice any significant disturbances associated with the functioning of the heart in my patients.
If patients have formed a large scar or many small ones, the following deviations are observed:
- dyspnea;
- increased heart rate;
- the appearance of edema;
- enlargement of the left chambers of the heart;
- pressure fluctuations.
Symptoms of pericarditis in adults
Pericarditis can feel like a heart attack with sudden, sharp or stabbing pain in the chest.
The pain may be in the middle or left part of the chest, behind the breastbone, and may spread to the shoulders, neck, arms or jaw. Other symptoms may include:
- temperature;
- dry cough;
- weakness or fatigue;
- difficulty breathing, especially when lying down;
- cardiopalmus;
- swelling of the feet, legs and ankles.
Symptoms that occur may worsen if the patient lies down, takes deep breaths, coughs, eats, or drinks.
But if he sits leaning forward, it gets better. If the cause of pericarditis is a bacterial infection, the patient may have fever, chills, and a higher than normal white blood cell count. If the cause is viral, there may be flu-like symptoms or stomach upset.
In any case, if chest pain appears (it happens in 85 - 90% of cases), you should immediately call an ambulance.
How dangerous is this?
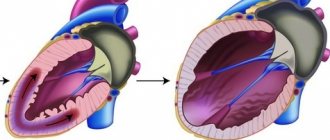
The most dangerous is the development of a scar as a result of large-focal or transmural infarctions, as well as several repeated violations in different basins of the coronary vessels with diffuse multiple lesions.
In the case of a large area of damage or widespread cardiosclerosis, the remaining healthy cells cannot fully compensate for the work of damaged cardiomyocytes. The frequency and strength of contractions increases in order to provide organs and tissues with oxygen and necessary substances.
As a result, tachycardia develops; with its appearance, the load on the heart becomes even greater, which leads to dilatation of the left ventricle and atrium. As it progresses, blood stagnation appears in the right side with the development of heart failure.
I also observed another type of complication: a scar on the heart after a heart attack with extensive and deep damage to all layers of the organ caused the formation of an aneurysm due to the thinning of its wall.
The reasons for the appearance of such a defect are:
- transmural lesion;
- increased blood pressure;
- increased blood pressure inside the ventricle;
- excessive physical activity of the patient, refusal to comply with the regimen.
An aneurysm leads to the rapid development of heart failure, the formation of a parietal thrombus, and pronounced stagnation in the systemic circulation. Often complicated by severe rhythm disturbances leading to death (paroxysmal tachycardia and ventricular fibrillation).
Heart attacks are no joke
Prolonged chest pain is a serious reason to consult a doctor
Heart attack is a word with a scary connotation. We often think of it as something far away. Something that happens to others, but will never happen to you or those close to you. Unfortunately, this detachment and unwillingness to delve into the essence of the problem can sometimes be fatal.
Heart disease is the main reason why Ugra residents die or become disabled. Unfortunately, not everyone knows its symptoms and does not contact doctors at the right time.
Chest pain is serious
Myocardial infarction is an emergency condition most often caused by coronary artery thrombosis. Most often it affects people suffering from a lack of physical activity against the background of psycho-emotional overload. But it can also affect people with good physical fitness, even young people. Although the likelihood of developing a heart attack in people leading a sedentary lifestyle is several times greater than in people who are physically active. Most often, myocardial infarction occurs in men aged 45 to 65 years and women over 55 years of age.
The main reasons contributing to the occurrence of myocardial infarction are: overeating, unhealthy diet, excess animal fats in food, insufficient physical activity, hypertension, bad habits.
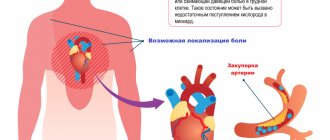
The heart is often thought of as a pump that pumps blood through itself. But the heart muscle itself is supplied with oxygen through blood vessels that approach it from the outside. As a result of various reasons, some part of these vessels is affected by atherosclerosis and can no longer pass enough blood. Coronary heart disease occurs. During a myocardial infarction, the blood supply to part of the heart muscle stops suddenly and completely due to complete blockage of the coronary artery. This is usually caused by the development of a blood clot on an atherosclerotic plaque, or less commonly by a spasm of the coronary artery. A section of the heart muscle that is deprived of nutrition dies.
“Symptoms of myocardial infarction are pressing, squeezing or burning pain behind the sternum, which can radiate under the shoulder blade, into the left arm, into the left shoulder, into the epigastric region (pain in the pit of the stomach) and even into the lower jaw.
Heart pain radiates through the plexus of nerve endings to the lower jaw. It feels like absolutely all the teeth in the lower jaw are hurting. There may also be numbness in the left arm. If this pain lasts longer than twenty minutes, then this indicates that the person has a prolonged anginal attack and the development of myocardial infarction is possible,” says Maria FRANZ , a cardiologist of the first qualification category of the cardiac surgery department of the District Clinical Hospital of Khanty-Mansiysk.
To the ambulance - without hesitation!
In addition to pain, a person may feel short of breath, experience weakness and sweating. If the heart does not have enough oxygen, this means that the vessel is clogged, blood does not flow into the heart muscle, and therefore the contractility of the heart muscle decreases. The amount of oxygenated blood decreases. As a result, a person feels as if he is short of air.
With the symptoms of a heart attack, if you feel them for the first time in your life, the main thing is not to panic. You need to chew 250 milligrams of aspirin - that's half a tablet. Place nitroglycerin under your tongue or take Isoket. Next, call an ambulance immediately!
At the Khanty-Mansiysk Regional Clinical Hospital, the patient immediately undergoes emergency coronary angiography - an examination of the blood vessels of the heart. The patient goes from the emergency room to the X-ray surgery department, where doctors look at the patency of the coronary arteries, looking for blood clots that close the vessels of the heart, interfering with normal blood flow.
Next, doctors perform coronary angioplasty to restore normal blood circulation. The prognosis after such an intervention is usually favorable: a heart attack is certainly not a death sentence or a disability. “The sooner we start working with the patient, the better for him and his health. It will be possible to avoid many complications caused by a heart attack. And soon there is a very high probability of returning to normal life,” says the cardiologist.
"Golden" 90 minutes
If you feel symptoms similar to those voiced in this article, call an ambulance without hesitation! It’s better to make a mistake than to suffer a heart attack on your feet.
In Khanty-Mansiysk, about 150-160 heart attacks occur per year. Unfortunately, some patients do not call an ambulance, thinking that the cause of the pain is, say, heartburn. The fact is that the heart is located close to the stomach; they are separated only by the diaphragm. If a heart attack develops along the back wall of the heart, the one that is directed towards the stomach, then the person will experience pain in the stomach during a heart attack. Pain impulses from the heart travel to the spinal cord and then to the head. Due to the close proximity of the heart and stomach, the brain often cannot distinguish which of these two organs the pain signal comes from.
But the time from the moment a symptom occurs to the moment medical care is provided is very important. “Often a patient comes to our cardiac surgery department who has already had a heart attack. We see this with electrocardiography. We see scars - zones of impaired contractility of the heart. In this case, the patient does not even know that he suffered a heart attack. But this does not mean at all that everything has passed without a trace for the body: The consequence may be a decrease in cardiac contractility and the development of heart failure. Or an aneurysm of the left ventricle of the heart, which requires more complex intervention. And there are situations when medicine is powerless - the consequences are so serious, says Maria Franz.
From the time the patient reaches the doctors until normal blood flow in the coronary artery is restored by medical means, no more than 90 minutes should pass. Ideally, a person should get to the hospital within the first hour, which doctors call the “golden hour.” The sooner the necessary measures are taken, the less damage will be caused to health, and the smaller the area affected by a heart attack. In other cases, it is possible to help the patient so quickly that a heart attack may not develop, doctors say.
Take care of your heart
In conclusion, I would just like to remind you that health is a priceless gift that should be valued and protected. Doing this is not so difficult, and with the advent of the habit of a healthy lifestyle, taking care of your body will begin to bring joy. Don’t “deprive” yourself of physical activity, eat right, give up cigarettes. And smile more often: a positive emotional attitude can also be safely attributed to the prevention of cardiovascular diseases.
Ilya Yurukin,
public relations editor
article from the site https://cmphmao.ru/node/30146
Diagnostics
In order to establish a diagnosis, I conduct a survey and study the medical history (mainly, it includes ischemic heart disease with a history of heart attack). External examination usually reveals increased respiratory rate, weakening of heart sounds during auscultation, the presence of edema, and various rhythm disturbances. I will definitely take a blood pressure measurement.
Then I send you to the following research:
- general and biochemical blood test, coagulogram (will help establish concomitant diseases, cholesterol levels and clotting time);
- EchoCG or ultrasound of the heart helps to establish the presence of localized or diffuse areas of connective tissue, allows you to clarify the location and extent of distribution;
- MRI helps to visualize and reliably assess the affected area;
- scintigraphy is required to determine dysfunctional areas of the myocardium.
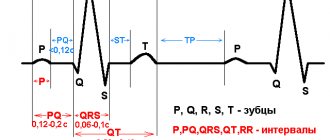
With the help of an ECG after a transmural and large-focal infarction, it is possible to clarify where the scar is located on the diseased heart.
It is determined by the presence of a Q wave in different leads, as can be seen in the table.
| ECG leads | Localization of post-infarction scar in the left ventricle |
| V1-V3 | Anterior wall with septal involvement |
| V3-V4 | Anterior wall and apex |
| I, aVL, V5-6 | Anterolateral sections |
| I, aVL, V1-6 | Entire front wall |
| II, III, aVF | Posterior wall and diaphragmatic region |
| V7-8 | Posterobasal area |
The increase in the T wave and ST segment, which are characteristic of the acute period, is no longer observed. ST returns to the isoline, T decreases. With a small area and depth of the lesion, no signs of a scar remain; it is leveled, since the function of conductivity and contractility is taken over by neighboring cells. A nonspecific manifestation of dystrophic changes can be a smoothed or moderately negative T wave.
Diagnosis and treatment
If you or your loved ones are experiencing the symptoms described above, we recommend getting tested. During diagnosis, the doctor monitors heart parameters at rest and during exercise.
The patient is prescribed:
- daily ECG monitoring,
- echocardiography (ECHO-CG),
- chest x-ray,
- CT and MRI using special equipment that allows you to examine the heart virtually between beats.
Such diagnostics are carried out not only during the initial examination of patients with suspected disease, but also in dispensary groups of patients with an already confirmed diagnosis.
Depending on the diagnostic results, the doctor prescribes the necessary treatment: therapy or surgery.
- Therapy is aimed at preventing, preventing and alleviating relapses of the disease that became the root cause of the defect, as well as treating heart failure.
- Surgical intervention is an extreme necessity, which due to age or complications may not be prescribed for all patients.
Typically, heart valve disease is a mechanical problem that can only be solved with surgery performed by a surgeon. For stenosis, an operation is indicated to separate the fused valve leaflets and widen the atrioventricular opening - commissurotomy. If there is insufficiency, prosthetics are performed: replacement with a biological or mechanical analogue.
Treatment
Treatment of dystrophic changes includes the use of medications, diet, and lifestyle changes.
Drug therapy
The choice of medications for the appearance of scars depends on the person’s condition.
Typically, after a heart attack and the formation of scar tissue, the following groups of drugs are used:
- statins to lower cholesterol levels (Atorvostatin, Rosuvastatin);
- Beta blockers and ACE inhibitors (Bisoprolol, Ramipril) help reduce the load on the LV and increase its resistance to ischemia
- diuretics allow you to remove swelling and relieve the systemic circulation (Indapamide, Torasemide).
Surgical intervention
When the scar causes complete blockade of the conduction system, treatment consists of installing a pacemaker (pacemaker). An operation (coronary artery bypass surgery) allows you to restore blood flow, when a section of a damaged coronary artery is replaced by another vessel.
In cases of severe degenerative processes and the development of heart failure incompatible with life, an organ transplant is required.
Traditional methods
It is impossible to treat cardiosclerosis and scar changes in the myocardium using traditional methods. They only slightly alleviate a person’s condition, complementing general therapy. However, neither mumiyo nor celandine, as the “healers” write, are capable of ridding the patient of a scar, much less restoring the functioning of the heart.
Causes and symptoms
Heart valve defects can be congenital or acquired. The main causes of the development of heart valve defects are rheumatism, infections, myocardial and cardiovascular diseases.
Congenital heart valve defects develop before birth and depend on how the pregnancy progressed. Congenital heart valve defects are an extremely rare diagnosis, diagnosed only in 1% of cases. Congenital defects include defects of the aortic and pulmonary valves, which are treated by surgical intervention in the first years of the patient’s life.
Purchased . Acquired heart valve defects include transformations of the valve structure due to infections, inflammation, previous heart attacks, etc. Most of them arise as a result of a gradual change in the structure of the heart; in some cases, rheumatism leads to the defect. All congenital and acquired defects have related symptoms that can appear at any age:
- increased heart rate,
- dyspnea,
- swelling,
- other manifestations of heart failure.
Initially, they appear during physical activity, but as pathologies develop, they will begin to appear in a calm state. Among the types of heart valve defects, mitral valve prolapse is the most common. It occurs during heart contractions when the valve leaflets in the left atrium sag. The walls of the valve lose elasticity and it “leaks”. Prolapse can be primary or secondary:
- Primary prolapse refers to congenital valve defects. Connective tissue pathologies in this case are a genetic predisposition.
- Secondary prolapse is an acquired defect. It occurs due to chest injury, rheumatism or myocardial infarction.
Prolapse does not have serious health consequences, and its symptoms do not interfere with life. However, they may not appear for a long time and most often bother people in old age, which is why they are written off as “age-related.” If you do not pay attention to the symptoms in time, complications may arise, such as arrhythmia and heart failure.
Symptoms also include complaints of pain in the heart area. They arise against the background of anxiety, are not associated with physical activity and are not relieved with medication. The pain is not intense, but long-lasting, accompanied by anxiety and rapid heartbeat.
Diet
The diet after a heart attack and scar formation depends on the degree of damage to the heart muscle.
General nutritional requirements are:
- maximum salt restriction;
- reducing fluid consumption (up to 1.5 liters);
- eliminating foods high in cholesterol;
- mandatory use of products with potassium;
- if you are overweight, you should reduce the total number of calories;
- Avoid caffeinated drinks completely.
It should be noted that currently there are no effective ways to completely get rid of a heart scar. Repeated attempts to restore tissue using stem cells have so far been unsuccessful.
Preventing heart disease during coronavirus
The health and life expectancy of a person directly depends on the state of the cardiovascular system. To prevent heart and vascular diseases, you will need a set of measures related to a responsible attitude towards your body.
Basic preventive measures:
- undergo preventive examinations at the clinic in a timely manner;
- adhere to a balanced diet, consume more fruits and vegetables, reduce the amount of animal fats;
- maintain water and drinking regime;
- pay attention to physical activity;
- spend more time in the fresh air;
- stop drinking alcohol, smoking, and taking drugs; avoid stressful situations;
- control pressure in arterial vessels;
- If symptoms of cardiac or vascular dysfunction develop, make a timely appointment with a cardiologist.
Case from practice
A patient came to me for a consultation with complaints of shortness of breath, fatigue, and swelling in the ankles.
History of large-focal myocardial infarction. On examination, the skin is pale and pasty (mild swelling) of the legs. Auscultation - heart sounds are slightly muffled. Blood pressure is within the age norm (130 to 75 mm Hg). The ECG shows signs of dystrophic changes in the posterior wall of the LV, post-infarction scar in the anteroseptal region. After examination, a moderate change in the myocardium and mild hypertrophy of the left ventricle were discovered. A biochemical blood test showed an elevated level of low-density cholesterol.
Diagnosis: IHD. Post-infarction cardiosclerosis, heart failure I. Received treatment with beta blockers, prescribed Aspirin Cardio in a minimal dosage, and a diuretic. She recommended lifelong use of statins (Atorvastatin) under the control of cholesterol levels. She prescribed a diet with a low amount of salt, limiting fluid to 1.5 liters per day, stopping smoking and drinking alcohol. After 2 weeks of treatment, pastiness is not detected, shortness of breath has decreased, and exercise tolerance has increased.