Hypertension is a common companion of women during pregnancy, when metabolic processes in the body intensify and intra-abdominal pressure increases. High blood pressure in pregnant women threatens to develop serious consequences, including premature birth, miscarriage, and even death. Therefore, it is important to have an idea of which antihypertensive drugs are most effective during pregnancy, whether concomitant treatment is necessary, and many other features of hypertension in women during this wonderful and crucial period.
Therapists at the Yusupov Hospital will help you choose a drug for the treatment of hypertension that is both highly effective and has minimal side effects.
Indications for use
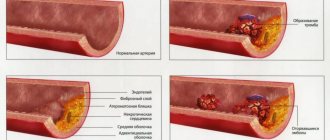
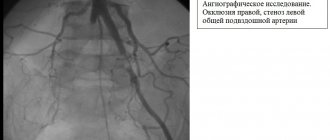
Peripheral vasodilator drugs are indicated for circulatory disorders in peripheral organs and tissues associated with narrowing of the lumen of the vessel: atherosclerotic plaque (vascular atherosclerosis obliterans), inflamed vascular wall (endarteritis obliterans), pathological reflex spasm (Raynaud's disease).
Peripheral vasodilators are used for circulatory disorders in the vessels of the lower extremities, which are accompanied by intermittent claudication, trophic ulcers, pain in the legs at rest, sensory disturbances, and spasms in the calf muscles.
Peripheral vasodilators are also used for vascular complications due to diabetes mellitus (diabetic angiopathy), up to the initial stages of gangrene of the foot.
In addition, drugs of peripheral vasodilators are used for chronic disorders of cerebral circulation - cerebral atherosclerosis, dyscirculatory encephalopathy, chronic cerebral vascular insufficiency.
Peripheral vasodilators are indicated for behavioral and mental disorders in old age, in patients after stroke, coma, and insufficient blood supply to the retina and inner ear.
Certain drugs of peripheral vasodilators (bendazole and its combinations with papaverine) are used for arterial hypertension and hypertensive crisis.
Arterial hypertension in pregnant women: diagnosis, management tactics and treatment approaches
Arterial hypertension (AH) occurs in 4–8% of pregnant women [6, 7, 8]. Hypertension includes a whole spectrum of different clinical and pathogenetic conditions: hypertension, symptomatic hypertension (renal, endocrine), preeclampsia. According to WHO, hypertensive syndrome is the second cause of maternal mortality after embolism [20, 31], accounting for 20–30% of cases in the structure of maternal mortality [1, 7]. Rates of perinatal mortality (30–100 0/00) and preterm birth (10–12%) in pregnant women with chronic hypertension significantly exceed the corresponding rates in pregnant women without hypertension [8]. Hypertension increases the risk of abruption of a normally located placenta and can cause cerebrovascular accidents, retinal detachment, eclampsia, and massive coagulopathic bleeding as a result of placental abruption [7, 20].
Until recently, hypertension was thought to occur relatively rarely in people under 30 years of age. However, in recent years, population surveys have revealed elevated blood pressure (BP) in 23.1% of people aged 17–29 years [2]. At the same time, the early appearance of hypertension is one of the factors responsible for the unfavorable prognosis of the disease in the future [9]. An important fact is that the frequency of identifying patients with hypertension based on visits is significantly lower than during mass surveys of the population. This is due to the fact that a significant proportion of people, mainly with early stages of the disease, feel well and do not visit a doctor. This, apparently, to a certain extent explains the fact that many women find out that they have high blood pressure only during pregnancy, which significantly complicates the diagnosis and treatment of such patients.
The physiological characteristics of the cardiovascular system, depending on the developing pregnancy, sometimes create a situation where it is difficult to distinguish physiological changes from pathological ones.
Hemodynamic changes during physiological pregnancy represent an adaptation to the coexistence of mother and fetus, they are reversible and are due to the following reasons [7, 10]:
- strengthening metabolic processes aimed at ensuring the normal functioning of the fetus;
- an increase in circulating blood volume (CBV);
- the appearance of an additional placental circulatory system;
- gradual increase in body weight of the pregnant woman;
- an increase in the size of the uterus and limited mobility of the diaphragm;
- increased intra-abdominal pressure;
- changes in the position of the heart in the chest;
- an increase in the blood levels of estrogens, progesterone, and prostaglandins E.
Physiological hypervolemia is one of the main mechanisms ensuring the maintenance of optimal microcirculation (oxygen transport) in the placenta and such vital organs of the mother as the heart, brain and kidneys. In addition, hypervolemia allows some pregnant women to lose up to 30–35% of their blood volume during labor without developing severe hypotension. Blood plasma volume in pregnant women increases from about the 10th week, then increases rapidly (until about the 34th week), after which the increase continues, but more slowly. The volume of erythrocytes increases at the same time, but to a lesser extent than the volume of plasma. Since the percentage increase in plasma volume exceeds the increase in red blood cell volume, so-called physiological anemia of pregnancy occurs, on the one hand, and hypervolemic dilution, leading to a decrease in blood viscosity, on the other.
By the time of birth, blood viscosity reaches normal levels.
Systemic blood pressure in healthy women changes slightly. During a normal pregnancy, systolic blood pressure (SBP) and diastolic blood pressure (DBP), as a rule, decrease in the second trimester by 5–15 mmHg. Art. The reasons for these changes are the formation of placental blood circulation during these periods of pregnancy and the vasodilating effect of a number of hormones, including progesterone and prostaglandins E, which cause a drop in total peripheral vascular resistance (TPVR).
During pregnancy, physiological tachycardia is observed. The heart rate (HR) reaches its maximum in the third trimester of pregnancy, when it is 15–20 beats/min higher than the heart rate of a non-pregnant woman. Thus, the normal heart rate in late pregnancy is 80–95 beats/min, and it is the same for both sleeping and waking women.
It is now known that cardiac output (CV) increases by approximately 1–1.5 L per minute mainly during the first 10 weeks of pregnancy and reaches an average of 6–7 L per minute by the end of the 20th week. Towards the end of pregnancy, MOS begins to decline.
During a physiologically proceeding pregnancy, a significant decrease in peripheral vascular resistance occurs, which is associated with the formation of the uterine circulatory system with low resistance, as well as with the vasodilating effect of estrogens and progesterone. A decrease in peripheral vascular resistance, as well as a decrease in blood viscosity, facilitates hemocirculation and reduces afterload on the heart.
Thus, the individual blood pressure level in pregnant women is determined by the interaction of the main factors:
- a decrease in peripheral vascular resistance and blood viscosity aimed at reducing blood pressure;
- an increase in BCC and MOS, aimed at increasing blood pressure.
If the balance between these groups of factors is disturbed, blood pressure in pregnant women ceases to be consistently normal.
Classification of hypertension
Hypertension in pregnant women is a heterogeneous concept that unites various clinical and pathogenetic forms of hypertensive conditions in pregnant women.
Currently, the classification is a subject of debate, since there are no uniform criteria and classification signs of hypertension during pregnancy [4, 5], there is no single terminological base (for example, the term is used to denote the same process in Russia and many European countries gestosis, in the USA and Great Britain - preeclampsia, in Japan - toxemia).
More than 100 classifications of hypertensive conditions during pregnancy have been proposed. In particular, the International Classification of Diseases, 10th revision (ICD-10) combines all such pregnancy-related manifestations in the 2nd obstetric block. In Russia, all diseases are encrypted in accordance with this classification, although due to different terminology, encryption in accordance with ICD-10 causes disagreement among specialists.
The Working Group on High Blood Pressure in Pregnancy in 2000 developed a more concise classification of hypertensive conditions during pregnancy [20], which includes the following forms:
- chronic hypertension;
- preeclampsia - eclampsia;
- preeclampsia superimposed on chronic hypertension;
- gestational hypertension: a) transient hypertension in pregnant women (there is no gestosis at the time of birth and the pressure returns to normal by the 12th week after birth (retrospective diagnosis)); b) chronic hypertension (pressure rise after childbirth persists (retrospective diagnosis)).
Chronic hypertension refers to hypertension that was present before pregnancy or diagnosed before the 20th week of gestation. Hypertension is defined as a condition with a SBP equal to or higher than 140 mmHg. Art. and DBP - 90 mm Hg. Art. Hypertension that was first diagnosed during pregnancy but did not disappear after childbirth is also classified as chronic.
Pregnancy-specific preeclampsia syndrome usually occurs after the 20th week of gestation. It is determined by an increased level of blood pressure (gestational rise in blood pressure), accompanied by proteinuria. Gestational hypertension is defined as a SBP above 140 mmHg. Art. and DBP above 90 mm Hg. Art. in women who had normal blood pressure before the 20th week. In this case, proteinuria is considered to be a protein concentration in the urine of 0.3 g per day or higher when analyzing a daily urine sample. The dipstick method can be used to diagnose proteinuria. If it is used, two urine samples must be obtained 4 hours or more apart. For analysis, an average portion of urine or urine obtained through a catheter is used. The sample is considered positive if the amount of albumin in both samples reaches 1 g/l.
Previously, an increase in SBP by 30 and DBP by 15 mmHg. Art. It was recommended to consider it a diagnostic criterion, even if the absolute values of blood pressure are below 140/90 mm Hg. Art. Some authors do not consider this a sufficient criterion, since available data show that the number of adverse outcomes does not increase in women in this group. Nevertheless, most experts call for special attention to be paid to women in this group who have an increase in SBP by 30 and DBP by 15 mmHg. Art., especially in the presence of concomitant proteinuria and hyperuricemia [20].
Diagnostics
According to WHO recommendations, blood pressure should be measured after a 5-minute rest, in a sitting position, on both arms, using a cuff of the appropriate size.
The most common errors when measuring blood pressure include: measuring blood pressure once without prior rest, using an incorrectly sized cuff (“cuff” hyper- or hypotension) and rounding numbers. The measurement should be taken on both hands. The SBP value is determined by the first of two successive auscultatory tones. In the presence of an auscultatory failure, an underestimation of blood pressure may occur. The DBP value is determined by the V phase of Korotkoff sounds. Blood pressure should be measured with an accuracy of 2 mmHg. Art., which is achieved by slowly releasing air from the tonometer cuff. For different values, the true blood pressure is considered higher [4]. It is preferable to take measurements in pregnant women in a sitting position. In the supine position, due to compression of the inferior vena cava, blood pressure values may be distorted.
A single increase in blood pressure ≥ 140/90 mm Hg. Art. is registered in approximately 40–50% of women. It is obvious that a random single measurement of blood pressure to make a diagnosis of hypertension in pregnant women is clearly not enough. In addition, the phenomenon of so-called “white coat hypertension”, i.e. high blood pressure when measured in a medical environment (office blood pressure) in comparison with outpatient (home) measurement, is widely known. In approximately 30% of pregnant women with hypertension registered at a doctor's appointment, daily blood pressure monitoring (ABPM) resulted in normal average daily blood pressure [4]. The question of the prognostic significance of the phenomenon of “white coat hypertension” has not yet been finally resolved. Currently, most researchers believe that it reflects increased reactivity of the vascular wall, which, in turn, potentially increases the risk of cardiovascular disease. The role of ABPM in pregnant women has also not been fully determined. In addition to diagnosing “white coat hypertension” and assessing the effectiveness of therapy for established hypertension, this method can be used to predict the development of preeclampsia. BP usually decreases at night in patients with mild gestosis and chronic hypertension, but in severe gestosis the circadian rhythm of BP may be distorted, with a BP peak at 2 am [16].
However, given the complexity of the technology, the high cost of equipment, as well as the existence of other alternative methods for predicting preeclampsia, it can be considered that ABPM is not included in the group of mandatory (screening) methods for examining pregnant women with high blood pressure. However, it can be successfully used for individual indications.
Antihypertensive therapy for hypertension in pregnant women
Long-term use of antihypertensive drugs in pregnant women with chronic hypertension is a matter of controversy. A decrease in blood pressure may impair uteroplacental blood flow and compromise fetal development [16, 25, 30]. Over the past more than 30 years, seven international studies have been conducted that compared groups of women with mild chronic hypertension in pregnancy using different management regimens (with antihypertensive therapy and without pharmacological correction of hypertension) [11]. Treatment did not reduce the incidence of preeclampsia, preterm birth, placental abruption, or perinatal mortality compared with groups without treatment [20].
Some centers in the United States now maintain close monitoring of women with chronic hypertension who have stopped taking antihypertensive medications [32, 36]. In women with hypertension that has developed over several years, with damage to target organs, and taking large doses of antihypertensive drugs, therapy should be continued [25]. Reports on the experience of monitoring patients with severe chronic hypertension without adequate antihypertensive therapy in the first trimester describe fetal loss in 50% of cases and significant maternal mortality.
Experts from the Working Group on High Blood Pressure in Pregnancy, 2000, consider the following criteria for prescribing treatment: SBP - from 150 to 160 mm Hg. Art., DBP - from 100 to 110 mm Hg. Art. or the presence of target organ damage, such as left ventricular hypertrophy or renal failure [20]. There are other provisions on the criteria for starting antihypertensive therapy: with blood pressure more than 170/110 mm Hg. Art. [15, 24] (at higher blood pressure, the risk of placental abruption increases, regardless of the genesis of hypertension) [18]. There is an opinion that treatment of hypertension at lower values of initial blood pressure “removes” such a significant marker of gestosis as elevated blood pressure. At the same time, normal AH numbers give a picture of false well-being [14, 22]. European recommendations for the diagnosis and treatment of pregnant women with hypertension offer the following tactics for managing pregnant women with various types of hypertension [28].
- Pre-pregnancy hypertension without target organ damage - non-drug therapy for blood pressure 140–149/90–95 mm Hg. Art.
- Gestational hypertension that developed after 28 weeks of gestation - drug therapy at blood pressure 150/95 mm Hg. Art.
- Pre-pregnancy hypertension with target organ damage, pre-pregnancy hypertension with superimposed preeclampsia, pre-eclampsia, gestational hypertension that developed before the 28th week of pregnancy - drug therapy for blood pressure 140/90 mm Hg. Art.
Basic principles of drug therapy for pregnant women: proven effectiveness and proven safety [13].
In Russia there is no classification of drugs according to safety criteria for the fetus. It is possible to use the criteria of the American classification of medicinal and food products Food and Drug Administration (FDA–2002).
FDA classification criteria for drug safety for the fetus (2002):
A - studies in pregnant women have not revealed a risk to the fetus;
B - a risk to the fetus was detected in animals, but not in humans, or there is no risk in the experiment, but there is not enough research in humans;
C—Side effects have been identified in animals, but there is insufficient research in humans. The expected therapeutic effect of the drug may justify its use, despite the potential risk to the fetus;
D - a risk to the fetus has been proven in humans, but the expected benefit from its use for the expectant mother may exceed the potential risk to the fetus;
X is a drug that is dangerous to the fetus, and the negative effects of this drug on the fetus exceed the potential benefits for the expectant mother.
Despite the fact that the range of drugs used in the treatment of hypertension in pregnant women is quite wide (methyldopa, beta blockers, alpha blockers, calcium antagonists, myotropic antispasmodics, diuretics, clonidine), the choice of drug therapy for a pregnant woman is very responsible and complex a matter that requires strict consideration of all the pros and cons of this treatment [32].
Methyldopa
This drug is classified as Class B by the FDA. It is preferred as a first-line treatment by many clinicians based on reports of stability of uteroplacental blood flow and fetal hemodynamics, as well as 7.5 years of follow-up with a limited number of children experiencing no delayed adverse developmental effects following methyldopa administration during pregnancy. their mothers [27].
Benefits of Methyldopa:
- does not worsen uteroplacental blood flow and fetal hemodynamics;
- does not cause delayed adverse effects on the development of children after administration during pregnancy to their mothers;
- reduces perinatal mortality;
- safe for mother and fetus.
Disadvantages of Methyldopa:
- not recommended for use at 16–20 weeks (possible effect on dopamine content in the fetal nervous system);
- intolerance: 22% experience depression, sedation, orthostatic hypotension.
There have been no adequate and strictly controlled studies on other groups of antihypertensive drugs during pregnancy. Even when the results of studies are combined into a meta-analysis, there is no clear evidence of the effectiveness and safety of antihypertensive drugs in pregnancy.
β-blockers
Most of the published literature on antihypertensive therapy in pregnancy comes from studies of the effects of adrenergic blockers, including β-blockers and the α-β blocker labetalol. There is an opinion that β-blockers prescribed in early pregnancy, especially atenolol, can cause fetal growth restriction [19]. However, none of these drugs produced serious side effects; although in order to state this with complete confidence, long-term follow-up is not enough [24, 29].
The advantage of β-blockers is the gradual onset of the hypotensive effect, characterized by a decrease in the frequency of proteinuria, no effect on blood volume, absence of postural hypotension, and a decrease in the frequency of respiratory distress syndrome in the newborn.
The disadvantages of β-blockers are a decrease in the weight of the newborn and placenta due to increased vascular resistance when prescribed in early pregnancy.
In accordance with the FDA classification, atenolol, metoprolol, timolol oxprenolol, propranolol, labetolol belong to class C, pindolol, acebutolol - to class B.
Dadelszen in 2000 conducted a “fresh” meta-analysis of clinical trials on β-blockers and came to very interesting conclusions. Intrauterine growth retardation is not due to the effect of β-blockers, but to a decrease in blood pressure as a result of antihypertensive therapy with any drug. All antihypertensive drugs equally reduced the risk of developing severe hypertension by 2 times compared with placebo. When comparing various antihypertensive drugs with each other, no advantages were found regarding the effect on end points (development of severe hypertension, maternal and perinatal mortality) [30].
α-blockers are used in the treatment of hypertension in pregnant women, but there have been no adequate and well-controlled studies in humans [21]. In limited, uncontrolled use of prazosin and a β-blocker in 44 pregnant women, no adverse effects were observed. The use of prazosin in the third trimester in 8 women with hypertension did not reveal clinical complications after 6–30 months, the children developed normally [3].
The advantages of this group of drugs are as follows:
- effective reduction of blood pressure (used in combination with β-blockers);
- do not affect the bcc;
- absence of adverse effects (based on the results of clinical studies in a small number of women).
Flaws:
- a sharp decrease in blood pressure;
- possible orthostatic reactions;
- lack of adequate and strictly controlled studies in humans.
In accordance with the FDA classification, prazosin and terazosin belong to class C, doxazosin to class B. In our country, according to the instructions of the Pharmaceutical Committee of the Russian Federation, α-blockers are not used for hypertension in pregnant women.
Calcium antagonists. Experience with the use of calcium antagonists is limited to their use mainly in the third trimester of pregnancy. However, a multicenter prospective cohort study on the use of these drugs in the first trimester of pregnancy did not reveal teratogenicity [12]. A recent multicenter randomized trial of slow-release nifedipine in the second trimester found neither positive nor negative effects of the drug when compared with a no-treatment control group [23, 29].
Benefits of calcium antagonists:
- fetal weight in women taking nifedipine is higher than in women taking hydralazine;
- early use reduces the incidence of severe gestosis and other complications in the mother and fetus (however, in a number of studies using nifedipine in the second trimester, neither positive nor negative effects of the drug were detected when compared with a control group that did not receive treatment);
- absence (according to the results of clinical studies) of embryotoxicity in humans;
- antiplatelet effect;
- when used in the first trimester of pregnancy, there are no teratogenic effects (not detected in studies).
Disadvantages of calcium antagonists:
- embryotoxicity of calcium antagonists in animals;
- a rapid decrease in blood pressure can lead to a deterioration in uteroplacental blood flow (therefore, nifedipine is better taken orally than sublingually to relieve a hypertensive crisis in pregnant women);
- side effects: swelling of the legs, nausea, heaviness in the epigastrium, allergic reactions.
According to the FDA classification, nifedipine, amlodipine, felodipine, nifedipine SR, isradipine, diltiazem belong to class C.
Diuretics (hypothiazide 25–100 mg/day). Opinions regarding the use of diuretics during pregnancy are controversial. Doctors' concerns are mostly understandable. It is known that gestosis is associated with a decrease in plasma volume and the prognosis for the fetus is worse in women with chronic hypertension who have not experienced an increase in blood volume. Dehydration may impair uteroplacental circulation.
During treatment, electrolyte disturbances and increased uric acid levels may develop (which means this indicator cannot be used to determine the severity of gestosis) [17]. In women taking diuretics, from the beginning of pregnancy there is no increase in blood volume to normal values. For this reason, due to theoretical concerns, diuretics are not usually prescribed first. A meta-analysis of nine randomized trials involving more than 7000 subjects treated with diuretics found a trend towards a reduction in the development of edema and/or hypertension with a confirmed lack of increase in adverse fetal outcomes. Moreover, if their use is justified, they prove to be safe and effective agents that can significantly potentiate the effect of other antihypertensive drugs, and are not contraindicated during pregnancy, except in cases of decreased uteroplacental blood flow (preeclampsia and intrauterine growth retardation). A number of experts believe that pregnancy is not a contraindication for taking diuretics in women with essential hypertension that preceded conception or manifested before mid-pregnancy. However, there is insufficient data regarding the use of diuretics to lower blood pressure in pregnant women with hypertension.
In accordance with the FDA classification, hypothiazide belongs to class B. However, the instructions of the Pharmaceutical Committee of the Russian Federation state that hypothiazide is contraindicated in the first trimester of pregnancy; in the second and third trimesters it is prescribed according to strict indications.
Clonidine , a central α2-adrenergic agonist, has restrictions for use during pregnancy, and when taken in the postpartum period, breastfeeding should be avoided. The drug has no advantages over β-blockers. Sleep disorders have been identified in children whose mothers received clonidine during pregnancy. When used in early pregnancy, embryotoxicity was detected [4].
Myotropic antispasmodics are currently not used for routine therapy. They are prescribed only in emergency situations - during a hypertensive crisis [18]. Hydralazine (apressin) with long-term use can cause: headache, tachycardia, fluid retention, lupus-like syndrome. Diazoxide (hyperstat) with long-term treatment can cause sodium and water retention in the mother, hypoxia, hyperglycemia, hyperbilirubinemia, thrombocytopenia in the fetus. Sodium nitroprusside can cause cyanide intoxication with long-term use [16].
Angiotensin-converting enzyme (ACE) inhibitors are contraindicated during pregnancy due to the high risk of intrauterine growth retardation, the development of bone dysplasia with impaired ossification of the cranial vault, shortening of the limbs, oligohydramnios (oligohydramnios), neonatal renal failure (renal dysgenesis, acute renal failure in the fetus or newborn ), fetal death [20].
Although no data have been accumulated regarding the use of angiotensin II receptor antagonists, their adverse effects are likely to be similar to those of ACE inhibitors, so these drugs should also be avoided [16].
Treatment of acute severe hypertension in pregnant women
Some experts raise DBP to 105 mm Hg. Art. or higher is considered an indication for starting antihypertensive therapy [20], others consider it possible to abstain from antihypertensive therapy up to 110 mm Hg. Art. [15, 18]. There is evidence that if the initial diastolic blood pressure did not exceed 75 mm Hg. Art., treatment should begin when it rises to 100 mm Hg. Art. [16].
The range of drugs used in the treatment of acute severe hypertension in pregnancy includes hydralazine (start with 5 mg intravenously or 10 mg intramuscularly). If there is insufficient effectiveness, repeat after 20 minutes (from 5 to 10 mg depending on the reaction; when the desired blood pressure levels are achieved, repeat as necessary (usually after 3 hours); if there is no effect from the total dose of 20 mg intravenously or 30 mg intramuscularly, use another drug ); labetalol (start with a dose of 20 mg intravenously; if the effect is insufficient, prescribe 40 mg 10 minutes later and 80 mg every 10 minutes 2 more times, maximum dose - 220 mg; if the desired result is not achieved, prescribe another drug; do not use in women with asthma and heart failure); nifedipine (start with 10 mg per os and repeat after 30 minutes if necessary); sodium nitroprusside (rarely used when there is no effect from the above drugs and/or there are signs of hypertensive encephalopathy; start with 0.25 mg/kg/min to a maximum of 5 mg/kg/min; the effect of cyanide poisoning of the fetus may occur with therapy lasting more than 4 hours).
Sudden and severe hypotension may occur when any of these drugs are given, especially the short-acting nifedipine. The ultimate goal of lowering blood pressure in emergency situations should be its gradual normalization.
In the treatment of acute hypertension, the intravenous route of administration is safer than the oral or intramuscular route, since it is easier to prevent accidental hypotension by stopping the intravenous infusion than by stopping the intestinal or intramuscular absorption of drugs [20].
Of the above drugs for relieving hypertensive crisis in pregnant women, only nifedipine is currently registered with the Pharmaceutical Committee of the Russian Federation. However, the instructions for this drug indicate pregnancy as a contraindication to its use.
Thus, the problem of arterial hypertension in pregnant women is still far from being resolved and requires the combined efforts of obstetricians, clinical pharmacologists and cardiologists.
Literature
- Arias F. High-risk pregnancy and childbirth: trans. from English M.: Medicine. 1989. 654 p.
- Ardamatskaya T.N., Ivanova I.A., Bebeshko S.Ya. Prevalence and features of the course of arterial hypertension in young people. Modern aspects of arterial hypertension: materials of the All-Russian scientific conference. St. Petersburg, 1995. P. 28
- Information about medicines for healthcare professionals. Issue 2. Medicines acting on the cardiovascular system. USP DI. Russian edition /ed. M. D. Mashkovsky: trans. from English M.: RC "Pharmedinfo", 1997. 388 p.
- Kobalava Zh. D., Serebryannikova K. G. Arterial hypertension and associated disorders during pregnancy // Heart. 2002. No. 5. P. 244–250.
- Kobalava Zh. D. Modern problems of arterial hypertension. No. 3. 45 p.
- Savelyeva G. M. Obstetrics. M.: Medicine. 2000. P. 816.
- Serov V.N., Strizhakov A.N., Markin S.A. Practical obstetrics. M.: Medicine, 1989. P. 109.
- Serov V.N., Strizhakov A.N., Markin S.A. Guide to practical obstetrics. M.: OOO MIA, 1997. 436 p.
- Williams G. H., Braunwald E. Hypertension of vascular origin // Internal diseases / ed. E. Braunwald, K. J. Isselbacher, R. G. Petersdorf, etc.: trans. from English: in 10 volumes. M.: Medicine, 1995. T. 5. P. 384–417.
- Shekhtman M. M. Guide to extragenital pathology in pregnant women. M.: Triada, 1999. 815 p.
- Abalos E., Duley L., Steyn DW, Henderson-Smart DJ Antihypertensive drug therapy for mild to moderate hypertension during pregnancy (Cochrane Review)//In: The Cochrane Library, Issue 1, 2002.
- Bortolus R., Ricci E., Chatenoud L., Parazzini F. Nifedipine administered in pregnancy: effect on the development of children at 18 months // British Journal of Obstetrics and Gynaecology. 2000; 107:792–794.
- Bucher H., Guyatt G., Cook R., Hatala R., Cook D., Lang J., Hunt D. Effect of calcium supplementation on pregnancy-induced hypertension and preeclampsia: a meta-analysis of randomized controlled trials//JAMA . 1996, 275(14), 1113–1117.
- Butters L., Kennedy S., Rubin PC Atenolol in essential hypertension during pregnancy//BMJ. 1990; 301:587–589.
- Cunningham FG Common complications of pregnancy: hypertensive disorders in pregnancy//In: Cunningham FG, editor. Williams Obstetrics. Stamford, CT.: Appleton and Lange. 1997: 693–744.
- DeCherney A.H., Nathan L. A Lange medical book. Current Obstetric and Gynecologic Diagnosis and Treatment. 9th Edition. McGraw-Hill. 2003; 338.
- Duley L., Henderson-Smart DJ Reduced salt intake compared to normal dietary salt, or high intake, in pregnancy (Cochrane Review)//In: The Cochrane Library/Issue 2, 2000.
- Duley L., Henderson-Smart DJ Drugs for rapid treatment of very high blood pressure during pregnancy (Cochrane Review)//In: The Cochrane Library/Issue 1, 2000.
- Easterling TR, Brateng D., Schmucker B., Brown Z., Millard SP Prevention of preeclampsia: a randomized trial of atenolol in hyperdynamic patients before onset of hypertension // Obstet. Gynecol. 1999; 93:725–733.
- Gifford RW, August PA, Cunningham G. Working Group Report on High Blood Pressure in Pregnancy. July. 2000; 38.
- Hall DR, Odendaal HJ, Steyn DW, Smith M. Nifedipine or prazosin as a second agent to control early severe hypertension in pregnancy: a randomized controlled trial//BJOG. 2000; 107:6:759–765.
- Laupacis A., Sackett DL, Roberts RS As assessment of clinically useful measures of the consequences of treatment//N. Engl. J. Med. 1988; 318:1728–1733.
- Levin AC, Doering PL, Hatton RC Use of nifedipine in the hypertensive diseases of pregnancy. Annals of Pharmacotherapy Levin AC, Doering PL, Hatton RC Use of nifedipine in the hypertensive diseases of pregnancy//Annals of Pharmacotherapy. 1994; 28(12): 1371–1378.
- Magee LA, Duley L. Oral beta-blockers for mild to moderate hypertension during pregnancy (Cochrane Review)//In: The Cochrane Library/Issue 1, 2002.
- Mulrow CD, Chiquette E., Ferrer RL, Sibai BM, Stevens KR, Harris M., Montgomery KA, Stamm K. Management of chronic hypertension during pregnancy. Rockville, MD, USA: Agency for Healthcare Research and Quality. Evidence Report//Tech. 2000: 1–208.
- Ross-McGill H., Hewison J., Hirst J., Dowswell T., Holt A., Brunskill P., Thornton JG Antenatal home blood pressure monitoring: a pilot randomized controlled trial//BJOG. 2000; 107:2:217–221.
- Rudnicki M., Frolich A., Pilsgaard K., Nyrnberg L., Moller M., Sanchez M., Fischer-Rasmussen W. Comparison of magnesium and methyldopa for the control of blood pressure in pregnancies complicated with hypertension//Gynecologic & Obstetric Investigation. 2000; 49:4:231–235.
- The Task Force on the Management of Cardiovascular Diseases During Pregnancy on the European Society of Cardiology. Expert consensus document on management of cardiovascular diseases during pregnancy//Eur. Heart. J. 2003; 24: 761–781.
- Vermillion ST, Scardo JA, Newman RB, Chauhan SP A randomized, double-blind trial of oral nifedipine and intravenous labetalol in hypertensive emergencies of pregnancy//American Journal of Obstetrics & Gynecology. 1999; 181:4:858–861.
- Von Dadelszen P., Ornstein MP, Bull SB, Logan AG, Koren G., Magee LA Fall in mean arterial pressure and fetal growth restriction in pregnancy hypertension: a meta-analysis//The Lancet. 2000; 355:87–92.
- WHO international collaborative study of hypertensive disorders of pregnancy. Geographic variation in the incidence of hypertension in pregnancy//Am. J. Obstet. Gynecol. 1988; 158:80–83.
- Yeo S., Steele NM, Chang MC, Leclaire SM, Ronis DL, Hayashi R. Effect of exercise on blood pressure in pregnant women with a high risk of gestational hypertensive disorders // Journal of Reproductive Medicine. 2000; 45:4:293–298.
A. L. Vertkin, Doctor of Medical Sciences, Professor O. N. Tkacheva , Doctor of Medical Sciences, Professor L. E. Murashko, Doctor of Medical Sciences, Professor I. V. Tumbaev I. E. Mishina MGMSU, TsAGiP, IvSMA, Moscow , Ivanovo
Classification of peripheral vasodilator drugs
Peripheral vasodilator drugs are classified according to their chemical structure and origin into:
- 2-amino-1-phenylethanol derivatives: isoxsuprine;
- nicotinic acid preparations: nicotinic acid;
- purine derivatives: xanthinol nicotinate, pentoxifylline;
- ergot alkaloids: nicergoline;
- Vinca alkaloids: vincamine;
- others: naftidofuryl, bendazole, bencyclane.
In addition, magnesium sulfate, hydralazine, antihypertensive drugs - calcium antagonists (amlodipine, nifedipine, felodipine, isradipine, nitrendipine), nitric oxide donors (sodium nitroprusside), potassium channel activators (minoxidil, diazoxide) have a peripheral vasodilating effect.
There are also combination preparations of the peripheral vasodilator bendazole with the myotropic antispasmodic papaverine.
Treatment and hospitalization of pregnant women with hypertension
In order to confirm the diagnosis and select adequate treatment, pregnant women with hypertension syndrome must be hospitalized three times. Antihypertensive drugs during pregnancy are prescribed strictly by the attending physician, who takes into account the duration of pregnancy and possible complications of intrauterine development of the fetus.
- the first hospitalization is carried out in the early stages (up to 12 weeks) - for the purpose of diagnosing hypertension;
- a second hospitalization is planned in the period from 26 to 30 weeks - in order to change therapy;
- The third hospitalization is prescribed a couple of weeks before the birth - to prepare for it.
When gestosis develops against the background of arterial hypertension, the woman requires immediate hospitalization, regardless of how far along the pregnancy she is at that moment.
Arterial hypertension in pregnant women requires constant drug support. Women are prescribed medications, and not only antihypertensives. During pregnancy complicated by high blood pressure, it is recommended to take sedatives, calcium antagonists, beta-blockers, alpha-blockers. In addition, symptomatic therapy is carried out.
In addition to drug therapy, a woman is recommended to follow a special regimen and diet throughout pregnancy.
There are a number of recommendations for pregnant women suffering from arterial hypertension:
- Observing the correct sleep and rest schedule helps to normalize the emotional state - you need to sleep at least 9 hours a day;
- you need to exclude any physical activity;
- A pregnant woman with arterial hypertension syndrome needs to constantly measure her blood pressure.
The nutrition of a pregnant woman, even despite toxicosis, should be complete and nutritious, with a sufficient amount of vitamins, microelements, proteins and antioxidants. It is recommended to include seafood and other foods containing polyunsaturated acids in your diet.
Features of treatment with peripheral vasodilator drugs
Due to the high risk of shock and collapse - a sharp drop in blood pressure with loss of consciousness - peripheral vasodilator drugs are prescribed with caution to people with hypotension (low blood pressure).
Peripheral vasodilator drugs, lowering blood pressure, with a sharp change in the horizontal position of the body to a vertical one, can lead to an outflow of blood from the brain, which is manifested by dizziness and even loss of consciousness. This condition is called orthostatic hypotension. To prevent the development of such an effect after taking peripheral vasodilator drugs, the patient should lie down or sit for about half an hour, without getting up suddenly.
Since peripheral vasodilator drugs thin the blood, having an antiplatelet effect, their use is contraindicated in patients with reduced blood clotting and uncontrolled bleeding.
When using peripheral vasodilator drugs, you should stop drinking alcohol and smoking.
Causes of high blood pressure during pregnancy
Arterial hypertension syndrome in women during pregnancy can be triggered by several factors. Blood pressure in pregnant women increases due to the following changes:
- the location of the heart changes;
- hormonal changes occur - the level of progesterone and estrogen in the blood increases;
- placental blood circulation increases;
- body weight increases;
- the mobility of the diaphragm is limited.
The development of all hemodynamic changes during pregnancy leads to a complex of problems that trigger arterial hypertension syndrome.
Calcium antagonists[edit | edit code]
When the cell membrane of cardiomyocytes or smooth muscle cells is electrically excited, changes in ionic currents occur, including the influx of calcium. Calcium antagonists block its entry into the cell without affecting the influx of sodium or outflow of potassium. These drugs are also called calcium entry blockers or calcium channel blockers. Calcium antagonists are divided into two groups according to their therapeutic effect: those acting on the heart and those acting on the blood vessels.
I. Dihydropyridine derivatives
. Dihydropyridines, such as nifedipine, are uncharged hydrophobic substances. They relax the walls of the arteries and in a therapeutic dose have virtually no effect on the function of the heart (in an experiment on an isolated heart they have a clear effect). These drugs are called vasoselective calcium antagonists. Vasodilation and a decrease in peripheral vascular resistance lead to a decrease in blood pressure. Afterload on the heart and oxygen consumption are reduced. The development of coronary spasm is prevented.
Indication
The purpose of prescribing nifedipine is not only the prevention, but also the relief of angina attacks.
Side effects
: palpitations (reflex tachycardia due to decreased blood pressure), headaches, and swelling of the legs.
Other dihydropyridine derivatives have similar effects and differ in pharmacokinetic behavior (slower elimination) and more stable blood concentrations.
Nitrendipine, isradipine and felodipine are used to treat hypertension. Nicardipine and nisoldipine are prescribed for angina pectoris. Nimodipine prevents vasospasm after subarachnoid hemorrhage. Amlodipine contains protonated nitrogen in the side chain and therefore can be in cationic form (i.e., carry a positive charge), which explains its very long half-life (t1/2 = 40 hours).
II. Verapamil and other cationic amphiphilic calcium antagonists
. Verapamil at physiological pH has a positive charge on the nitrogen atom and is a cationic amphiphilic molecule. It has an effect not only on smooth muscles, but also on the heart. The influx of calcium causes depolarization in the sinus node of the heart (electrical excitation), in the atrioventricular node (conducting excitation from the atrium to the ventricles), as well as in cardiomyocytes (electromechanical work). Therefore, verapamil has negative chronotropic, dromotropic and inotropic effects.
Indications
. Verapamil is an antiarrhythmic agent and is indicated for supraventricular tachyarrhythmias. During atrial fibrillation and flutter, it inhibits the conduction of impulses through the AV node and weakens ventricular contractions. Verapamil is also used to prevent angina pectoris and treat hypertension.
Side effect.
Reflex tachycardia as a result of exposure to the sinus node is not observed; the heart rate does not change or there may be a tendency towards bradycardia. AV block or heart failure may develop. Patients often complain of constipation, as verapamil blocks intestinal activity.
Gallopamip (a methoxy derivative of verapamil) is very similar in structure and action to verapamil.
Diltiazem (a benzodiazepine derivative) is a cationic amphiphilic compound and has similar effects to verapamil.
Treatment
Almost all patients with hypertension need blood pressure lowering medications. At the initial stage of the disease, with a slight increase in blood pressure, it is sometimes possible to bring the indicators back to normal by changing lifestyle (diet, weight loss, stress management, physical activity). But most patients still require constant medication. If treatment is stopped, high blood pressure, and along with it unpleasant symptoms, and the risk of complications return. During treatment, it is very important to monitor the level of pressure and keep a diary by the patient in which his indicators are recorded. This allows you to select the optimal treatment and accurately assess its effect.
Nowadays, a large number of drugs have been created that reduce blood pressure. Let's look at the main groups of these drugs.
ACE inhibitors
- Enap;
- Diroton;
- Prestarium A;
- Hartil.
They suppress (inhibit) one of the enzymes involved in raising blood pressure and are often used as the first choice drugs when starting treatment for hypertension.
Advantages of this group:
- do not affect the pulse rate (can be prescribed for any pulse rate);
- do not cause an increase in cholesterol and blood sugar levels;
- for diabetes mellitus and chronic kidney disease, they not only reduce blood pressure, but also prevent the development of renal failure;
- these medications are also effective for chronic heart failure.
But this group is not suitable for pregnant (or planning pregnancy) women - it can have a negative effect on the fetus. Also, sometimes, while taking these medications, a dry cough appears. If it greatly bothers the patient, it is necessary to replace it with a drug from another group.
ACE inhibitors are not suitable for pregnant women, because negatively affect the fetus.
Angiotensin receptor blockers (ARBs).
- Lozap;
- Valsacor;
- Aprovel;
- Edarby.
Their mechanism of action is close to the drugs of the previous group, but blocks the process at a different level. In general, they have the same properties as ACE inhibitors. They are often prescribed if a dry cough develops while taking ACE inhibitors, since this group does not have such a side effect.
Beta blockers
- Concor;
- Betalok;
- Nebilet.
They reduce blood pressure by acting on beta-adrenergic receptors of the heart and blood vessels. In addition to lowering blood pressure, these medications slow down the heart rate. They are preferable if you are prone to rapid heartbeats, but if your heart rate is initially low, they are not recommended. When selecting a dose and treatment, pulse control is required (it should be at least 50 beats per minute).
They are also recommended for use when hypertension is combined with coronary heart disease or chronic heart failure. And when combined with bronchial asthma or chronic obstructive pulmonary disease (COPD), they should be used with caution - bronchospasm may increase.
Calcium antagonists
They reduce blood pressure by affecting the calcium channels of cells. They can be used when hypertension is combined with bronchial asthma, COPD, diabetes mellitus, and kidney disease.
Diltiazem, Verapamil, Isoptin (extended form) - also reduce heart rate and can be used as an alternative to beta blockers.
Cordaflex, Normodipin, Lerkamen - without reducing the pulse, they have a vasodilating effect. They are especially effective in increasing diastolic (“bottom”) pressure.
Diuretics
- Hypothiazide;
- Indapamide;
- Arifon-retard;
- Indapamide retard.
Remove excess water and sodium from the body. Especially relevant for people with edema or signs of heart failure. Long-acting indapamide has the least pronounced diuretic effect and minimal side effects, but at the same time it stabilizes blood pressure well.
Diuretics are suitable for people with signs of heart failure.
This group should be used with caution if blood sugar and uric acid levels are elevated.
Centrally acting drugs
- Physiotens;
- Albarel.
They reduce blood pressure by acting on receptors in the brain. As a rule, they are added to combinations of other drugs if the desired effect cannot be achieved.
Combined products
When treating hypertension, combinations of several active ingredients are often used. According to research, the use of combinations is more effective than simply increasing the dose of the drug and causes fewer side effects. Many medications, when used together, complement and enhance each other's effect. That is why many combination drugs have been created, when one tablet contains 2, and sometimes three drugs at once. Their use is both effective and very convenient.
Combinations of 2 drugs:
- ACE inhibitor + diuretic: Enap N, co-diroton, noliprel;
- ACE inhibitor + calcium antagonist: tarka, dalneva, equator;
- angiotensin receptor blocker + diuretic: lozap plus, valsacor N, edarbi clo;
- angiotensin receptor blocker + calcium antagonist: lortenza, vamloset, aprovasc;
- beta blocker + calcium antagonist: Concor AM, Logimax.
Combinations of 3 drugs:
- ACE inhibitor + diuretic + calcium antagonist: co-dalneva, triplixam;
- angiotensin receptor blocker + diuretic + calcium antagonist: co-vamloset, Co-Exforge.
When selecting treatment for hypertension, they usually start with small doses and, if necessary, gradually increase them. You cannot sharply reduce blood pressure to normal if it is initially very high. It is better to first stabilize it at a lower level (for example, if the initial blood pressure is more than 180/100, reach values not exceeding 150-160/90 mm Hg), and after some time try to intensify therapy, taking into account its tolerability.
Finding the optimal treatment is not easy. Even doctors need time for this. The patient's active participation in keeping a diary and taking medications regularly is mandatory. Changing the treatment regimen on your own or stopping it can lead to unpleasant consequences, including complications of hypertension (heart attacks, strokes). If for some reason you change your medication intake, do not hide it from your doctor. Only together can we achieve sustainable results in treatment.