Women with diseased heart valves may be at increased risk of negative clinical effects during pregnancy, however, with a positive assessment and an assigned treatment, most of them can succeed We want to give birth to healthy children. The key points for optimizing vaginosis in such patients are accurate diagnosis of the etiology and importance of valve disease, assessment of patients before the onset of vaginess, and after the onset of vaginess. Facts: Severe women with the greatest risk of aggravation in the center, as there may be evidence of such patients.
Hemodynamic changes during vacancy
Vaginism is influenced by underlying hemodynamic changes, which progress over the course of vaginess; hemodynamics then change during the pubertal period and in the post-pubescent period. As the pressure on the heart progresses, the inheritance of placental circulation and hormonal effects increases, an increase in cardiac output by 30–50%, and an increase in heart rate (HR) by 10–20 beats per hour are observed. c. and an increase in blood volume by 30–50%. Systemic vascular resistance decreases, and therefore arterial pressure becomes low, regardless of the growth of cardiac output. The blood volume increases while the erythrocyte mass remains unchanged, and a decrease in hematocrit is avoided. Most of these hemodynamic changes begin already in the first half of the first trimester, reach a peak during the next trimester, and plateau phases occur in the third trimester.
As the puberty progresses, there is an increase in cardiac output, heart rate, arterial pressure and systemic vascular resistance, and all these changes are accentuated in the skin. Painful and anxious women experience increased heart rate and arterial pressure, while pain control and the use of anxiolytics help to reduce the severity of hemodynamic changes. The delivery of the placenta increases after pressure increases, as a result of the low-resistance vessel bed being removed, and after this pressure increases sharply due to the return of venous blood to the mother’s circulatory bed. The loss of blood during bedtimes leads to a further decrease in hematocrit. These changes affect cardiac function in patients with valvular disease, which may require invasive hemodynamic monitoring and aggressive drug therapy. bath in the pre-lapup period. As the canopies are complicated by excessive blood loss, infection, arrhythmia and complex obstetric problems, such patients can grow even larger before treatment.
Methods of correction and recovery of the patient
Types of surgical interventions:
applying clips and rings (correction of the shape of the leaflets and the width of the fibrous base of the valve);- installation of a prosthesis (complete replacement of the mitral valve).
Principles of patient recovery after surgery:
- support of blood rheology (thinning drugs);
- preventing blood clots (antiplatelet agents);
- exclusion of significant physical activity;
- long-term follow-up.
Careful treatment for pregnant women due to diseased heart valves
Women with heart valve disease may not be able to tolerate hemodynamic changes during periods of pregnancy or pregnancy, as there may be no symptoms prior to pregnancy (Table 3). In addition, in some patients who have more than minor valve dysfunction before the onset of pregnancy, during the hour of pregnancy, acute levels of valve dysfunction may develop, for example, gastric mitral regurgitation in inheritance of chordee rupture and acute stenosis inherited from thrombosis of a mechanical prosthesis.
The first stage when treating pregnant patients with heart valve disease - establish the level of risk for mother and fetus on the basis of the functional state, the importance and type of valve disease, the function of the left sac and equal to the pressure in the legen artery (Table 4).
Table 3. Basic principles of treating pregnant women with heart valve diseases
| Rizik assessment • Until the age of pregnancy – History of cardiac symptoms, including arrhythmias – Value of output tolerance to physical fitness and functional class (test with fitness, if necessary) – External echocardiographic follow-up – Anatomy and hemodynamics of valve activity – Function of the shunts and pressure in the legen artery – Stability of cardiac hemodynamics over an hour • Stretch vagutnosti – Respectful repeated history taking and physical examination will be performed once per trimester – Frequent monitoring as new symptoms develop – Change the functional class – Serial echocardiographic follow-up to indicate any changes in symptoms – An effective method of contraception, as long as vaginalness is not bad – Consider the possibility of valve reconstruction or valve replacement if symptoms persist until they become severe – Adjust the necessary medications and dosages to avoid side effects on the fetus • Stretch vagutnosti – Stop unnecessary medications that are not contraindicated for vaginosis – Control of symptoms with the help of medication, bed rest and sourness – Transcutaneous valvuloplasty in cases of necessity and feasibility. – Reconstruction of the valve and its replacement, which prevents uncontrolled symptoms of class III and IV • Sexual period – Short vaginal canopies with partial anesthesia – Position on the left side – Kesariv roztin lishe for obstetric demonstrations – Invasive monitoring in times of need – Medical treatment to optimize the attention on the heart and treat the swelling of the leg • After the canopies – Treat anemia – Medical treatment to optimize the attention on the heart and treat the swelling of the leg – Valve reconstruction or replacement, as indicated – For the sake of recognition of an effective method of contraception |
Table 4. Risk stratification for pregnant women with heart valve disease
| High risk of negative clinical outcomes for mother and fetus • History of cardiac dysfunction or arrhythmia • NYHA class > 2 cyanosis • Dysfunction of the systemic scutum (Vikidu fraction < 40%) • Legenian hypertension (systolic pressure at the pulmonary artery > 50% of systemic pressure) • Valve obstruction in the left chambers of the heart – Important aortic stenosis (valve area <1 cm2, maximum fluidity of the blood stream at the level of the aortic valve with Doppler ultrasound > 4 m/s) – Symptomatic or important mitral stenosis – Important aortic and mitral regurgitation with symptoms of class III or IV according to NYHA – Regurgitation for evidence of normal size of the left sac and its function |
Patients who have a low risk can be encouraged that vaginosis is not contraindicated and it is sufficient to follow up with a primary care physician. Women who are suffering from the middle rhizic need to be treated at a specialized center, and care for the development of pregnancy must be coordinated between the primary care physician and the specialized center. Patients at high risk of maternal and fetal impairment should be optimally monitored in centers where a multidisciplinary team is available.
Presented until the present day of pregnancy
In high-risk patients who have undergone fasting until the planned vomiting, it is recommended to carry out invasive debridement, especially since the valve can be subjected to external insertion or reconstructive surgical insertion without replacing the valve prosthesis ohm In order to further reduce the risks associated with vagusity, giving before the planned vagusity may be of further benefit, a large number of patients who are expecting a newborn baby are encouraged to before surgical delivery in the near post-natal period. If the only choice is valve replacement, many patients and doctors opt for bioprostheses, which, regardless of the period of operation, allow the risk to disappear chronically ї anticoagulant therapy with prolongation of vomiting.
Driven by vagusness
Patients with heart valve disease respond differently to hemodynamic changes that occur during stress, depending on the specific valvular pressure. Patients with left-sided obstructive disorders (mitral or aortic valve stenosis) have difficulty tolerating increases in heart rate, blood volume, and cardiac function. On the other hand, a decrease in systemic vascular resistance often worsens during the hour of pregnancy in women in whom valve disease is accompanied by regurgitation, but in them the situation can radically change if Raptovy growth of vascular resistance can lead to swelling of the legen. Women with pulmonary hypertension are especially unable to tolerate hemodynamic changes during pregnancy and represent a group of high risk patients.
The type and frequency of cardiac vasodilation monitoring is determined by specific valve expressions and clinical changes in the skin patient. It is important to inform the patient about the symptoms and signs of cardiac decompensation and emphasize the importance of seeking medical attention if such symptoms occur. It is important to note that the vascularity of the kidney can be tolerated well, additional factors that increase the pressure on the heart, such as infection, anemia, arrhythmia, thromboembolism of the legen's artery, or simply pain and anxiety, can lead to clinical deterioration will occur and require aggressive treatment. In addition to treating the provoking factor, pressure on the heart can be changed with additional bed rest and sourness. It is sometimes necessary to use careful medication to change heart rate and influence such hemodynamic indicators as pre- and post-vantagement, but this often prevents invasive monitoring. In case of valve damage, such as long-term stress due to overexertion, in late stages of vaginess and in the canopies, stand in the position on the sides; This allows me to avoid changes in the venous rotation to the heart due to the compression of the lower empty vein by the uterus.
Stagnation of drugs
Vaginal women who suffer from congestion of the heart valves often suffer from drug depletion, especially if there is heart failure, significant arrhythmia or obvious prosthetic valve. Although this drug is not completely safe in pregnant women, treatment may be important to maintain cardiac stability. Medicines that are contraindicated for pregnancy include ACE inhibitors, angiotensin receptor blockers, amiodarone and nitropruside, so it is important to switch from the names of the drugs to an alternative treatment before the onset of pregnancy. Before heart medications, which are often used during pregnancy, there are beta blockers, hydralazine, diuretics and digoxin. The optimal approach to anticoagulant therapy during the period of gestation when a mechanical prosthetic valve is evident in the heart calls out the superechiki, which will be discussed below.
Sexual period
In women with evidence of heart valve disease, a short and intense period of pain helps to minimize hemodynamic fluctuations. It is especially difficult to monitor changes in heart rate, cardiac output, venous rotation and vascular resistance in patients with evidence of mitral or aortic valve stenosis, which often requires hemodynamic monitoring, including continuous monitoring of the body. arterial blood acidity, ECG, arterial pressure, pulmonary artery pressure and pressure jammed in the legen's capillaries, as well as the heart's tissue. Fetal monitoring is another way to assess the adequacy of maternal cardiac treatment, since fetal distress is an indicator of damaged cardiac function.
Women with heart valve disease are best treated with vaginal veils if pain is adequately controlled. Caesarean surgery should result in significant hemodynamic changes and greater blood loss, which is why in typical cases it is reserved for obstetric indications. Once the cervix is adequately dilated, induction of the canopies is carried out, and during this period all medical personnel who may be needed during the development of the deformity will be present.
Adequate anesthesia includes both anxiolytics and narcotics to minimize tachycardia and hypertension that result from pain and anxiety. The straining of the mother is reduced to a minimum, often using stagnant forceps or vacuum devices, in order to avoid the rapid increase in systemic vascular resistance and the decrease in systemic venous circulation that occurs during straining. In case of vaginal vulva in women with diseased heart valves, it is recommended to stop antibiotic prophylaxis against endocarditis, since it is impossible to transmit the culprit of complications such as episiotomy.
Why does backflow of blood into the MV occur?
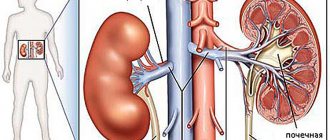
The pumping function of the heart is provided by the left ventricle.
When it relaxes, blood from the atrium flows through the mitral orifice into its cavity. This is the diastole phase. During systole, the ventricle contracts, pushing the blood it contains into the vascular bed. Tightly closed fibrous plates, the mitral valve leaflets, prevent blood from refluxing into the atrium. If their edges do not touch during systole, part of the fluid volume moves back, and regurgitation occurs.
This condition is called mitral regurgitation.
The causes of backflow of blood may be degenerative processes in the valves. A change in the structure of the valve disrupts the shape of its edges and negatively affects the range of motion.
- systemic connective tissue lesions (for example, scleroderma);
- congenital hereditary diseases (Ehlers-Danlos syndrome);
- rheumatism;
- endocarditis of infectious etiology;
- rupture of the chordae (thin strings that connect the edge of the valve and the bottom of the left ventricle; the main function is to prevent eversion (prolapse) of the leaflets towards the atrium);
- dysfunction of the papillary muscles (located at the base of the chordae);
Valvular mitral regurgitation can be caused by changes in the myocardium with a normal leaflet structure:
- expansion of the mitral ring;
- pathological enlargement of the left ventricular cavity (with heart failure);
- hypertrophic cardiomyopathy (typical for hypertension stages 2, 3).
The atrioventricular orifice has a round shape. The basis for the valves is a fibrous ring fused to the myocardium. If the heart muscle stretches, the shape of the hole will change . In this case, the unchanged leaflets will not be able to perform their function (tightly block this outlet for blood during systole) and regurgitation will occur.
If the bicuspid valve does not close completely, this triggers a cascade of pathological processes:
The return of part of the blood volume to the left atrium causes stretching of its walls (dilatation) and overflow with blood.- The myocardium has to push out a larger volume, the muscle fibers hypertrophy compensatoryly and contract more strongly.
- Since blood enters the left atrium from the pulmonary circulation, the pressure in the lungs increases ( the first characteristic symptom appears here - shortness of breath ).
- The right ventricle pumps blood into the lungs, and to overcome the increased resistance it also hypertrophies, but to a lesser extent.
- The left ventricle is gradually stretched by the increased incoming volume of blood.
As long as he is able to cope with the increased workload, there will be no clinical symptoms.
Illness of the song valves
Mitral stenosis
The most common cause of mitral stenosis is rheumatic heart valve disease, which is often first diagnosed during pregnancy. In vaginal women with mitral stenosis, an increase in the cardiac output, which is combined with a decrease in the hour of respiration of the left atrium due to an increase in heart rate, can cause a shift in the pressure in the left atrium and gain yak legen. It is likely that in women who have a lot of common symptoms before pregnancy, a shortened period of diastolic response is expressed as a result of the development of atrial fibrillation and the appearance of comorbid conditions that correspond to an increase in heart rate, such as Nemia or fever often results in hemodynamic decompensation.
The purposes of treatment are: 1) treatment of any pathological condition, such as infection, fever or anemia; 2) adjusting heart rate by increasing the diastolic level; 3) reduction of anterior pressure in the fall, if a swelling of the leg develops, and 4) maintaining an adequate level of arterial pressure. Thus, treatment in typical cases includes bed rest, sour cream, beta blockers, diuretics and antibiotics for signs of infection. In most vaginal women with mitral stenosis, bicilinoprophylaxis is also necessary to prevent recurrence of rheumatic fever.
If, despite adequate medical treatment, persistent hemodynamic instability may require percutaneous balloon valvuloplasty. The advantages of renewing normal placental hemorrhage after this procedure outweigh the risks of the procedure itself, and the risk of damage to the fetus is reduced to a minimum when the lead apron is frozen. In women who, in addition to mitral stenosis, may have concomitant regurgitation on the mitral valve or other contraindications for balloon valvuloplasty, in extreme cases (decompensation persists, regardless of aggression In addition, drug therapy) may negate the need for surgical intervention on the mitral valve. If you want to undergo cardiac surgery if you are pregnant, you should be aware of the information about successful operations for the mother and fetus. The specific risk for the fetus is important to establish from the literature, but, as it appears, it is not directly related to the gestational age or the trivial period of the individual blood flow. The surgical risk for the mother seems to be moving in line with the risk for the non-maternal, important as an inheritance of the urgent nature of the surgical procedure.
Aortic stenosis
Important aortic stenosis is a problem that is difficult to treat due to vagusity. Of course, all women with symptomatic aortic stenosis should undergo surgical treatment until the patient becomes pregnant. Most patients who have no symptoms before vaginess can tolerate vaginess well, but a minority may experience symptoms of heart failure, angina and syncope. Medicinal treatment of symptoms is more problematic and includes bed rest, sourness, reduction of provoking factors, administration of beta blockers and, in case of evidence of volumetric overload, careful administration of diuretics. Drugs that reduce pressure are not safe, fragments on the valves are clearly fixed obstruction. At the Patzindoks, in the Yaki Persistan hemodinamic, the vibor vibor is the Boti through the Ballo Ballon Valvulomia, one of the procedure is able to viconuvati at the Vidpovly morphology, the pathologic aortic valve. In cases of mitral stenosis, if the mother lives in trouble, the possibility of surgical valve replacement is considered.
Leghenian artery valve stenosis
Valvular stenosis of the pulmonary artery can be treated isolated or as a component of a complex congenital heart disease, such as tetralogy of Fallot. In the absence of other hemodynamically significant effects, valvular stenosis of the pulmonary artery is important to be tolerated well. If necessary, you can opt for transcutaneous balloon valvuloplasty.
Aortic or mitral regurgitation
Patients with chronic regurgitation of the mitral or aortic valve in most cases are able to tolerate vasodilation due to decreased pressure, but problems may arise during bedtime and early In the postnatal period, there is an increase in both venous circulation to the heart and vascular resistance. In the pre-apology period, it may be necessary to use diuretics, and in the first 24–48 years after pregnancy, drug reduction after pregnancy may help stabilize the condition.
In contrast to chronic disease of the gastric valves, valvular regurgitation is poorly tolerated. As in non-invasive cases, acute aortic regurgitation (for example, inheritance of aortic dissection or infectious endocarditis of the aortic valve) is not a simple surgical procedure. Women with acute mitral regurgitation, such as inheritance of ruptured chords, can be stabilized using the additional method of internal aortic balloon counterpulsation, except in typical cases, urgent surgery is necessary gіchne delivery.
Regurgitation on the valve of the legen artery
Regurgitation of the legen artery valve is most often diagnosed in patients who previously suffered from congenital heart failure, such as tetralogy of Fallot. These patients with typical episodes also suffer from increased risk of arrhythmia. Insufficiency of the pulmonary artery valve is important to be well tolerated, since the patient has no few symptoms, the right valve has normal systolic function and does not have any dilation. Patients with symptoms, such as worsening of the right valve or systolic dysfunction, should undergo valve replacement until vomiting occurs. Symptoms that arise from vomiting are most important to treat with diuretics and, if necessary, with antiarrhythmic drugs.
Prosthetic heart valves
In the past, there was concern that degeneration may be accelerated in bioprostheses during pregnancy. However, the frequency of degenerative processes in bioprostheses is closely related to the age, and women often have too few implants of bioprostheses for many years until the age of vacancy, so it is entirely possible that the degenerate This bioprosthesis under the hour of vagusness simply reflects the obvious triviality of the functioning of these prosthetic valves. The treatment of pregnant women with bioprostheses does not differ from the treatment of women with diseases of natural valves.
The main difficulty in treating women with mechanical prostheses during vaginosis is the need to maintain chronic anticoagulant therapy. Vagism is a thrombogenic factor, and therefore, vaginal women with mechanical prostheses have a group of displaced rhizics due to thrombosis of the prosthesis. Ideally, the method is continuous effective anticoagulant therapy, which is safe for both the mother and the fetus. Unfortunately, there is no drug available for this drug. Warfarin is a teratogenic drug, especially in the first trimester, the estimated risk of fetal defects is 5 to 10%, but this risk may be much lower if the daily dose of warfarin is ≤ 5 mg. Warfarin is also associated with increased intracerebral hemorrhage in the fetus. Heparin is safe for the fetus, since the veins do not pass through the placenta and can be used both subcutaneously and in the form of continuous infusion, but heparin is not safe enough for the mother, since it is difficult to ensure adequate ny and stable level of anticoagulation. Vaginism induces a hypercoagulable state, which is why the stagnation of subtherapeutic doses of anticoagulants and the risk of thrombosis is a risk for both anticoagulant therapy with warfarin and heparin; It is therefore important to achieve higher levels of anticoagulation and maintain frequent monitoring.
Currently, there is no clearly defined approach to anticoagulant therapy for vaginosis. It’s a good idea to take heparin from the 36th week of pregnancy to bed. In more early periods of pregnancy, treatment options include:
- (1) heparin during the first trimester, then warfarin until the 36th trimester;
- (2) heparin throughout the entire period of gestation;
- (3) warfarin until the 36th pregnancy.
Physicians are unaware of various aspects of anticoagulant therapy, and the patient must have a detailed discussion discussing aspects of various treatment options. Warfarin is safe for the mother, but has more risks for the fetus, and for heparin, the ideal method of administration is more important. If warfarin is prescribed, the dose of the drug should be adjusted to maintain the international normalized ratio (INR) within the therapeutic range for the specific type of valve in accordance with the recommendation; It is necessary to monitor the MHC more frequently in pregnant patients than in non-vigilant patients.
If heparin becomes stagnant, options for administering the drug include continuous intravenous administration of unfractionated heparin through an indwelling venous catheter, subcutaneous administration or stasis of low molecular weight heparin. The most important principle to be followed during heparin therapy is dose adjustment to maintain a therapeutic level of anticoagulation. When administering unfractionated heparin, it is recommended to achieve an active partial thromboplastin hour that is 2.5 times higher than that of the control. The negative aspects of continuous intravenous administration of heparin are the risk of infection, the high risk of treatment and insecurity for the patient. Acute administration of heparin will require significant dose adjustments and frequent monitoring.
The stagnation of low molecular weight heparins becomes superfluous. Prolonged therapeutic effect makes low-molecular-weight heparin an attractive alternative to unfractionated heparin, and early evidence shows an increased risk of prosthetic thrombosis in pregnant women. However, more recent studies suggest that the increased incidence of thrombosis was associated with inadequate dosing and inadequate monitoring. If low-molecular-weight heparin is used, the drug should be administered early two days a day to ensure an adequate therapeutic effect 4 years after dosing, the level of antifactor Xa should reach 1.0–1.2.
Prepared by Volodymyr Pavlyuk
Diagnostics of the process and detailing of complaints
The disease can only be diagnosed after the patient seeks help. Mitral valve regurgitation of the 1st degree (up to 5 ml) is not clinically manifested. Symptoms occur with more significant hemodynamic disturbances.
Long-term concealment of mitral insufficiency is ensured by thickening of the left ventricular myocardium. However, when the reserves of this mechanism are depleted, the patient’s condition sharply worsens.
There are 5 stages of mitral insufficiency.
| Stage | Complaints | Hemodynamic disorders | Treatment |
| Compensation | None | Clinically insignificant regurgitation, up to 1+ (no more than 5 ml) | Not required |
| Subcompensations | Shortness of breath when walking long distances or running | Regurgitation within 2+ (about 10 ml). Left heart: ventricular hypertrophy, atrial dilatation | Surgical treatment is not indicated |
| Right ventricular decompensation | Breathing problems with minor exercise | Significant regurgitation, 3+. Dilatation of the left ventricle, enlargement of the right sections. | Surgical treatments are recommended |
| Dystrophic | Shortness of breath without external causes, cough, swelling, fatigue | Deterioration of the pumping function of the heart, relative insufficiency of the tricuspid valve | Surgical treatment indicated |
| Terminal | The patient's condition is serious. Hemoptysis, cough, swelling, poorly healing ulcers. | Decompensation of the circulatory system | Treatment not indicated |
The army will not accept for military service a person with regurgitation of the second degree or higher!
Typical complaints with mitral insufficiency:
shortness of breath (initially with significant physical activity, in the terminal stages - on an ongoing basis);- palpitations (during physical activity);
- acrocyanosis (blue discoloration of fingertips);
- “mitral butterfly” (blue blush on the cheeks);
- cardialgia (pain in the heart of an aching or pressing, sometimes stabbing nature, not necessarily associated with stress);
- swelling in the legs (appears in the afternoon, in the evening, in the initial stages disappears overnight);
- pain in the right hypochondrium (appears as a result of blood stagnation, with pronounced swelling);
- cough (with stagnation of blood in the pulmonary circulation, often unproductive);
- hemoptysis (with decompensation of the patient’s condition).
Hemodynamic disorders can be diagnosed using the following instrumental methods:
- electrocardiography (left ventricular hypertrophy, arrhythmias, after the third stage - right ventricular hypertrophy);
- phonocardiography (the first tone is weakened, a systolic murmur is determined at the apex of the heart);
- echocardiography (enlargement of the heart cavities and thickening of the myocardium, changes in the movements of the interventricular septum, calcifications in the mitral valve leaflets);
- Doppler echocardiography (detection of the return of part of the blood to the atrium during ventricular systole).
Literature
- 1. Reimold SC, Rutherford JD. Clinical practice. Valvular heart disease in pregnancy. N Engl J Med 2003;349:52-9.
- 2. Bonow RO, Carabello BA, deLeon AC, et al. ACC/AHA guidelines for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on management of patients with valvular heart disease). J Am Coll Cardiol 1998;32:1486-588.
- 3. Qasqas SA, McPherson C, Frishman WH, et al. Cardiovascular pharmacotherapeutic considerations during pregnancy and lactation. Cardiol Rev 2004;12:201-21.
- 4. Myerson SG, Mitchell AR, Ormerod OJ, et al. What is the role of balloon dilatation for severe aortic stenosis during pregnancy? J Heart Valve Dis 2005;14:147-50.
- 5. Ginsberg JS, Chan WS, Bates SM, et al. Anticoagulation of pregnant woman with mechanical heart valves. Arch Intern Med 2003;163:694-8.
- 6. Elkayam U, Bitar F. Valvular heart disease and pregnancy part I: native valves. J Am Coll Cardiol 2005;46:223-30.
- 7. Stout KK, Otto CM. Pregnancy in women with valvular heart disease. Heart 2007;93:552-558.
Causes
Valve dysfunction and regurgitation can develop as a result of inflammation, trauma, degenerative changes and structural abnormalities. Congenital incompetence occurs as a result of intrauterine developmental defects and may be due to heredity.
Reasons that can lead to regurgitation:
- infective endocarditis;
- systemic autoimmune disease;
- infective endocarditis;
- chest injury;
- calcification;
- valve prolapse;
- myocardial infarction with damage to the papillary muscles.
Therapy for pulmonary regurgitation
Violations of the zero and first degrees do not require treatment, children are not exempted from physical education, young men can be drafted into the army, physical activity is indicated for them.
Second and third degree disorders are treated depending on the symptoms and the presence of the underlying disease.
Complications that are not amenable to conservative therapy are an indication for surgical intervention.
The prognosis of pulmonary regurgitation depends on the age of the patient, concomitant diseases and the degree of impairment.
All patients with this problem are observed by a cardiologist and must undergo a full examination every six months in order to identify and treat emerging problems.
Lack of adequate treatment and self-medication can lead to heart failure, even death.
Degrees of regurgitation
A slight reflux of blood near the valve leaflets, which does not affect the functioning of the heart and the physical condition of a person, is called in medicine - physiological regurgitation (grade 1).
With the existing slight turbulence of flow at the valves (valvular regurgitation), they remain healthy. This condition is a variant of the norm.
This term applies only to the tricuspid valve.
Despite the fact that usually the physiological condition in the first degree does not cause clinical manifestations, in some cases a person begins to be bothered by symptoms such as arrhythmia and shortness of breath.
Symptoms of 2 and 3 severity:
- breathing disorders;
- swelling;
- bluish skin tone;
- arrhythmia.