Hydropericardium refers to the accumulation of transudate (non-inflammatory fluid) in the pericardial cavity. Normally, between the layers of the pericardium there is a small amount of lubricant (about 30 ml), which is necessary for the normal functioning of the heart. An increase in the volume of transudate is usually due to increased permeability of the vessels of the pericardial sac in the decompensated course of chronic diseases, or difficulty in its reabsorption, which is caused by venous stagnation.
- Causes
- Symptoms and possible complications
- Diagnostics
- Treatment, prognosis and prevention
What is pericarditis
Pericarditis is an inflammation of the pericardium, the thin, two-layered sac that surrounds the heart.
There is a small amount of liquid between the layers to prevent friction during beating. When the layers become inflamed, this can lead to disruption of the full functioning of the heart, the formation of adhesions in the cavity, fluid accumulation and chest pain. The pericardium also helps keep the heart inside the chest. Pericarditis usually occurs suddenly and lasts from several days to several weeks.
Anyone can get pericarditis. In most cases, it goes away on its own. However, 15 to 30% of people get it more than once—this is called recurrent pericarditis.
There are several forms of pericarditis:
- acute - it can occur on its own or as a symptom of an underlying disease;
- recurrent - can be periodic or constant, the first recurrence usually occurs within 18 - 20 months from the initial illness;
- chronic - in this case, relapse occurs immediately after treatment;
- delayed (Dressler syndrome) - it develops several weeks after heart surgery or a heart attack;
- constrictive - the pericardium scars or sticks to the heart so the heart muscle cannot expand (this form is rare and can develop in people with chronic pericarditis or after heart surgery);
- effusion-constrictive pericarditis - in this case, effusion (fluid) accumulates in the pericardium and a narrowing of the heart occurs.
One third of people with pericardial effusion develop cardiac tamponade, which requires emergency medical attention.
Epicardial fat and cardiovascular risk. Is there a connection
00:00
Gilyarevsky Sergey Rudzherovich , Doctor of Medical Sciences, Professor:
— I am pleased to give the floor to Olga Nikolaevna Korneeva. The topic is intriguing.
Korneeva Olga Nikolaevna , Candidate of Medical Sciences:
— Good afternoon, dear colleagues.
The topic of my report is intended to answer the question: is there a connection between epicardial fat and cardiovascular risk. Of course, risk factors for cardiovascular disease have been known for a long time. One of the founders of the concept of risk factors for cardiovascular diseases can be considered the outstanding clinician Alexander Leonidovich Myasnikov.
I took the liberty of quoting his textbook “Fundamentals of diagnosis and private pathology (propaedeutics) of internal diseases.” He identified the already traditional risk factors for cardiovascular diseases, such as heredity, mental stress, tobacco and alcohol abuse, and predisposition to atherosclerosis.
In his opinion (we see that this is still relevant today), people with a hypersthenic physique serve, perhaps because their blood has a higher cholesterol level. Also, atherosclerosis is often combined with obesity, gout and cholelithiasis.
In the 21st century, we see that the range of cardiovascular markers has expanded significantly. This became possible thanks to the rapid development of laboratory and instrumental diagnostic methods.
More than 20 cardiovascular markers are presented. Many of them are determined using ultrasound diagnostic methods and biochemical diagnostic methods. Perhaps in the future this list will be supplemented with a new marker, which is the subject of our discussion - epicardial fat.
Speaking about obesity, we must understand that the most dangerous (everyone already knows this) is visceral obesity. More familiar to cardiologists and therapists, this is a patient with an abdomen, with a tummy, which makes up the bulk of patients who come to see a doctor. The so-called abdominal type of obesity.
It is also necessary to understand that visceral obesity is not limited to abdominal localization. Excess fat in the body finds its home in all organs and tissues. Lipids are also deposited inside cells in skeletal muscles and in the liver, leading to the development of non-alcoholic fatty liver disease, causing steatosis of the pancreas. Subsequently, the beta cells of the pancreas are damaged.
The sad ending is the development of type II diabetes mellitus in obese patients. In the heart, fat is deposited both inside cardiomyocytes, leading to fatty degeneration of the myocardium, and outside, increasing the thickness of epicardial fat.
03:21
Epicardial fat (in the literature you can also find the synonym “subepicardial fat”) is adipose tissue that is located between the myocardium and the epicardium. Epicardial fat is visceral fat in origin. It comes from brown adipose tissue. Its origin in embryogenesis is similar to omental fat cells and mesenteric fat.
Pericardial fat, which is located between the layers of the pericardium, is white adipose tissue in origin. There is currently no evidence that pericardial fat plays any role in the development of cardiovascular disease.
Interest in the study of epicardial fat has arisen in recent years. This is due to the fact that previously it was determined only by magnetic resonance and computed tomography. These are quite expensive methods.
In addition, epicardial fat is not equally distributed among animals. It is absent in small animals and practically never found in laboratory rats and mice, which has also limited its active study.
An avalanche of interest in the study of epicardial fat became possible with the help of its diagnosis using echocardiography. Echocardiography is performed on every cardiac patient. Normally, the maximum amount of fat is located behind the free wall of the right ventricle. In our clinical practice, we can easily determine the thickness of the epicardial fat, parasternal position along the long axis of the left ventricle. The anatomical landmark is the aortic ring.
05:20
Over the past 5-7 years, there has been great interest in the study of epicardial fat due to the widespread measurement of epicardial fat using echocardiography. Epicardial fat is currently being positioned as a new marker of cardiovascular disease. It correlates (logically) with the visceral amount of fat in the body, but not with body mass index. Its relationship with waist circumference and the level of low-density lipoproteins was revealed. The thicker the epicardial fat, the more severe the patient's hypertension and the higher their insulin levels.
A close relationship between epicardial fat and coronary heart disease has been proven. In addition, epicardial fat thickness is an independent predictor of major cardiovascular events in patients with acute coronary syndrome.
According to a 2008 Park study, within 30 days, patients with acute coronary syndrome were more likely to develop fatal and nonfatal heart attacks and cerebral stroke if their epicardial fat thickness was 7.5 mm (versus 5 mm in the control group). mm).
It should be said that at the moment the quantitative unit of epicardial fat thickness at which we can talk about an increased cardiovascular risk in patients has not been found. Some data give a figure of 7 mm, at which signs of subclinical atherosclerosis are detected. Other data suggest an epicardial fat thickness of 9 mm, at which insulin resistance is highly likely to be diagnosed. Patients with metabolic syndrome are significantly more likely to have a larger layer of epicardial fat (6 mm) than patients without metabolic syndrome (4.9 mm). To date, no clear quantitative value of the epicardial fat layer has been found.
Why is this relationship found between cardiovascular risk and epicardial fat thickness? This happens due to anatomical and morphological changes in the heart. As the thickness of the epicardial fat increases, the heart becomes encased in a fatty shell. In this case, the thickness of epicardial fat can reach 2 cm.
Another important point is that there is no anatomical structure, fascia, between the myocardium and epicardial fat. Adipose tissue fibers literally penetrate the thickness of the myocardium. Data from sectional material and histological pictures are presented, where this feature is clearly visible.
08:35
In addition, when there is an excess of epicardial fat, it is deposited along the coronary arteries. The coronary arteries become encased in a kind of fatty sheath. This is also due to the fact that, as I already said, there is no fascia between the epicardial fat and the myocardium and coronary arteries. All those adipokines and pro-inflammatory cytokines can be directly secreted into the coronary arteries, provoking the rapid development of atherosclerosis.
In addition, there is a general microcirculation between the coronary bed and epicardial fat. Epicardial fat is supplied with blood from the coronary arteries.
As is known, visceral adipose tissue, which includes epicardial fat, is an actively secreting endocrine organ. There are many factors that contribute to the development of atherosclerosis and inflammation in the vascular wall. These include tumor necrosis factor, leptin, interleukins - 1.6, free fatty acids (this is, naturally, a substrate for lipolysis of epicardial fat) and, of course, angiotensin II.
Let's talk about myocardial fibrosis. It has been proven that with epicardial obesity of the heart, myocardial fibrosis develops more quickly. It even precedes the development of left ventricular myocardial hypertrophy, which we also consider one of the triggers for impaired diastolic function of the heart. Apparently, because fat is deposited along the coronary arteries, we see reactive fibrosis (perivascular and interstitial).
Reactive fibrosis, unlike reparative or replacement fibrosis (Oksana Mikhailovna already spoke about this earlier), develops without loss of cardiomyocytes. Normal muscle tissue of the heart is replaced by fibrous tissue. It has been proven that reactive fibrosis is significantly more common in obese hypertensive patients.
Angiotensin II, which is secreted in excess by visceral fat in the heart, affects the synthesis of markers of fibrosis. Their number is increasing. The synthesis of procollagen peptide, transforming growth factor beta (TGF-?) increases. Tissue inhibitor of metalloproteinases increases. All this leads to the rapid development of myocardial fibrosis and disruption of the diatolic function of the heart. Not only due to the fact that the heart is constrained by a fatty shell, but also due to the rapid processes of fibrogenesis.
11:45
Epicardial fat has been shown to influence myocardial thickness. According to Corradi (he examined sectional material), the mass of epicardial fat (both left and right ventricle) was significantly higher in individuals with left ventricular hypertrophy.
Other studies also suggest that epicardial fat contributes to greater left ventricular myocardial hypertrophy. Also, epicardial fat correlates with the degree of atriomegaly and the degree of atrial dilatation.
It also appears to contribute to atrial fibrosis, since normally a small amount of epicardial fat covers the atrial appendages and the surface of the atria. Naturally, as the thickness of the epicardial fat increases, the atria begin to suffer more.
Also recently obtained data. They were announced in June of this year at the meeting of the American Society of Echocardiography. 61 patients without signs of coronary heart disease were studied. Epicardial fat has been found to be associated with impaired left ventricular diastolic function.
Diastolic function was assessed by the decrease in “e” minor or “e”, which reflects myocardial movement in early diastole on tissue Doppler. Multiple regression analysis proved that only age and epicardial fat thickness, regardless of other parameters and associated risk factors, influence the decrease in this e' value.
Data from work in patients with metabolic syndrome, interest in which is still not waning, are presented. It was revealed that metabolic syndrome is characterized by a high frequency of diastolic dysfunction even before the development phase of left ventricular myocardial hypertrophy. It is associated with increased epicardial fat thickness and is also associated with the presence of carotid atherosclerosis.
The natural outcome of the medical history of an obese hypertensive patient is diastolic chronic heart failure. The main mechanisms were announced. These are fibrosis, increased epicardial fat, and hypertrophy of the left ventricular myocardium.
14:23
In addition, it should be remembered that obese hypertensive patients have unfavorable parameters for 24-hour blood pressure monitoring. The work carried out at our department showed that patients with arterial hypertension and visceral obesity have a higher hypertensive load index, increased pulse pressure and a violation of the daily blood pressure profile.
Most of them are non-dippers compared to the so-called thin hypertensives. The heart of an obese hypertensive patient suffers not only from pressure. It's like a driven horse. This is also associated with hypertrophy of the left ventricular myocardium, impaired diastole, severe fibrosis of cardiomyocytes, an increase in the volume of epicardial fat and volume and pressure overload. Moreover, arterial hypertension is associated with a high risk of cardiovascular complications according to 24-hour blood pressure monitoring.
Of course, an obese patient cannot be considered based on any one organ. Obesity occurs not only in the heart, but also in the liver. Non-alcoholic fatty liver disease has also shown an association with cardiovascular disease in recent years.
According to recent data, the risk of cardiovascular disease is 4 times more likely to be observed in patients with non-alcoholic fatty liver disease compared to patients who do not have fatty liver disease. How to explain this relationship between the liver and heart? Perhaps it is the increase in epicardial fat thickness that is the link between cardiovascular risk and non-alcoholic steatohepatitis.
Data from one of the works carried out in 2010. Patients with non-alcoholic steatohepatitis were compared with healthy volunteers. It was found that the thickness of epicardial fat in patients with non-alcoholic steatohepatitis is almost 8 mm versus 4 mm in the control group. It correlates with the amount of body fat, waist circumference, insulin resistance index and the severity of non-alcoholic steatohepatitis (that is, the level of alanine transaminase).
16:57
When choosing a drug for the treatment of cardiovascular complications and arterial hypertension, you still need to think. After all, the deceit of an obese patient is a multiple combined pathology. The drug must be both metabolically neutral and not interfere with the function of other organs compromised by obesity.
Here Lisinopril can come to our aid. The pathogenetic mechanism of its action has already been announced several times today. It is an angiotensin-converting enzyme inhibitor.
In addition, it enters the body in an active form. There is no transformation in the liver. It is excreted through the kidneys to a greater extent, rather than through the liver. This attracts its use in patients with obesity, arterial hypertension and non-alcoholic fatty liver disease
There is no original drug on the Russian market. Many of you are probably surprised to learn that Diroton is a generic drug. Of course, this is the most famous “Lisinopril” in our country.
Patients with obesity and metabolic syndrome are at high risk of developing cardiovascular complications. What to combine with? Of course, the combination of an angiotensin-converting enzyme inhibitor with calcium antagonists is optimal due to the pronounced antihypertensive effect, cardiovascular protection and optimal tolerability with minimal side effects.
Now we can use fixed preparations containing two drugs in one tablet. These include the drug “Lisinopril” plus “Amlodipine” with the beautiful name “Equator”.
The synergy of action has already been mentioned. Angiotensin-converting enzyme inhibitor and calcium antagonist. “Lisinopril” and “Amlodipine” successfully complement each other and affect the processes that occur in the heart of an obese hypertensive patient. These are hypertrophy, fibrosis and a high antihypertensive effect.
I allowed myself to create such a romantic picture where Lisinopril and Amlodipine surround the heart. This is a rational choice of therapy in individuals with obesity and hypertension. Due to the fact that patients adhere to treatment, they have to take only one tablet a day.
The drug is metabolically neutral. This combination has already been discussed today. The risk of cardiovascular complications is reduced. What is important is that fibrosis processes in the myocardium slow down and pronounced antihypertensive activity is noted.
In conclusion, let me summarize the above once again. A new marker of increased cardiovascular risk is epicardial fat. It is easily detected by routine echocardiography.
Epicardial fat contributes to the development of left ventricular myocardial hypertrophy, coronary atherosclerosis, impaired diastolic function, and cardiomyocyte fibrosis. When choosing an antihypertensive drug, it is necessary to take into account all of the above pathophysiological mechanisms. An obese hypertensive patient can safely be prescribed a combination drug of a calcium antagonist and an ACE inhibitor.
Thanks a lot.
Causes of pericarditis in adults
The cause of most pericarditis is unknown, but 80 to 90% of cases are thought to be associated with infections (viruses, bacteria, fungi, and parasites).
In addition, pericarditis can be caused by:
- cardiovascular problems (previous heart attack or surgery);
- injuries;
- radiation therapy;
- autoimmune diseases such as lupus;
- some medications, which is rare;
- metabolic disorders such as gout;
- renal failure;
- some genetic diseases, such as familial Mediterranean fever;
- cancer;
- some medications.
Varieties
There are different types of pulmonary edema:
- fulminant. It develops extremely quickly, in a few minutes - the outcome in this case is only fatal;
- spicy. Symptoms increase over four hours and the risk of death is very high. Such swelling often occurs with heart attack, suffocation, and traumatic brain injury;
- subacute. The development of symptoms alternates between active and quieter stages. Occurs in liver failure;
- protracted. It can develop within twelve hours, even several days, and not have a clear manifestation. It manifests itself in heart failure, as well as chronic lung diseases.
Obviously, each option requires different actions. If the patient can still be saved, speed of response will be a key factor.
Symptoms of pericarditis in adults
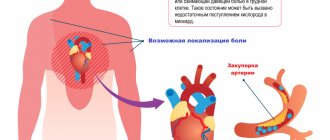
Pericarditis can feel like a heart attack with sudden, sharp or stabbing pain in the chest.
The pain may be in the middle or left part of the chest, behind the breastbone, and may spread to the shoulders, neck, arms or jaw. Other symptoms may include:
- temperature;
- dry cough;
- weakness or fatigue;
- difficulty breathing, especially when lying down;
- cardiopalmus;
- swelling of the feet, legs and ankles.
Symptoms that occur may worsen if the patient lies down, takes deep breaths, coughs, eats, or drinks.
But if he sits leaning forward, it gets better. If the cause of pericarditis is a bacterial infection, the patient may have fever, chills, and a higher than normal white blood cell count. If the cause is viral, there may be flu-like symptoms or stomach upset.
In any case, if chest pain appears (it happens in 85 - 90% of cases), you should immediately call an ambulance.
Left side or right side?
The different symptoms of heart failure depend on which side of the heart is involved. For example, the left atrium (upper chamber of the heart) receives oxygenated blood from the lungs and pumps it into the left ventricle (lower chamber), which in turn pumps blood to the rest of the organs. When the left side of the heart cannot pump blood efficiently, it backs up into the pulmonary vessels and excess fluid flows through the capillaries into the alveoli, causing difficulty breathing. Other symptoms of left-sided heart failure include general weakness and excessive mucus (sometimes mixed with blood).
Right-sided insufficiency occurs when there is difficulty in the outflow of blood from the right atrium and right ventricle, which happens, for example, when the heart valve is not functioning properly. As a result, pressure increases and fluid accumulates in the veins ending in the right chambers of the heart - the veins of the liver and legs. The liver becomes enlarged, painful, and the legs become very swollen. With right-sided insufficiency, a phenomenon such as nocturia or increased nighttime urination is observed.
In congestive heart failure, the kidneys cannot handle large volumes of fluid, and kidney failure develops. Salt, which is normally excreted by the kidneys along with water, is retained in the body, causing even greater swelling. Renal failure is reversible and disappears with adequate treatment of the main cause - heart failure.
Diagnostics
Other tests used for diagnosis include:
- a chest x-ray, which shows the shape of the heart and possible excess fluid;
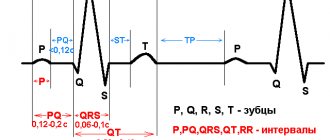
- an electrocardiogram (ECG) to check your heart rhythm and see if the voltage signal is decreasing due to excess fluid;
- an echocardiogram, which will also show the shape, size of the heart and fluid accumulation;
- MRI;
- computed tomography, which provides a detailed image of the heart and pericardium;
- right heart catheterization, which will provide information about the pressure in the heart;
- blood tests to look for inflammatory markers that indicate pericarditis.
Modern methods of treatment
Treatment for pericarditis will depend on its underlying cause.
If it is a bacterial infection, antibiotics may be prescribed. In most cases, according to the American Heart Association, pericarditis is mild and goes away on its own - you just need to rest. But the doctor may prescribe non-steroidal anti-inflammatory drugs (Ibuprofen, Aspirin). If there are other medical risks, the patient may be hospitalized. In this case, therapy will be aimed at reducing pain, inflammation and minimizing the risk of relapse. As a rule, Colchicine is prescribed in this case.
Corticosteroids are also effective in reducing the symptoms of pericarditis, however, studies have shown that early use of these drugs may have an increased risk of recurrence of the disease and should be avoided except in extreme cases where the disease is refractory to conventional treatment.
Surgery may be considered for recurrent pericarditis that does not respond to other treatments, in which case the pericardium is removed.
Forecasts
It is estimated that about 50% of patients diagnosed with heart failure live with the disease for more than 5 years. However, the prognosis for each individual patient depends on the severity of the disease, concomitant diseases, age, effectiveness of therapy, lifestyle and much more. Treatment of this disease has the following goals: improving the functioning of the left ventricle of the heart, restoring work capacity and improving the patient’s quality of life.
You can make an appointment by phone. We are located at St. Petersburg, st. Botkinskaya 15, building 1 (5 minutes walk from the metro station Ploshchad Lenina, exit to Botkinskaya street).
Popular questions and answers
We asked cardiologist Stanislav Snikhovsky to answer questions about pericarditis.
What complications can occur with pericarditis?
In general, pericarditis is considered a disease with a favorable outcome, since timely, qualified care leads to complete recovery in most patients. In rare cases, with severe disease, the following complications may occur:
- thickening or sticking together of the pericardial layers (external and internal), which leads to difficulty in the functioning of the heart and the development of heart failure;
- cardiac tamponade (accumulation of a large amount of fluid between the layers of the pericardium), which also leads to difficulty in the functioning of the heart, the development of heart failure and possible cardiac arrest;
- the formation of fistulas (holes) of the internal mammary artery - this is possible only with purulent pericarditis and is a rare complication.
After pericarditis, cardiac conduction disturbances may occur for a long time. They manifest themselves as periodic attacks of arrhythmia (especially during physical activity).
When to call a doctor at home if you have pericarditis?
Pericarditis usually develops gradually.
Therefore, if major complaints and symptoms occur, you must consult a doctor for diagnosis. Most often, patients complain of shortness of breath (at rest or with light physical exertion), pain in the heart area, palpitations, and general weakness.
Is it possible to cure pericarditis with folk remedies?
There are many treatment options for pericarditis.
As a rule, they depend on the cause of pericarditis (treatment of the disease that caused pericarditis leads to the disappearance of symptoms of pericarditis, up to recovery). Only a doctor can prescribe treatment for pericarditis after a complete examination and determination of the cause of the disease. Folk remedies in the treatment of pericarditis are used as additional therapy and only in the treatment of dry (fibrinous) pericarditis. Among them:
- decoction of young pine needles;
- a collection of hawthorn, calendula, linden flowers and dill;
- infusion of birch catkins;
- collection from the root of valerian officinalis, yarrow and lemon balm leaves.
Published on the portal kp.ru
Therapeutic measures
Treatment for diagnosing fluid in the organ cavity includes two directions: relief of negative symptoms and treatment of the underlying pathology, as well as prevention of complications.
The following methods are used:
- To reduce the amount of sweated exudate, diuretics (Furosemide, Veroshpiron) are prescribed.
Non-steroidal anti-inflammatory drugs are used as drugs to relieve the symptoms of inflammation. For example, Ibuprofen. In severe, protracted cases, Colchicine is used together with it. These drugs are taken simultaneously with probiotics and medications that normalize kidney and liver function (Hilak-forte, Essentiale).- If the causative agent is an infection, antibiotics (Ceftriaxone, Amoxicillin) or antiviral drugs Groprinosin, Interferon are used). If necessary, add antiparasitic and antifungal agents (Nystatin, Pyrantel).
- If the cause is autoimmune pathologies, glucocorticosteroids (Prednisolone, Dexamethasone) and cytostatics (Cisplatin) are used. Prednisolone in small doses is indicated only for relieving asthma attacks, because it is addictive.
- If there is a threat of tamponade, a suspected purulent process, or the absence of resorption of the exudate, a puncture of the pericardial cavity is made in order to remove the fluid mechanically. This procedure is also used to determine the etiology of the disorder.
- In more complex situations, pericardiotomy is used. This is a surgical intervention whose purpose is to remove part of the pathological pericardium.