Unexpected deaths of athletes during performances or matches are part of the depressing statistics today. The reason for this was the high-profile incidents that happened to famous athletes. Since heart problems can be one of the most common causes of unexpected deaths in athletes, we decided to study this issue in more detail. In this article we will try to find out whether physical activity can often lead to the development of complex diseases with a fatal outcome. For obvious reasons, information on the issue we are studying is rarely made public. However, the problem continues to remain relevant and requires the attention of specialists.
Sometimes a problem happens unexpectedly and its development ends in tragedy
Heart disease in athletes
It is no secret that urbanization leads to an increase in population concentration in cities. And this feature forms a new paradigm of thinking. For people who communicate with nature every day, living far from cities, there is no problem of lack of movement. At the same time, residents of megacities need physical activity. Doctors, teachers and politicians talk about this.
So, we have two categories of population associated with the port:
- Professional athletes. This category is characterized by high loads, a specific rhythm of life and fairly constant health monitoring. The deaths of athletes in all disciplines cause serious dissonance in society and controversy among experts. The causes of unexpected tragedies are said to be overtraining, insufficient “warming up” of the body before serious performances, the rigid rhythm of life of professional athletes, non-compliance or violation of the prescribed rules of life, as well as doping. But the main ones, without a doubt, are heart disease.
- Lovers. These people go in for sports constantly or sometimes - in the warm season, on the advice of doctors, as a temporary hobby. Mortality problems in this category may be caused by a lack of awareness of one's own health status and a low level of knowledge about training systems. As a rule, sports heart syndrome is not observed in amateurs. To improve heart function and quickly gain the necessary body tone without developing pathologies, doctors at the Military Academy of the Russian Academy of Medical Sciences (St. Petersburg) recommend taking Khavinson’s peptide bioregulators, in particular Cardiogen.
Sports heart syndrome in cyclists is not a rare occurrence, as is the development of pathologies that are recognized as diseases.
Treatment
No specific therapy is required if there are no:
- pain;
- fainting;
- ischemia;
- arrhythmia;
- increased fatigue;
- conduction disturbance.
In this case, the changes are considered physiological. As a means of prevention, the following may be prescribed:
- Beta blockers.
- Adaptogens.
- Vitamin and mineral complexes.
- Nutritional supplements.
In case of serious cardiac dysfunction, complex treatment is carried out using cardiotonics, antihypertensive and antiarrhythmic drugs.
Proper nutrition plays an important role, especially for young athletes. The menu should contain a sufficient amount of protein, be rational and quite high in calories. You should eat foods rich in vitamins and minerals.
The diet must include the following products:
- cottage cheese;
- vegetables;
- fruits;
- fish;
- meat;
- juices
In advanced cases, surgical intervention and complete abstinence from sports activities are indicated, sometimes requiring the installation of a pacemaker.
Health problems that lead to early mortality
Doctors know several factors that have a greater impact on the well-being of active people:
- Congenital heart defects – these are associated with abnormalities in the structure of the heart that are present at birth. About a quarter of the population has a kind of “hole” in the heart, which may not cause any symptoms at all throughout life. But it can also lead to serious health complications in the second half of life.
- Coronary artery disease can lead to heart attack, stroke or heart failure.
- Arrhythmia, characterized by an abnormal heartbeat (too fast, slow, or irregular) can potentially lead to other heart problems and affect people of all ages, including newborns, young adults, adults, midlife, and the elderly.
- Hypertension is one of the most common cardiovascular diseases among athletes and people leading an active lifestyle. Hypertension usually begins in early adulthood, gradually developing into a serious problem in old age.
These are just a few of the heart diseases that athletes can develop. Although a healthy diet and physical activity can reduce the risk of heart disease, an athlete may still be at risk due to age, family history, or other factors. To reduce the risk of developing pathological heart disorders caused by excessive stress, take the peptide bioregulator Cardiogen.
Coronary heart disease may not manifest itself for a long time. It develops over the years.
Sports heart in childhood
A child involved in professional sports has some characteristics and differences from an adult. This is due to a discrepancy in the growth of internal organs (including the heart) compared to the musculoskeletal system, as well as a hormonal “explosion” in adolescents (especially girls). After just 2-3 months of daily strength and speed training, the child experiences adaptive changes in the cardiovascular and respiratory systems. In other words, the rudiments of myocardial hypertrophy begin to form already at this time.
Before sending a child to big sports, parents should carefully take care of a full medical examination. Regarding the cardiovascular system, an ECG, ultrasound of the heart and Rufier's test are mandatory. Those children who have begun to engage in professional sports should conduct the same studies annually and visit a cardiologist.
Children who do not experience any clinical manifestations during or after exercise (loss of consciousness, darkness before the eyes, stupor, sensations of interruptions in the heart, pain in the chest) can continue playing sports. Otherwise, intense training is contraindicated.
Prevention of heart disease in athletes
Dr. Vijay Subbarao, a cardiologist at Denver's Heart and Rose Medical Center who specializes in treating athletes and patients with heavy physical activity and heart disease, believes the following preventive measures should be mandatory for athletes:
- heart health screenings;
- prevention and regular examinations;
- supply system;
- compliance with the rules of training and performances.
Most sudden deaths in young athletes are due to hereditary or genetic heart disease. Assessing each athlete for their risk of developing certain diseases is a complex task. Hence the problems of athletes dying during training or performances.
Among hockey players, there are the following statistics on death from heart and vascular diseases (USSR, Russia):
Viktor Blinov died on July 9, 1968 during training from heart failure; Andrey Zemko - died in July 1988 at a training camp from a heart attack; Alexander Kravsun - died of a stroke on 07/03/2002 during training; Alexey Cherepanov - died on October 13, 2008 from myocarditis - the attack occurred during the match; Igor Misko - died on 07/06/2010 from cardiac arrest while driving a car.
Amateur level gymnastics does not cause heart pathologies
How to exercise without harming your heart
Consult your doctor before starting to exercise if you have not exercised for a long time or have never exercised. If you have heart disease or risk factors for it, your doctor may recommend an exercise tolerance test.
Start training gradually. For example, do the exercises at a slow pace or only for a few minutes. Over time, you can increase the intensity and duration. Warm up before your workout and cool down after.
Stop exercising and contact your doctor immediately if you experience any of the following symptoms during exercise:
- pain, tightness, heaviness in the chest, arms, throat, jaw, or back;
- nausea or vomiting;
- a feeling of “fluttering” of the heart or a very rapid heartbeat;
- severe dizziness, weakness, fatigue;
- inability to catch your breath;
- pain in the joints, legs, heels or calf muscles (this is not an emergency, but it is also better to consult a doctor about it).
So that the training does not harm:
|
Use household activities if you find it difficult to find time for a full workout:
- take the stairs instead of the elevator;
- park further from your destination or get off one stop earlier than yours on public transport;
- take a longer route when going somewhere;
- spend your free time actively, choose outdoor games;
- get a pet that needs to be walked;
- clean the house yourself.
The health of your cardiovascular system and other body systems depends on whether you move enough. There are no pills, supplements, devices or techniques that can take the place of movement, so take every opportunity to move.
Author: Ksenia Benimetskaya, cardiologist, nutritionist, Ph.D.
Literature
1. The Physical Activity Guidelines for Americans, JAMA, 2021 2. Strength training for health in adults: Terminology, principles, benefits, and risks — UpToDate 3. The benefits and risks of aerobic exercise — UpToDate 4. Exercise-induced oxidative stress: cellular mechanisms and impact on muscle force production, Physiol Rev, 2008 5. Worldwide trends in insufficient physical activity from 2001 to 2016: a pooled analysis of 358 population-based surveys with 1·9 million participants, Lancet Glob Health, 2021 6. Recommendations on physical activity, Sekta 7. Resistance training and executive functions: a 12-month randomized controlled trial, Arch Intern Med, 2010 8. Different modalities of exercise to reduce visceral fat mass and cardiovascular risk in metabolic syndrome: the RESOLVE randomized trial, Int J Cardiol, 2013 9. The effect of 12 weeks of aerobic, resistance or combination exercise training on cardiovascular risk factors in the overweight and obese in a randomized trial, BMC Public Health, 2012 10. Is yoga heart-healthy? It's no stretch to see benefits, science suggests, Heart.org, 2021 11. 2021 European Guidelines on cardiovascular disease prevention in clinical practice: The Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice ( constituted by representatives of 10 societies and by invited experts) 12. The effectiveness of yoga in modifying risk factors for cardiovascular disease and metabolic syndrome: A systematic review and meta-analysis of randomized controlled trials, European Journal of Preventive Cardiology, 2014 13. Effects of yoga in patients with paroxysmal atrial fibrillation - a randomized controlled study, European Journal of Cardiovascular Nursing, 2021 14. Yoga for Heart Failure: A Review and Future Research, Int J Yoga, 2021 15. Tai Chi Boosts Heart Health, Cleveland Clinic, 2021 16. Tai Chi exercise for psychological well-being among adults with cardiovascular disease: A systematic review and meta-analysis, European Journal of Cardiovascular Nursing, 2021 17. 3 Kinds of Exercise That Boost Heart Health, Hopkins medicine 18. State of the Art Review: Atrial Fibrillation in Athletes, Heart Lung Circ, 2021 19. Atrial Fibrillation (AF) in Endurance Athletes: a Complicated Affair, Curr Treat Options Cardiovasc Med, 2021 20. Atrial fibrillation in athletes and general population. A systematic review and meta-analysis, Medicine, 2021 21. The “Extreme Exercise Hypothesis”: Recent Findings and Cardiovascular Health Implications, Curr Treat Options Cardiovasc Med, 2021 22. Increased Cardiovascular Disease Mortality Associated With Excessive Exercise in Heart Attack Survivors, Mayo Clinic Proceedings, 2014 23. A reverse J-shaped association of leisure time physical activity with prognosis in patients with stable coronary heart disease: evidence from a large cohort with repeated measurements, Heart, 2014 24. Frequent physical activity may not reduce vascular disease risk as much as moderate activity: large prospective study of women in the United Kingdom, Circulation, 2015 25. Dose of Jogging and Long-Term Mortality: The Copenhagen City Heart Study, Journal of the American College of Cardiology, 2015 26. Are you getting too much exercise? MedlinePlus, 2020
Athletic heart syndrome
Doctors observe this non-pathological condition mainly in patients associated with heavy and regular physical activity. Athletic heart syndrome is characterized by the following features:
- large heart size compared to normal;
- lower contraction frequency at rest.
The athletic heart, due to long-term loads, is improved in a specific way.
It is important to understand that physiological adaptations to exercise training result in structural and functional changes in the heart that may be confused with heart disease:
- Training with dynamic exercises leads to an increase in the size of the heart chamber and the mass of the left ventricle.
- Static exercise increases left ventricular wall thickness and left ventricular mass. These changes in cavity size and hypertrophy can alter the ECG in ways that resemble pathological chamber enlargement and may resemble patterns seen with inflammation or myocardial infarction.
- Dynamic exercise also reduces resting heart rate and can lead to excessive resting vagal tone, leading to abnormalities such as atrioventricular block and atrial vagal pacemaker.
All these rhythm disturbances usually disappear in a trained athlete after performing exercises.
Some sports are contraindicated for heart disease
Is it possible to develop a sports heart through physical education?
When engaging in physical activity as usual (exercise, jogging, Nordic walking, swimming), hypertrophy does not develop, but adaptation mechanisms in the heart are still formed. Thus, in people who regularly and for a long time engage in physical exercise, the heart rate also decreases and the minute volume of blood increases, but a clearly defined thickening of muscle fibers does not occur. In order for the “athlete’s heart” to be formed, long-term daily training that develops endurance is necessary, lasting at least 3-4 hours of intensive training per day.
Features of heart development by sport
Cyclists and long-distance runners are known to have very large hearts. In contrast, athletes who do little aerobic exercise, such as golfers, have normal-sized hearts.
Athletes with significant static training, such as weightlifters, often have thick left ventricular myocardial walls that may exceed the upper limits of normal. One study documented wall thicknesses of up to 16 mm in elite athletes.
ECG studies among athletes have also shown that:
- 17% of men and 8% of women had clearly abnormal ECGs.
- 28% of men and 14% of women had moderate ECG abnormalities.
Abnormal ECGs were further assessed and it was found that the majority were in high aerobic fitness sports such as cycling.
89% of athletes with lower aerobic fitness, such as equestrians, had normal ECG readings.
Among 145 patients with obvious ECG abnormalities, 14 were found to have cardiovascular disease. Among the remaining 131, two thirds had enlarged cavities or thickened ventricular walls on echocardiogram. And one third had completely normal ECG readings. Thus , most athletes with ECG abnormalities do not suffer from heart disease.
Most athletes do not suffer from heart pathologies - this is evidenced by statistics
Professional sports
From a medical point of view, any hypertrophy of our left ventricle is considered as a risk of developing pathologies. Professional athletes very often go beyond the anaerobic limit and provoke d-hypertrophy of the heart muscle. Experts believe: if you have developed a sports heart, then it is critically important for you to be physically active for the rest of your life.
Having been at the rank of a pro, you can no longer allow yourself to relax in the future. For such a person, a sedentary lifestyle will be destructive. This is our biological reality. Former athletes who do not get out of their chairs are more likely than the average person to develop hypertension. And it brings with it a huge number of other ailments.
Mortality statistics
In the USA, testing of students, schoolchildren and active youth passionate about professional sports occurs constantly. This is due to the fact that sports training is part of the educational programs of many educational institutions. In this country, more than 5 million active athletes are under the age of 20.
In this case, there are the following statistics:
- The sudden death rate among high school athletes is 1:100–200,000.
- Among marathon runners, deaths are recorded at around 1:50,000.
- Among recreational runners, the mortality rate is 1:15,000.
Thus, sudden cardiac death in sports is a rare event.
However, sudden cardiac deaths in competitive athletes are still highly visible emotional events. They come under intense public scrutiny because they occur in young people who are considered healthy.
In athletes over 35 years of age, especially men, the most common cause of sudden death is atherosclerotic coronary artery disease. In younger people, atherosclerotic coronary artery disease is much less common, and other diseases predominate:
- Hypertrophic cardiomyopathy.
- Anomalies of the coronary arteries.
- Abnormal left ventricular hypertrophy.
- There are other causes of sudden death, such as asthma, heat stroke, drug abuse, and injuries that cause structural damage to the heart.
Any sports activity requires careful monitoring of your health so that heart disease does not cause death.
Differences between L and D hypertrophy
First, let's talk about l-hypertrophy. It comes initially from long training. The pulse does not exceed 150 beats per minute. But everything is purely individual and often different. In general, l-hypertrophy is aerobic cardio training that does not cross the anaerobic threshold. Roughly speaking, we run, but not very fast, so as not to start suffocating. The heart increases in volume up to 40%.
With d-hypertrophy, the pulse operates at 150 beats per minute, and this can be called the physical limit. Let's say we run and for the last few minutes we do it as hard as we can. You can also do something similar in the gym when we do drop sets and supersets. As a result, the heart does not have time to fully open. Relaxation does not occur, and a diastole defect appears. Those. Local acidification occurs in our myocardium and causes myofibrils to grow.
As a result, each of us is able to grow due to the elasticity or acidification of our heart, and this is not a very healthy situation.
How to prevent deaths in sports
It is extremely important for people who are involved in active training and have a confirmed hereditary history of cardiovascular disease to undergo regular medical examination.
It is known that Irina Viner’s wards (gymnasts) are selected for the national team on the basis of a genetic passport, which clearly indicates the girls’ risks for a particular disease. In some cases, even very talented gymnasts are excluded from further challenging training.
In the case of amateur athletes, which usually concerns young people, before starting classes in any section, it is important to undergo a medical examination and consult with your attending physician. If the examination reveals contraindications to training, the athlete should be temporarily suspended from training until the problem is resolved.
The doctor must resist pressure from the athlete, his family, the coach and the administration of educational institutions, performing exclusively his function, which is aimed at preserving the life and health of the patient.
Physical activity is a great factor in maintaining health - it's important to remember!
Evaluating an older athlete who wants to take up a fitness program or compete at the Master of Sports level is more difficult. There are several factors to weigh here:
- Health benefits of exercise.
- Risk of cardiovascular diseases.
The focus of doctors is the risk of coronary heart disease. The risk can be significantly reduced by following a training regimen, nutrition, and taking maintenance medications like Cardiogen.
Thus, any physical activity that a person intends to perform on a regular basis requires mandatory preliminary health monitoring. Both professionals and amateurs have risks of serious heart disease or unexpected death. Special control groups include young athletes and people over 35 years of age. In the first case, doctors need to assess the young person's predisposition to heart disease through family history and testing of general indicators. In the second case, it is important to take into account the body’s readiness for increased loads, since in the first half of the athlete’s life they could contribute to the development of irreparable pathologies.
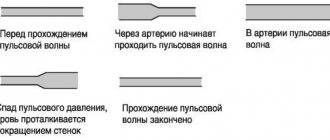
Heart and speed or endurance training
The force of contraction of the heart muscle obeys the Frank-Starling law: the more the muscle fibers are stretched, the more intense the compression of the ventricles. This is true not only for the myocardium, but also for all smooth and striated muscles.
The mechanism of this action can be imagined by pulling the bow string - the more it is pulled, the stronger the launch will be. This increase in cardiomyocytes cannot be unlimited; if the increase in fiber length is more than 35 - 38%, then the myocardium weakens. The second way to increase the work of the heart is to increase the blood pressure in its chambers. In response, the muscle layer thickens to counteract hypertension.
All loads are divided into dynamic and static. They have fundamentally different effects on the myocardium. The first type of training involves developing endurance. This is primarily important for runners, skaters, cyclists, and swimmers. The following adaptation processes occur in the body:
- muscle fibers constantly contract and lengthen; Increases blood flow in working muscles
- peripheral arteries dilate;
- blood flow in working muscles increases;
- metabolic reactions with the participation of oxygen are accelerated (aerobic);
- the rhythm of contractions becomes more frequent during exercise;
- vein tone increases;
- the myocardium stretches under the influence of increased blood flow;
- the volume of shock ejection increases.
Thus, in athletes with a predominance of dynamic (aerobic) exercise, dilatation (expansion) of the cardiac cavities is observed with a minimal degree of myocardial hypertrophy.
Isometric loads (strength) do not change the length of muscle fibers, but increase their tone. Tense muscles compress the arteries, and the resistance of their walls increases.
With this type of training, the need for oxygen is moderate, but there is no increase in blood flow through the compressed arteries, so tissue nutrition is provided by increasing blood pressure. Constant hypertension during exercise provokes myocardial hypertrophy without expansion of the cavities.
Watch the video about what happens to the heart during physical activity:
How do you know if your body is ready for physical activity?
To find out if the body is ready for exercise, people with health problems should consult a doctor. Any physical activity requires the right approach, systematicity and understanding of the state of your own body in order to control the load.
If a person is physically or emotionally exhausted, feels unwell, is overweight or has any other pathologies, improperly selected physical activity can harm and complicate the health condition.
Can SCD be prevented?
As a rule, if suspicions are identified during medical examination, a thorough further examination is carried out, and, if a threatening diagnosis is confirmed, athletes are released from the competitive and training regime. Depending on the condition, pharmacotherapy, radiofrequency ablation or surgical treatment may be selected. In some cases, an implantable defibrillator is used, which in threatening situations gives an electrical impulse and allows the heart rhythm to remain stable.