In the 20th century, when medicine made significant progress in the diagnosis and treatment of many chronic diseases, a person most often had one of them and had it treated by a specialized specialist. And so far, most clinical recommendations are intended to treat one chronic disease and do not take into account the presence of other concomitant ones.
Therefore, if a person has several diseases, each specialist he comes to prescribes treatment according to his profile and without taking into account other diseases. As a result, people are forced to take 8 or more medications at the same time, which, instead of recovery and improvement of the condition, can cause its deterioration. The number of such patients has increased significantly recently, and these are not only those who are over 75 years old.
Treating people with a “bouquet” of diseases is a difficult task, since diseases can mutually aggravate each other, and medications for treating one disease can worsen the course of another. To prevent this from happening, doctors from various specialties join forces and treat the patient together. And most often this is a gastroenterologist and cardiologist.
Why are cardiovascular and gastroenterological diseases often combined?
The first reason is that diseases of the gastrointestinal tract and cardiovascular system are among the most common. According to statistics, every fourth person in economically developed countries has some kind of heart or vascular disease; the most common are coronary heart disease and hypertension. On the other hand, there is a constant increase in the number of people suffering from diseases of the gastrointestinal tract (GIT), and in particular diseases of the esophagus, stomach, liver, biliary system and intestines.
The second reason is common risk factors. These include:
- Overweight and obesity.
- Smoking and alcohol abuse.
- Unhealthy and unbalanced diet.
- Insufficient consumption of vegetables and fruits.
- Sedentary lifestyle.
- Increased level of total blood cholesterol (above 5 mmol/l).
- Elevated sugar levels (above 5.5 mmol/l.
- Increased level of low-density lipoprotein LDL (above 2.5 - 3 mmol/l).
The third reason is that over a long period of time, one of the diseases can cause another and vice versa. For example, in chronic cardiovascular failure, the liver suffers, and non-alcoholic fatty liver disease increases the risk of developing heart and vascular diseases by 64%.
The fourth reason is that chronic use of cardiovascular drugs can lead to significant deterioration in gastrointestinal health.
Therefore, people with a combination of hypertension, coronary heart disease, chronic heart failure and diseases of the esophagus, stomach, intestines and liver require joint treatment by a cardiologist and gastroenterologist with the selection of drugs that have minimal damaging effects on the gastrointestinal tract and the additional prescription of gastroprotectors and hepatoprotectors.
Acute gastritis - symptoms and treatment
Diagnosis begins with interviewing and examining the patient. During the conversation, the gastroenterologist clarifies what the patient ate before the signs of acute gastritis appeared, what medications he is taking, and whether he has any concomitant diseases (neuralgia, gallbladder, liver or heart disease). Objectively, attention is drawn to pale and dry skin, coating on the tongue, rashes in the area of the nasolabial triangle, bitterness and bad breath. On palpation (palpation), pain occurs in the epigastrium with irradiation to the left or right hypochondrium.
To confirm the diagnosis, various laboratory and instrumental research methods are used.
Important laboratory tests include:
- clinical blood test;
- 13C-urease breath test for antigen to Helicobacter pylori;
- biochemical blood test - allows you to identify disturbances in the functioning of the pancreas, liver, gallbladder and its ducts.
most commonly used instrumental diagnostic methods are
- radiography with a contrast agent - allows you to examine the relief of the gastric mucosa and the degree of tension of its walls;
- Ultrasound of the stomach - makes it possible to study the affected areas during a detailed examination, but does not allow collecting material for a detailed laboratory study.
FGDS deserves special attention - insertion of a thin endoscope into the stomach through the esophagus. This procedure is the optimal diagnostic method for gastric diseases [12]. It is prescribed regardless of the patient’s age. It allows you to determine the areas and extent of damage to the mucosa, assess the risk of internal bleeding and timely detect a malignant neoplasm.
The advantage of FGDS is the ability to perform a biopsy - to pinch off a small piece of tissue from different parts of the stomach. This procedure is painless and cannot cause bleeding.
The rules for preparing for FGDS are quite simple:
- a few days before the procedure, you need to give up some medications or coordinate their use with your doctor;
- 12 hours before the examination, refuse to eat (if the procedure is scheduled for the morning, then the last meal can be at 18:00, but not later).
Often patients are emotionally frightened due to the upcoming FGDS. The procedure is unpleasant, but tolerable and practically painless. As a rule, 15 minutes are allotted for it, but in the absence of pathologies, the process takes no more than 2-5 minutes.
FGDS can take place under:
- general anesthesia;
- light sedation (pain relief);
- local anesthesia.
Most often, doctors use local anesthesia - irrigation of the mucous membrane of the pharynx and the root of the tongue with a special anesthetic drug. This is a reliable method, proven over the years, which does not cause any complications and is easily tolerated by patients of any age. It allows you to reduce the gag reflex and calm the patient, without causing complications. Within 10-15 minutes the patient feels the same as before.
Anesthesia (medicated sleep) is carried out in the absence of contraindications, is easily tolerated, makes it possible to avoid negative emotions from the procedure, and also allows the endoscopist to work calmly and efficiently. Medication-induced sleep is performed in many countries around the world on a regular basis during a standard endoscopic procedure (sleep endoscopy). Local anesthesia is often an exception to the rule and is performed in the presence of contraindications to intravenous sedation, of which there are very few.
Complications after FGDS are rare. These include: dry or sore mouth, headache due to the patient’s severe nervousness. When the walls of the stomach are straightened during the procedure, belching of air may occur.
to become infected during FGDS if the equipment is processed and sterilized not manually, but in automatic installations for washing endoscopes.
What diseases of the cardiovascular system do cardiologists treat?
The treatment of cardiovascular diseases is carried out by various specialists - cardiologists, cardiac surgeons, arrhythmologists, neurologists, rheumatologists, angiosurgeons.
Cardiologists treat patients with damage to the heart and its blood vessels, as well as peripheral artery disease.
Such diseases include:
- coronary heart disease (CHD);
- angina pectoris
- myocardial infarction
- chronic heart failure;
- congenital and acquired heart defects;
- inflammatory lesions of the heart muscle and pericardium;
- cardiomyopathies (hereditary and secondary);
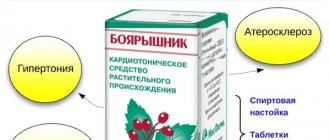
- arterial hypertension (hypertension);
- vascular atherosclerosis;
- disturbances of heart rhythm and conduction.
Which cardiovascular drugs are gastro or hepatotoxic?
Gastrotoxicity of a drug is an undesirable drug reaction, expressed in damage to the organs of the digestive system and associated with the peculiarities of the mechanism of drug metabolism, as well as the dose and duration of their use. When they talk about hepatotoxicity, they mean the predominant damaging effect of the drug on the liver. However, there are drugs that negatively affect both the gastrointestinal mucosa and liver cells.
Drugs prescribed by a cardiologist that can cause toxic damage to the gastrointestinal tract include antiarrhythmic, antihypertensive, hypolipidemic (to reduce the level of cholesterol, triglycerides, low-density lipoproteins associated with the risk of developing vascular atherosclerosis) drugs, as well as aspirin, used to prevent thrombosis. The main task of a cardiologist when selecting therapy is to take into account the existing gastrointestinal disease and select a drug that has less gastro- and hepatotoxicity. In turn, the gastroenterologist observing the patient can additionally select drugs to protect the gastrointestinal tract.
How to distinguish cardiac pain from non-cardiac pain?
The heart and organs of the digestive system are located quite close to each other, therefore, when pain occurs in the left half of the chest, both a gastroenterologist and a cardiologist are involved in the examination and diagnosis. The complaint of chest pain is one of the most common and alarming symptoms for both the doctor and the patient. Differential diagnosis is most often carried out between gastroesophageal reflux disease (GERD) and angina or coronary heart disease, and in case of an acute painful attack, between exacerbation of GERD and myocardial infarction.
In addition to gastroesophageal reflux disease, chest pain can be caused by
- esophageal spasm;
- reflux esophagitis;
- hiatal hernia (hiatal hernia);
- stomach ulcer;
- biliary or intestinal colic;
- cholecystitis;
- pancreatitis.
In addition, there are cases when a patient has both pathologies: gastrointestinal disease and heart disease. In such cases, it must be taken into account that drugs used to treat coronary heart disease and hypertension have a relaxing effect on the smooth muscles of the esophagus and may lead to aggravation of reflux symptoms.
The appearance of gastritis symptoms
This disease manifests itself with different signs. It all depends on the degree and type of disease. The main features include:
- Decreased or loss of appetite.
- Sudden painful sensations in the abdomen, and a feeling of fullness while eating food.
- Belching, vomiting, or heartburn.
- Unpleasant odor from the mouth, the color of stool changes, and the stomach swells.
- Head pain, rapid heartbeat, high level of salivation.
- Chronic gastritis has symptoms that are more difficult to define (coated tongue, constipation, fatigue, bloating, diarrhea, abdominal noises while eating).
What diseases of the cardiovascular system and gastrointestinal tract mutually aggravate each other?
The combination of non-alcoholic fatty liver disease (fatty hepatosis) with heart and vascular diseases significantly increases the risk of developing cardiovascular accidents. Cardiovascular disease is the leading cause of death in patients with fatty liver disease.
In people with hypertension combined with non-alcoholic fatty liver disease, hypertension is unstable and may develop a form of hypertension that is resistant to treatment.
Erosive and ulcerative lesions of the stomach and duodenum are quite often complicated when taking drugs to prevent the formation of blood clots in the coronary arteries, which contain acetylsalicylic acid. They are prescribed for the treatment of coronary heart disease, angina pectoris, and myocardial infarction.
Pathological changes in the intestinal microflora are currently considered as an independent risk factor not only for intestinal diseases, but also for the development of lipid metabolism disorders, systemic inflammation, obesity and type 2 diabetes mellitus, which increase the risk of developing cardiovascular diseases and their complications.
When is it necessary to consult a cardiologist?
Regular monitoring of heart health is necessary for men after 40 years of age and women after 50 years of age. If there is an increased risk of cardiovascular diseases (with a hereditary predisposition, increased neuropsychic and physical stress, or low physical activity, smoking, increased cholesterol and blood sugar levels, obesity and liver steatosis), preventive examinations begin earlier.
In what cases should you consult a doctor:
- pain, burning or discomfort in the chest (sometimes constant tension in the chest is mistaken for stomach pain);
- shortness of breath and increased heart rate that occur with increased physical activity or at rest;
- feeling of palpitations, interruptions in heart rhythm;
- fatigue, dizziness, fainting;
- decrease or increase in pressure;
- swelling of the lower extremities.
The main disease of the stomach is chronic gastritis
And here you can’t do without the help of a doctor, and much more serious help will be needed. Each of us knows from our own experience what abdominal pain is. Sometimes the discomfort goes away on its own; other times we habitually reach for pills. However, if the pain comes back again and again, you should not self-medicate, because you need to look for the cause, and not relieve the symptoms, in which case it is better to trust a specialist. After all, pain in the stomach can be a sign of a number of diseases. The most common of these is gastritis.
Chronic gastritis is an inflammatory process of the gastric mucosa, one of the most common diseases of the gastrointestinal tract.
How to recognize the manifestations of gastritis? Chronic gastritis is an inflammatory process of the gastric mucosa, one of the most common diseases of the gastrointestinal tract.
With increased acidity, the aggressive properties of hydrochloric acid increase; with low acidity (hypoacid and anacid gastritis), food is retained in the stomach and fermentation processes intensify. Inflammation of the gastric mucosa causes the body to disrupt the process of digesting food. And this worsens the general condition of the body, reduces performance, causeless fatigue, weakness and other symptoms appear, which even the person himself for some reason ignores, not caring about the possible consequences.
The main manifestations of gastritis may be pain or discomfort, burning in the upper abdomen, heaviness after eating a small amount of food, an unpleasant taste in the mouth or belching “sour” or “rotten egg”, usually in the morning. However, after consuming food or liquid, symptoms may decrease somewhat. Other symptoms (which indicate involvement of the esophagus in the inflammatory process) include heartburn (a burning sensation behind the sternum), belching of air or recently eaten food, and sometimes nausea. If unpleasant sensations bother you constantly and do not go away for more than a week, you need to consult a doctor in order to determine the cause, establish a diagnosis and begin adequate treatment, which can help avoid unpleasant complications. Chronic gastritis can occur without symptoms - this picture is observed in approximately half of the people suffering from this disease.
To the question “What causes gastritis?” most will answer quite easily: poor diet, too much spicy food, smoking, drinking alcohol. Some will name stress and the use of certain medications. All this really influences the appearance of the disease. However, recent studies prove that most often all these factors are not the main ones. In approximately 85% of cases, the disease occurs “thanks to” the bacterium Helicobacter Pylori (Helicobacter) that lives in the stomach. This discovery at the end of the 20th century became one of the turning points in gastroenterology - after all, it was traditionally believed that it was impossible to “get infected” with gastritis.
Infection more often occurs within a family or other closely communicating groups, since the infection spreads when using the same utensils, failure to comply with hygiene rules, and overcrowding. Often the infection is transmitted from mother to child (through saliva that gets on the pacifier, spoon and other objects). You can become infected with Helicobacter pylori even by kissing. Bacteria in the stomach “sleep” indefinitely, and then at some point they begin to “act”, causing illness. Moreover, the probability of developing chronic gastritis if a person is infected before the age of 20 is more than 50%; in this case, he develops the so-called “Helicobacter gastritis”. Its peculiarity is that it is difficult to treat, provokes an increase in exacerbations of gastritis, and is highly likely to cause various complications, primarily ulcers and stomach cancer. If such an ulcer is treated with conventional means without destroying the bacteria, then the probability that it will occur again is extremely high and is close to 90% within the first year after the end of therapy. Therefore, it is necessary to approach the treatment, and therefore the removal from the body of the main enemy of the stomach - Helicobacter, very carefully and with all seriousness.
How to cope with gastritis?
First of all, you should remember: in the fight against Helicobacter pylori gastritis, almagel alone will not help, it is only a symptomatic remedy that will relieve discomfort for a short time: more serious remedies are needed here, moreover, prescribed by a doctor after a thorough examination.
It is desirable that this examination include all the necessary tests - instrumental (fibrogastroscopy - which allows you to fully determine the condition of the gastric mucosa and reliably detect the presence or absence of bacteria) and laboratory (breath test and blood test from a vein). Diagnosis of infection by blood test is less reliable, because it only determines the presence of antibodies to the bacterium - immune cells, and not Helicobacter itself. You need to perform either fibrogastroscopy or 2 methods, a breath test and a blood test. If the result is positive, it is necessary to eradicate the pathogen, that is, to cleanse the body of it. In this case, treatment regimens specially developed by the Society of Gastroenterologists are used.
In addition, the doctor will recommend a suitable diet - both during treatment and after it. A good addition to the tablets would be, in case of high acidity, the habit of not eating citrus fruits or drinking their juices, you should temporarily forget about chocolate and coffee, and do not abuse spicy foods and alcohol. With low acidity, food should not be very hot or cold, it should be chewed thoroughly. They recommend products that have a juice-containing effect (meat and vegetable decoctions, lean meat, fish, herring in small quantities, black caviar, herbs, vegetables, fruits, lactic acid products, for example, cottage cheese, preferably homemade, cheese, as well as juices, jam, etc. .).
It is easier to cure any disease in the early stages - before something serious happens. Therefore, if abdominal pain, even infrequently occurring and not severe, bothers you again and again, it’s time to contact a gastroenterologist who will help solve this problem. The sooner you start treatment, the better the effect you can get.