Sinus bradycardia - a decrease in heart rate to 60 beats per minute. This condition is not a pathology. It can be either a variant of the norm or a sign of a serious illness. Bradycardia is often observed in professional athletes. With regular exercise, the heart pumps blood more actively and provides the necessary blood flow through fewer contractions. In swimmers, skiers and track and field athletes, the resting heart rate can reach 30 beats per minute. In this case, this is not considered a deviation. However, if the heart rate is less than normal and other disturbing symptoms are observed, there is a reason to seek advice from a cardiologist.
What is "bradycardia"?
A decrease in heart rate (HR) below the established norm (60 beats per minute) is called “bradycardia”.
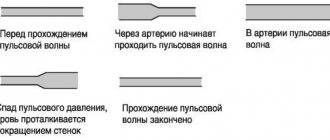
It can occur both in healthy people and in patients with various pathologies. Compared to tachycardia (increased heart rate more than 90 beats per minute), bradycardia is less common. It is typical for people over 60 years of age, since heart disease is more common at this age. Heart rate usually corresponds to the pulse, since with each release of blood into the aorta under pressure, rhythmic vibrations of the arterial walls occur.
What is the normal heart rate?
In adults, the heart rate should be 60–90 beats per minute (bpm); for children, normal heart rates depend on age. Thus, in babies under one year old, heart rate fluctuates between 100–170 beats/min. As the child grows up, normal heart rate values gradually decrease. By age 12–15, your resting heart rate should approach 70–90 beats per minute.
How to measure pulse?
The pulse can be measured by feeling the arteries that are located shallow to the surface of the skin and where they can be pressed against the bones. Then you can feel the movement of the vessel wall with your fingertips (Fig. 1). It occurs with every heartbeat. The pulse is measured in the following arteries: temporal, carotid, brachial, radial (at the wrist), femoral, popliteal, dorsalis pedis, posterior tibial (at the ankle of the foot).
Figure 1. How to measure pulse Source: MedPortal
Diagnostics
Conducted by a cardiologist. In the absence of data for a purely cardiac process, a neurologist may be involved.
Approximate list of events:
- Oral interview and history taking. Objectification of symptoms, drawing up a clinical picture.
- Measurement of blood pressure and heart rate. Blood pressure is normal, but heart rate drops. This is a typical but not required combination. The indicators exist separately.
- 24-hour Holter monitoring. Dynamic assessment of indicated vital levels over a 24-hour period. If necessary, it is prescribed repeatedly. It is considered the most informative methods of early diagnosis.
- Electrocardiography. Study of the functional activity of cardiac structures. Detects arrhythmias and other disorders.
- Echocardiography. Used to visualize defects and anatomical defects.
- MRI as needed
- EEG.
- Assessment of neurological status using routine methods. Including testing basic reflexes.
- General blood test, biochemical, hormones. In case of metabolic disorders or deviations in the level of specific substances, an endocrinologist is involved.
This is enough for early diagnosis.
Causes of bradycardia
A decrease in heart rate can occur not only with cardiac lesions, but also with non-cardiac pathologies. Common reasons for a decrease in heart rate include:
- coronary heart disease, heart defects, atherosclerotic cardiosclerosis, heart attack, myocarditis, cardiomyopathies, pericarditis;
- jaundice and kidney failure, in which toxins slow the heart's impulses;
- connective tissue diseases (rheumatism, rheumatoid arthritis, scleroderma, lupus erythematosus);
- hypothyroidism - decreased function of the thyroid gland;
- infections (diphtheria, borreliosis, syphilis, toxoplasmosis, viral hepatitis, etc.);
- disturbance of the electrolyte composition of the blood - decreased potassium levels and increased calcium;
- increased intracranial pressure due to brain tumors, stroke, trauma, developmental defects;
- lymphogranulomatosis, multiple myeloma, amyloidosis, sarcoidosis, hemochromatosis are conditions in which myocardial damage is possible.
Drug-induced bradycardia often occurs. This occurs when taking or overdosing on beta blockers, cardiac glycosides, calcium channel blockers, and antiarrhythmic drugs.
The heart rate is affected by the work of the nervous system: the parasympathetic system reduces the heart rate, and the sympathetic system increases it. Reflex bradycardia occurs as a result of the influence of the parasympathetic nervous system on the sinus node. The causes of such bradycardia may be:
- diseases of the nervous system;
- gastrointestinal pathology (peptic ulcer of the stomach and duodenum, cholecystitis, cholelithiasis);
- diseases of the esophagus and diaphragm;
- low body temperature, hypothermia;
- blow to the upper abdomen (up to cardiac arrest);
- pressure on the eyeballs or neck in the area of the carotid artery;
- cough, vomiting.
When the heart rate slows, blood pressure (BP) can be normal, high or low.
Bradycardia with high blood pressure is an uncommon occurrence. It is dangerous due to respiratory arrest, loss of consciousness, risk of blood clots, insufficient blood supply to the brain and heart with the development of stroke and heart attack. The combination of hypertension and bradycardia requires special treatment approaches so as not to aggravate the slowing of the rhythm.
For newborns (especially premature ones), bradycardia can occur against the background of apnea - stopping breathing for more than 20 seconds (Fig. 2). This occurs due to the immaturity of the nervous and muscle tissue of the newborn.
Figure 2. Bradycardia and apnea in infants. Source: MedPortal
Therapy methods
Therapeutic tactics depend on the underlying disease that caused the low pulse while maintaining normal blood pressure.
- Cardiac pathologies themselves are treated with medication. The operation is indicated for defects, atherosclerosis and malnutrition of the heart tissue. Drugs are selected with caution, tonic medications are prescribed.
- Endocrine abnormalities require replacement therapy or surgery (for tumors, etc.).
- Neurogenic factors are eliminated with sedatives based on herbal components. Like Motherwort. Valerian and others.
- Symptomatic therapy - prescribing Eleutherococcus tincture, Ginseng, caffeine-based products. Critical heart rate levels are corrected by Epinephrine and Adrenaline.
After normalization and discharge from the hospital, or a visit to a specialist, lifestyle changes are recommended.
Correction of the diet, in accordance with treatment table No. 10, giving up alcohol, cigarettes and tobacco products in general.
Moderate physical activity at the level of walking, swimming. If drugs are the cause of bradycardia, you need to consult a doctor and adjust the main course of therapy.
Classification of bradycardia
The work of the heart is impossible without the normal functioning of the conduction system. These are special muscle fibers that form nodes and bundles and provide coordinated contraction of the atria and ventricles of the heart. A normal rhythm is generated with a frequency of 60–90 per minute in the sinus node (SU), which is located in the right atrium. Along the internodal bundles, the electrical impulse is conducted to the atrioventricular node (atrioventricular - AV), located in the interatrial septum. From the AV node, the impulse goes directly to the muscles that provide contraction of the ventricles of the heart.
Depending on the mechanism of occurrence, bradycardia occurs:
- Sinus. Associated with a slowdown in impulse generation in the sinus node itself (Fig. 3).
- Sinoatrial, in which the transmission of impulses from the sinus to the atria is blocked.
- Atrioventricular, when there is a blockade of excitation transmission in the AV node.
Figure 3. Development of sinus bradycardia.
Source: mayoclinic.org Bradycardia can be pathological and physiological - a decrease in heart rate is typical for young athletes and during sleep. Pathological bradycardia occurs:
- acute and chronic;
- with symptoms and without clinical manifestations;
- cardiac and extracardiac (depending on the reasons).
Hypotension with VSD: how to treat nausea and dizziness in the morning
Dizziness and nausea with vegetative-vascular dystonia are associated with a sharp decrease in blood pressure. This is explained by the inadequate regulation of peripheral vascular tone, as well as venous insufficiency, which often accompanies VSD. It is difficult for a person with low blood pressure to maintain vigor and good health during the day; he has a particularly difficult time with hunger and thirst, is irritable, and inattentive. It takes a lot of effort for a hypotensive person to wake up in the morning and get out of bed. Our recommendations will help facilitate this process and improve your overall condition.
- Morning coffee is the most popular way to slightly increase blood pressure during hypotension. For people with VSD with frequent dizziness and weakness, doctors recommend two to three cups of coffee a day. If you don't have access to coffee, take one caffeine tablet. For arrhythmias and heart failure, which can also be accompanied by low blood pressure, coffee and products containing caffeine are contraindicated.
- Pouring your feet with cold water. You can tone up with a cold shower below your knees. A cold shower in your legs will help your veins contract and return more blood to your upper body, meaning you won't feel dizzy from low blood pressure. It's a pity that this simple method cannot help maintain normal blood pressure all day long. To reduce the likelihood of dizziness during the day with dystonia, regular cool foot baths in the morning and before bedtime are recommended.
- Gymnastics in bed. If morning exercises make you want to lie down as soon as possible, then exercises while lying in bed are what you need. Orthostatic collapse with VSD most often occurs immediately after waking up, when a person tries to jump up at the alarm clock. Several exercises in a lying position will activate blood circulation and restore muscle tone to the vessels of the legs. No tricks: lying on your back, stretch your arms and legs in opposite directions as hard as you can, rotate your feet, do the “bicycle” exercise for 30 seconds, roll over onto your stomach and bend your back, clasp your ankles with your hands and rock back and forth for 30 seconds, stretch forward first one hand, then the other. After this, sit on the bed and stay in this position for about a minute.
- Freshly squeezed orange juice immediately after waking up. This method is suitable if you have normal or reduced acidity of gastric juice. For frequent heartburn and stomach pain, drink 150-200 ml of water with a squeeze of lemon. This way you will immediately replenish your blood volume and it will be easier to keep your blood pressure at an acceptable level. Vitamin C from an orange (in smaller quantities from a lemon slice) activates the sympathoadrenal system, and the second mechanism of increasing blood pressure will work.
An increase in the level of glutathione in the body, a strong endogenous antioxidant, the deficiency of which is associated with the development of vegetative-vascular dystonia. You can activate the synthesis of glutathione by taking amino acids, from which it is formed as a result of a biochemical reaction inside cells: glutamic acid, cystine, glycine. The drug Eltacin® contains three essential amino acids in an optimal ratio and is recommended as the main medicine for dystonia.
Why is bradycardia dangerous?
A decrease in heart rate can cause heart failure, chronic attacks of bradycardia, and the formation of blood clots.
Heart failure
It rarely develops when the decrease in heart rate is significant (less than 40 per minute). Bradycardia results in insufficient cardiac output, which means that the heart can no longer supply oxygen to all organs and systems of the body at the proper level. In this case, the brain and the heart itself suffer first. The risk of developing coronary artery disease and myocardial infarction also increases, and fainting and cardiac arrest may occur.
Blood clots
With prolonged or frequently occurring bradycardia with an irregular rhythm, as a result of slowing down the movement of blood flow in the chambers of the heart, blood thickens and the gradual formation of blood clots occurs. When they enter the vessels of the brain or heart, strokes and heart attacks occur.
Chronic attacks of bradycardia
When the cause of bradycardia cannot be identified and eliminated, attacks occur that reduce the quality of life and are difficult to correct. During an attack, the patient experiences weakness, dizziness, and decreased performance. Sometimes fainting is possible.
Types of arrhythmias
There are many different types and forms of arrhythmias, but those that affect the ventricles are usually more serious than atrial problems. Arrhythmias can be caused by either a slow heartbeat (bradycardia) or a fast heartbeat (tachycardia) . A low heart rate can occur due to sick sinus syndrome. This occurs when the heart's natural pacemaker fails, causing the electrical signals that contract the heart to be transmitted more slowly. The condition is more common in older people and may be worsened by certain medications (such as beta blockers) that also slow the heart rate.
Heart block occurs when the electrical signal sent from the upper chambers of the heart (atria) to the lower chambers of the heart (ventricles) is interrupted. Without this signal transmission, the heart cannot contract effectively to pump blood to the body.
An increased heart rate may be the result of atrial fibrillation (AF). The arrhythmia clinic involves random signals that are fired in rapid succession. They cause fibrillation, which is an uncoordinated shaking of the muscular wall of the atria. It is often described as "heart cramps". The atria stop pumping blood effectively, but the ventricles receive enough blood for the heart to function. However, AFib is potentially dangerous because blood can pool in the atrium and lead to the formation of a clot. If one of these clots enters the brain, it causes a stroke. AF is the most common form of dangerous arrhythmia, affecting almost 1% of the population. It is more common in older people, affecting about 5% of the population over 69 years of age. One study showed that one in four people over 40 years of age develops FIP. Source: On the issue of classification of cardiac arrhythmias. Batyanov I.S., Batyanova E.I. Cardiovascular therapy and prevention, 2005.
Ventricular fibrillation (VF) is the most dangerous form of arrhythmia. The ventricles twitch but do not pump blood. If the twitching does not stop on its own or as a result of a defibrillator discharge, this complication of arrhythmia can be fatal.
Symptoms of bradycardia
Manifestations of bradycardia are caused by a lack of blood supply to vital organs: the brain, heart and lungs. Bradycardia can manifest itself (Fig. 4):
- decrease in blood pressure;
- presyncope and loss of consciousness;
- dizziness, headache;
- rapid fatigue;
- chest pain;
- shortness of breath and poor tolerance to any physical activity;
- pale skin.
Figure 4. Symptoms of bradycardia. Source: MedPortal
When to see a doctor?
If you have symptoms of bradycardia and a pulse less than 60 beats per minute, you should consult a physician or cardiologist. The doctor will determine the causes of this condition and prescribe effective treatment.
Not all bradycardia causes symptoms. However, low heart rates cannot be ignored. A repeated decrease in heart rate is the “first bell” that will force the timely diagnosis of heart disease and non-cardiac pathology, and prevent the development of dangerous complications.
Diagnosis of bradycardia
Only a doctor can differentiate physiological or pathological bradycardia. To do this, he uses several diagnostic methods.
Auscultation
A simple diagnostic method is to listen to the heart using a phonendoscope. Auscultation of the heart allows not only to determine a rare rhythm, but also to suspect certain diseases of the cardiovascular system.
Electrocardiography
ECG is a method of instrumental diagnostics of the heart, which records not only heart rate, but also helps to diagnose cardiac causes of bradycardia (myocardial ischemia and infarction, sinus node pathology, AV block). This is important for effective therapy. In some cases, daily ECG monitoring is necessary - a Holter study.
Phonocardiography
Phonocardiography (PCG) is a method of hardware diagnostics of sound phenomena that are created during the work of the heart. The study is carried out in conjunction with an ECG. At the same time, the heart sounds that are created during the operation of the valves, as well as additional noise, are assessed.
To diagnose the causes of bradycardia, the doctor may also prescribe:
- EchoCG - ultrasound examination of the heart;
- blood test for markers of damage to the heart muscle (troponins, creatine kinase);
- study of inflammation indicators (C-reactive protein, rheumatic tests, markers of collagenosis);
- blood test for thyroid function indicators (TSH, T4, T3);
- study of blood electrolytes (potassium, magnesium, calcium, sodium);
- biochemical blood test (glucose, bilirubin, cholesterol, creatinine, etc.).
First aid for an arrhythmia attack
Defibrillators are devices that restart blocked heart muscles by delivering electricity to the chest. Defibrillators are effective in stopping the heart from ventricular fibrillation, but because ventricular fibrillation can be fatal in less than 4 minutes, they should be used as soon as possible. Most defibrillators are external devices, but there are now automated implantable cardioverter/defibrillators (AICDs). These devices can be as large as pacemakers. They can detect dangerous fibrillation and return the heart to normal before any damage is done.
Article sources:
- "New Theory of Arrhythmia" clarifies the causes of arrhythmia. Ermoshkin V.I. Educational bulletin “Consciousness”, 2015. p. 22-30
- Innovations in the treatment of cardiac arrhythmia. Zh.A. Arzykulov, A.A. Omarov, B.B. Kituev, F.A. Tursunova, A.A. Yeshtay, N.G. Pavlova. Bulletin of Surgery of Kazakhstan, 2012. p. 4-5
- On the issue of classification of cardiac arrhythmias. Batyanov I.S., Batyanova E.I. Cardiovascular therapy and prevention, 2005
- A look from the inside focuses on a patient with arrhythmia. Boqueria O.L. Annals of Arrhythmology, 2014. p. 196-199
- Cardiac arrhythmias from the point of view of their dimension. Ubiennykh A.G. Measurement. Monitoring. Control. Control, 2021. p. 70-76
- Epidemiology of arrhythmias (review of literature data). Zatonskaya E.V., Matyushin G.V., Gogolashvili N.G., Novgorodtseva N.N. Siberian Medical Review, 2021. p. 5-16
Treatment of bradycardia
Not all bradycardia requires treatment. Only a doctor can determine the need for treatment by excluding physiological causes of a decrease in heart rate.
Conservative treatment
For conservative treatment use:
- anticholinergics - drugs that prevent the influence of the parasympathetic nervous system on the heart;
- adrenaline analogues - drugs that stimulate heart rate;
- antiarrhythmic drugs.
Treatment is carried out with tablets and injections. Their doctor can prescribe them occasionally during attacks and for a long time.
Surgery
In cases where conservative treatment is ineffective or there is damage to the conduction system of the heart, surgical treatment is indicated - installation of an electrical pacemaker (pacemaker). This is an electronic device that is implanted subcutaneously in the left subclavian region and sets the necessary rhythm to the heart through electrodes (Fig. 5). The pacemaker not only stimulates impulses to contract the heart, but also controls its natural electrical activity.
Figure 5. Installation of a pacemaker for bradycardia. Source: MedPortal
Treatment with folk remedies
To treat bradycardia at home, infusions of herbs are mainly used, which reduce the tone of the parasympathetic nervous system, increase myocardial contractions, and maintain blood pressure. These are Chinese lemongrass, tartar, immortelle, yarrow, walnuts, a mixture of lemon, honey and garlic and others.
Important! Treatment with folk remedies should be carried out very carefully and only after consultation with a doctor. It is possible with mild degrees of bradycardia (heart rate of at least 40), in the absence of complications and manifestations such as fainting, shortness of breath, dizziness, chest pain.
Modern methods of treatment
In some cases, arrhythmias occur due to bad habits, such as drinking too much alcohol. Giving up the habit will be a real help for arrhythmia. Reducing stress, avoiding caffeine, improving diet, and increasing the amount of exercise the patient does during the week can also reduce the incidence of arrhythmias. Before you begin making these changes, you should first talk to your doctor. For others, arrhythmias are a symptom of heart disease and will not go away unless the underlying problem is addressed. Fortunately, many people can benefit from invasive treatment of cardiac arrhythmias using modern medical interventions, especially surgery and special electrical devices.
Drug treatment for cardiac arrhythmia is also possible. There are several medications that can slow a fast heartbeat (known as "antiarrhythmic drugs"). Beta blockers are medications that are very useful in controlling heart rate in people with various heart conditions. Calcium channel blockers may also be used to control heart rate. Often these drugs can be used for more than one purpose (eg, to control heart rate, high blood pressure, protect the heart after a heart attack). The drug Digoxin is derived from a substance called Digitalis, which has been used for arrhythmias for over 200 years.
Other medications called antiarrhythmics can convert the abnormal rhythm to a normal one and prevent seizures from recurring (known as "rhythm control"). Patients with atrial fibrillation (AF) are usually prescribed the anticoagulant Warfarin, which thins the blood and prevents blood clots and strokes. Recent studies have shown that heart rate control and adequate anticoagulation are very important (perhaps even more important than rhythm control) for people with certain types of arrhythmias (eg, AF).
In some cases, AF returns to a normal rhythm with a treatment called cardioversion. The patient is given a small electrical shock that resets the heart's natural pacemakerSource: Innovations in the Treatment of Cardiac Arrhythmia. Zh.A. Arzykulov, A.A. Omarov, B.B. Kituev, F.A. Tursunova, A.A. Yeshtay, N.G. Pavlova. Bulletin of Surgery of Kazakhstan, 2012. p. 4-5.
Many arrhythmias can be completely treated with radiofrequency ablation. Thin catheters are passed into the heart to send radio waves directly to electrical pathways carrying inappropriate signals. These waves destroy abnormal tissue, preventing it from causing abnormal heart rhythms. Artificial pacemakers can take over the job of generating electrical signals. They are not limited to treating low heart rates, newer pacemakers can also control high heart rates. They can operate for up to 15 years on a single battery to prevent heart arrhythmia. Some save energy by turning off when the heartbeat is normal. Most units are placed under the skin, requiring only minor surgery.
Prevention
To prevent complications of bradycardia, you need to consult a specialist as soon as possible if your pulse decreases and heart rate is less than 60, and undergo a full examination to identify the causes of the condition. It is equally important to strictly follow your doctor's recommendations for treating episodic or prolonged bradycardia.
To prevent bradycardia, it is necessary to adhere to a lifestyle that reduces the risk of heart disease:
- stop smoking and drinking alcohol;
- eat well: limit animal fats, salt, caloric content of food should correspond to energy costs;
- reduce excess weight if you are overweight;
- avoid nervous stress;
- normalize blood pressure.
How to restore your pulse
The simplest methods of stabilization:
- thermoregulation – wear warm clothes in cold weather and try to avoid overheating in hot weather;
- healthy sleep at the right time of day;
- walk more.
Among the slightly less easy to use, but very useful methods:
- drinking tonic drinks – green and black tea, coffee. But make sure that the pressure does not jump because of them;
- spicy and sweet foods, like bitter dark chocolate or black pepper. But this should not be used for diabetes and stomach diseases;
- hot showers and baths are among the most pleasant and least dangerous methods. If you want to improve the water, you can add sea salt or essential oils, and the nervous system will feel better;
- light massage – older people should massage their temples, ears, feet, and back of the head. This will not cause harm, but will improve the heartbeat;
- alcohol - yes, under certain circumstances it can be useful, but only with careful adherence to the measure and dosage, and also in the absence of contraindications. Increase your pulse with fifty ml of wine or twenty-five ml of good cognac.