External structure of the heart
The heart (cor) has the shape of a truncated cone, which is located in the anterior mediastinum with the apex to the left and down. The apex of this cone has the anatomical name "apex cordis", so you won't get confused. Look at the illustration and remember - the top of the heart is at the bottom, not at the top.
The top of the heart is called the base of the heart (basis cordis). You can show the base of the heart on the specimen if you simply circle the area into which all the major vessels of the heart enter and exit. This line is quite conventional - as a rule, it is drawn through the opening for the inferior vena cava.
The heart has four surfaces:
- Diaphragmatic surface (facies diaphragmatica). Located below, it is this surface of the heart that is directed towards the diaphragm;
- The sternocostal surface (facies sternocostalis). This is the anterior surface of the heart, it faces the sternum and ribs;
- Pulmonary surface (facies pulmonalis). The heart has two pulmonary surfaces - right and left.
In this picture we see the heart in combination with the lungs. Here is the sternocostal, that is, the anterior surface of the heart.
There are small projections at the base of the sternocostal surface. These are the right and left appendages (auricula dextra / auricula sinistra). I highlighted the right ear in green, and the left ear in blue.
Anatomy of the Human Heart - information:
The heart, cor , is a hollow muscular organ that receives blood from the venous trunks flowing into it and drives the blood into the arterial system.
The heart cavity is divided into 4 chambers: 2 atria and 2 ventricles.
The left atrium and left ventricle together constitute the left, or arterial, heart according to the properties of the blood in it; the right atrium and right ventricle make up the right, or venous, heart. The contraction of the walls of the heart chambers is called systole, and their relaxation is called diastole.
The heart has the shape of a somewhat flattened cone. It distinguishes between the top, apex, base, basis, anterior-superior and lower surfaces and two edges - right and left, separating these surfaces. The rounded apex of the heart, apex cordis, faces down, forward and to the left, reaching the fifth intercostal space at a distance of 8-9 cm to the left of the midline; the apex of the heart is formed entirely by the left ventricle. The base, basis cordis, faces upward, backward and to the right. It is formed by the atria, and in front by the aorta and pulmonary trunk. In the upper right corner of the quadrangle formed by the atria, there is the entry point of the superior vena cava, in the lower - the inferior vena cava; Now, to the left are the entry points of the two right pulmonary veins, and on the left edge of the base are the two left pulmonary veins.
The anterior, or sternocostal, surface of the heart, facies sternocostalis , faces anteriorly, upward and to the left and lies behind the body of the sternum and the cartilages of the ribs from III to VI. The coronary groove, sulcus corondrius, which runs transversely to the longitudinal axis of the heart and separates the atria from the ventricles, divides the heart into an upper section formed by the atria and a larger lower section formed by the ventricles. The anterior longitudinal groove, sulcus interventricularis anterior, running along the facies sternocostalis, runs along the border between the ventricles, with most of the anterior surface formed by the right ventricle, and a smaller part by the left.
The lower, or diaphragmatic, surface, facies diaphragmatica , is adjacent to the diaphragm, to its tendon center. A posterior longitudinal groove, sulcus interventricularis posterior, runs along it, which separates the surface of the left ventricle (larger) from the surface of the right (smaller). The anterior and posterior interventricular grooves of the heart merge with each other at their lower ends and form on the right edge of the heart, immediately to the right of the apex of the heart, the cardiac notch, incisura apicis cordis. The edges of the heart, right and left, are of unequal configuration: the right is sharper; the left edge is rounded, more blunt due to the greater thickness of the wall of the left ventricle.
It is believed that the heart is equal in size to the corresponding individual's fist. Its average dimensions are: length 12-13 cm, largest diameter 9-10.5 cm, anteroposterior size 6-7 cm. The weight of the heart of a man is on average 300 g (1/215 of body weight), of a woman - 220 g (1/250 body weight).
Innervation of the heart. Afferent pathways from the heart consist of n. vagus, as well as in the middle and lower cervical and thoracic cardiac sympathetic nerves. In this case, the feeling of pain is carried through the sympathetic nerves, and all other afferent impulses are carried through the parasympathetic nerves.
Efferent parasympathetic innervation.
- Preganglionic fibers begin in the dorsal autonomic nucleus of the vagus nerve and go as part of the latter, its cardiac branches (rami cardiaci n. vagi) and cardiac plexuses to the internal nodes of the heart, as well as the nodes of the pericardial fields.
- Postganglionic fibers extend from these nodes to the heart muscle.
Function: inhibition and suppression of cardiac activity; narrowing of the coronary arteries.
Efferent sympathetic innervation.
- Preganglionic fibers begin from the lateral horns of the spinal cord of the 4-5 upper thoracic segments, exit as part of the corresponding rami communicantes albi and pass through the sympathetic trunk to the five upper thoracic and three cervical nodes. In these nodes, postganglionic fibers begin, which are part of the cardiac nerves, nn. cardiaci cervicales superior, medius et inferior and nn. cardiaci thoracici, reach the heart muscle. The break is carried out only in the ganglion stellatum. Cardiac nerves contain preganglionic fibers, which switch to postganglionic fibers in the cells of the cardiac plexus.
Function: strengthening the work of the heart.
Chambers of the heart
The heart is a hollow (that is, empty from the inside) organ. It is a bag of dense muscle tissue, which has four cavities:
- Right atrium (atrium dexter);
- Right ventricle (ventriculus dexter);
- Left atrium (atrium sinister);
- Left ventricle (ventriculus sinister).
These cavities are also called the chambers of the heart. The human heart has four cavities, that is, four chambers. That is why they say that a person has a four-chambered heart .
On a heart that is cut in the frontal plane, I highlighted the boundaries of the right atrium in yellow, the left preseries in green, the right ventricle in blue, and the left ventricle in black.
Right atrium
The right atrium collects “ dirty ” (that is, rich in carbon dioxide and poor in oxygen) blood from throughout the body. The upper (brown) and lower (yellow) complete veins flow into the right atrium, which collect blood with carbon dioxide from the entire body, as well as the great vein of the heart (green), which collects blood with carbon dioxide from the heart itself. Accordingly, three openings open into the right atrium.
Between the right and left atria there is an interventricular septum. It contains an oval depression - a small oval-shaped depression, an oval fossa (fossa ovalis). In the embryonic period, in place of this depression there was an oval hole (foramen ovale cordis). Normally, the foramen ovale begins to close immediately after birth. In this picture, the oval fossa is highlighted in blue:
The right atrium communicates with the right ventricle through the right atrioventricular orifice (ostium atrioventriculare dextrum). The flow of blood through this opening is controlled by the tricuspid valve.
Right ventricle
This cavity of the heart receives “dirty” blood from the left atrium and sends it to the lungs to be cleaned of carbon dioxide and enriched with oxygen. Accordingly, the right ventricle connects to the pulmonary trunk, through which blood will be sent to the lungs.
The tricuspid valve, which must be closed during the reflux of blood into the pulmonary trunk, is fixed by tendon threads to the papillary muscles. It is the contraction and relaxation of these muscles that controls the operation of the tricuspid valve.
The papillary muscles are highlighted in green, and the tendon filaments are highlighted in yellow:
Left atrium
This part of the heart collects the “ purest ” blood. It is into the left atrium that fresh blood flows, which is first purified in the small (pulmonary) circle from carbon dioxide and saturated with oxygen.
Therefore, four pulmonary veins flow into the left atrium - two from each lung. You can see these holes in the picture - I've highlighted them in green. We remember that arterial passes veins .
The left atrium communicates with the left ventricle through the left atrioventricular orifice (ostium atrioventriculare sinistrum). The flow of blood through this opening is regulated by the mitral valve.
Left ventricle
The left ventricle begins the systemic circulation . When the left ventricle pumps blood into the aorta, it is isolated from the left atrium by the mitral valve. Just like the tricuspid valve, the mitral valve is controlled by papillary muscles (highlighted in green), which are connected to it by tendon strands.
You may notice the very strong muscular wall of the left ventricle. This is explained by the fact that the left ventricle needs to pump a powerful flow of blood, which must be sent not only in the direction of gravity (to the stomach and legs), but also against gravity - that is, upward , to the neck and head.
Can you imagine how cunningly the circulatory system of giraffes is designed, in which the heart must pump blood all the way up the neck to the head?
Septa and grooves of the heart
The left and right ventricles are separated by a thick muscular wall. This wall is called the interventricular septum (septum interventriculare).
The interventricular septum is located inside the heart. But its location corresponds to the interventricular grooves that you can see from the outside. The anterior interventricular groove is located on the sternocostal surface of the heart . I have highlighted this furrow in green in the figure.
On the diaphragmatic surface of the heart is the posterior interventricular groove (sulcus interventricularis posterior). It is highlighted in green and indicated by the number 13.
The left and right atria are separated by the interatrial septum (septum interatriale), also highlighted in green.
From the outer part of the heart, the ventricles are separated from the atria by the coronary groove (sulcus coronarius). In the figure below you can see the coronary groove on the diaphragmatic, that is, the posterior surface of the heart. This groove is an important landmark for identifying the large vessels of the heart, which we will discuss later.
Circulation circles
Big
The powerful, large left ventricle launches arterial blood into the aorta - this is where the systemic circulation begins. It looks like this: blood is ejected from the left ventricle into the aorta, which branches into organ arteries. Then the caliber of the vessels becomes smaller and smaller, down to the smallest arterioles that approach the capillaries.
Gas exchange occurs in the capillaries, and the blood, already saturated with carbon dioxide and decay products, rushes back to the heart through the veins. After the capillaries, these are small venules, then larger organ veins that flow into the inferior vena cava (if we are talking about the torso and lower extremities) and into the superior vena cava (if we are talking about the head, neck and upper extremities).
In this figure, I have highlighted the anatomical formations that complete the systemic circulation. The superior vena cava (green, number 1) and the inferior vena cava (orange, number 3) drain into the right atrium (magenta, number 2). The place where the vena cava enters the right atrium is called the sinus vena cava (sinus venarum cavarum).
Thus, the great circle begins with the left ventricle and ends with the right atrium:
Left ventricle → Aorta → Large main arteries → Organ arteries → Small arterioles → Capillaries (gas exchange zone) → Small venules → Organ veins → Inferior vena cava/Superior vena cava → Right atrium.
When I was preparing this article, I found a diagram that I drew in my second year. It will probably show you the systemic circulation more clearly:
Small
The pulmonary (pulmonary) circulation begins with the right ventricle, which sends venous blood to the pulmonary trunk. Venous blood (be careful, this is venous blood !) is sent along the pulmonary trunk, which is divided into two pulmonary arteries. According to the lobes and segments of the lungs, the pulmonary arteries (remember that they carry venous blood) are divided into lobar, segmental and subsegmental pulmonary arteries. Ultimately, the branches of the subsegmental pulmonary arteries break up into capillaries that approach the alveoli.
Gas exchange occurs again in the capillaries . Venous blood, saturated with carbon dioxide, gets rid of this ballast and is saturated with life-giving oxygen. When the blood is saturated with oxygen, it becomes arterial . After this saturation, fresh arterial blood runs through the pulmonary venules, subsegmental and segmental veins, which drain into the large pulmonary veins. The pulmonary veins drain into the left atrium.
Here I have highlighted the beginning of the pulmonary circulation - the cavity of the right ventricle (yellow) and the pulmonary trunk (green), which leaves the heart and is divided into the right and left pulmonary arteries.
In this diagram you can see the pulmonary veins (green) flowing into the cavity of the left atrium (purple) - it is these anatomical formations that complete the pulmonary circulation.
Diagram of the pulmonary circulation:
Right ventricle → Pulmonary trunk → Pulmonary arteries (right and left) with venous blood → Lobar arteries of each lung → Segmental arteries of each lung → Subsegmental arteries of each lung → Pulmonary capillaries (entangle the alveoli, gas exchange zone) → Subsegmental/segmental/lobar veins (with arterial blood) → Pulmonary veins (with arterial blood) → Left atrium
Hello student
circulatory system of the heart
The activity of the heart, associated with large expenditures of energy, is ensured by a developed system of its own blood vessels, through which approximately 10% of all blood distilled in systole is pumped.
All superficial vessels are located subepicardially. Slightly convoluted vessels are surrounded by adipose tissue, the amount of which depends on the fatness of the animal. From all superficial vessels into the myocardium, branches extend at right angles, turning into a very dense capillary network. The capillaries of neighboring areas intersect with each other, but do not connect. Thus, the branches of the cardiac arteries are the terminal arteries responsible for the blood supply to a certain area, which, if the corresponding artery is blocked, does not receive blood (=infarction). ARTERIES
The blood supply to the muscles of the heart is carried out through two large arteries that arise from the aorta directly above the semilunar valve. In accordance with the topography of the initial sections, they are called coronary arteries, aa. coronariae
Left coronary artery, a. coronaria sinistra, after reaching the coronal sulcus, divides into two main branches. Its interventricular paraconal branch, ramus interventricularis paraccmalis, runs in the groove of the same name to the apex of the heart, and the circumferential, or circumflex, branch, ramus circumflexus, is located in the left section of the coronary sulcus.
From the interventricular paraconal branch in cats and dogs, proximal and distal collateral branches, rami collaterales proximalis et distalis, depart to the auricular surface of the left ventricle; in the cat, an angular branch, ramus angularis, still extends in front of these branches. Proximal and distal collateral branches supply blood to the cushion papillary muscle. In the cat, the interventricular paraconal branch additionally gives off into the wall of the right ventricle a branch of the conus arteriosus, ramus coni arteriosi, as well as several small branches into the areas of the interventricular septum along the paraconal interventricular groove. The blood supply to most of the interventricular septum, atrioventricular node and atrioventricular bundle is carried out through a branch of the interventricular septum, ramus septi interventricularis, which also supplies the mastoid muscles of the right ventricle.
Rice. 11. Base of a dog's heart after removal of the atria. Large arteries and veins are depicted separately, small ones together (according to Liicke, 1955) a. b, with valva aortae: a valvula semilunaris sinistra, b valvula semilunaris dextra, with valvula semilunaris septalis; d, e, f valva trunci pulmonalis: d valvula semilunaris sinistra, e valvula semilunaris dextra, f valvula semilunaris intermedia; g, h valva atrioventricularis sinistra s. bicuspidalis: g cuspis septalis, h cuspis parietalis; i, k, I valva atrioventricularis dextra s. tricuspidalis: i cuspis septalib, k cuspis parietalis, l cuspis annularis; m septum interatrialc; n conus arteriosus; o margo ventricularis dexter; p margo ventricularis sinister; q sulcus interventricularis paraconalis; r sulcus interventricularis subsinuosus
1 a. coronaria sinistra; 2 ramus interventricularis paraconalis; 3 ramus col lateral Is proxi-malb, 4 ramus circumflexus; 5 ramus proximalis ventnculi sinistri; 6 ramus marginis ventriculi sinistri; 7 ramus et v. distalis ventnculi sinistri; 8 ramus interventricularis subsinuosus; 9 a. coronaria dextra, ramus circumflexus: 10 ramus et v. coni arteriosi; 11 ramus et v. proximalis ventriculi dextri; 12 ramus et v nuirginis ventriculi dextri; 13 ramus et v. distalis ventriculi dextri; 14 ramus attrii dextri; 15 ostium sinus coronarius; 16 sinus coronarius; 17 v. cordis media; 18 v. cordis magna; 19 v. interventricularis paraconalis; 20 v. obliqua atria sinistri
Rice. 12. Auricular surface of the dog’s heart. Large arteries and veins are indicated separately, small ones together (according to Liicke, 1955)
auricula cordis dextra; b auricula cordis sinistra; with atrium sinistrum; d margo ventricularis dexter; e margo ventricularis sinister; f ventriculus dexter; g ventriculus sinister; h sulcus interventricularis paraconalis; i conus arteriosus; k sulcus coronarius; I apex cordis; m incisura apicis cordis 1 arcus aortae; 2 a subclavia sinistra; 3 truncus brachio-cephalicus; 4 truncus pulmonalis: 5 a. pulmonalis sinistra; 6 vv pulmonales; 7 v. cava cranialis; 8 a. coronaria sinistra, 9 her ramus circumflexus, 10 her ramus interventricularis paraconalis, 11 her ramus collaterals proximalis, 12 her ramus collateralis distalis; 13 ramus proximalis ventriculi sinistri, 14 ramus marginis ventriculi sinistri; 15 a.m. coronaria dextra, ramus circumflexus; 16 a.m. et v. coni arteriosi; 17 ramus et v. proximalis ventriculi dextri; 18 v. cordis magna; 19 v. interventricularis paraconalis; 20 v. proximalis atrii sinistri; 21 v. intermedia atria sinistri
Rice. 13. Atrial surface of the dog’s heart. Large arteries and veins are indicated separately, small ones together (according to Lucke, 1955)
a atrium sinistrum; b atrium dextrum; with sinus venarum cavarum; d ventriculus sinister; e ventriculus dexter; f margo ventricularis sinister; g margo ventricularis dexter; h sulcus interventricularis subsinuosus; i, k sulcus coronarius; l apex cordis; m incisura apicis cordis 1 arcus aortae; 2 a. subclavia sinistra; 3 truncus brachio-cephalicus; 4 a. pulmonalis dextra, 5 a pulmonalis sinistra; 6 w pulmonales dextrae, 7 vv. pulmonales; 8 v cava caudalis; 9 v. cava cranialis; 10 v. azvgos dextra; 11 sinus coronarius et a. coronaria sinistra, ramus circumflexus; 12 ramus interventricularis subsinuosus and v. cordis media, 13 ramus et v. distalis ventriculi sinistri; 14 v. ventriculi dextri; 15 ramus distalis atrii sinistri; 16 a.m. coronaria dextra, ramus circumflexus; 17 ramus et v. marginis ventriculi dextri; 18 ramus distalis ventriculi dextri; 19. 20 rami distales atrii dextri; 21 ramus intermedius attrii dextri
Rice. 14. Base of the cat's heart after removal of the atria (approximately 1.5 times magnification) (after Habermehl, 1959)
a, b, c valva aortae: a valvula semilunaris sinistra, b valvula semilunaris dextra, c valvula semilunaris septalis; d, e, f valva trunci pulmonalis: d valvula semilunaris sinistra, e valvula semilunaris dextra, f valvula semilunaris intermedia; g, h valva atrioventricularis sinistra s. bicuspidalis: g cuspis septalis, h cuspis parietalis; i, k, I valva atrioventricularis dextra s. tricuspidalis: i cuspis septalis, k cuspis parietalis, I cuspis angularis; m septum interatriale; n conus arteriosus;
o margo ventricularis dexter; p margo ventricularis sinister; q sulcus interventricularis paraconalis; r sulcus interventricularis subsinuosus 1 a. coronaria sinistra, 2 a. coronaria sinistra, ramus interventricularis paraconalis, 3 a. coronaria sinistra, ramus circumflexus; 4 ramus et v. angularis; 5 ramus et v proximalis ventriculi sinistri; 6 ramus et v. marginis ventriculi sinistri; 7 ramus et v. distalis ventriculi sinistri; 8 ramus proximalis atrii sinistri; 9 a. coronaria dextra, 9′ her ramus circumflexus; 10 a.m. et v. coni arteriosi; 11 ramus et v. proximalis ventriculi dextri; 12 ramus et v. marginis ventriculi dextri; 13 ramus et v distalis ventriculi dextri; 14 ramus distalis atrii dextri, 15 ramus mtermedius atrii dextri; 16 ramus proximalis atrii dextri; 17 sinus coronarius; 18 v. cordis magna; 19 v. interventricularis paraconalis; 20 v. obliqua atria sinistri; 21 v. cordis media; 22 a.m. coronaria sinistra, ramus interventricularis subsinuosus; 23 ramus distalis atrii sinistri; 24 ramus intermedius attrii sinistri
Rice. 15. Arteries and veins of the auricular surface of the cat’s heart (approximately 1.5 times magnification) (after Habermehl, 1959)
A auricula cordis dextra; B auricula cordis sinistra, partially removed;
With margo ventricularis dexter; D margo ventricularis sinister; E ventriculus dexter; F ventriculus sinister; With sulcus interventricularis paraconalis; H conus arteriosus; J sulcus coronarius; To apex cordis; L incisura apicis cordis
a arcus aortae; b truncus brachiocephalicus; ca subclavia sinistra; d truncus pulmonalis; e vv. pulmonales sinis-trae; f v. cava cranialis; g v. azvgos dextra
1 a. coronaria sinistra, 2 its ramus interventricularis paraconalis, 3 its ramus circumflexus; 4 ramus angularis et v. angularis; 5 ramus et v. proximalis ventriculi sinistri; 6 ramus et v. marginis ventriculi sinistri; 7 ramus et v. collatcralis proximalis; 8 ramus et v. collateralis distalis; 9 a. coronaria dextra, ramus coni arteriosi et v. coni arteriosi; 10 ramus et v proximalis ventriculi dextri; 11 ramus et v. coni arteriosi; 12 v. cordis magna; 13 v. interventricularis paraconalis
Rice. 16. Arteries and veins of the atrial surface of the cat’s heart (approximately 1.5 times magnification) (after Habermehl, 1959)
A atrium dex trum; In atrium sinistrum; C marge) ventricularis dexter; D margo ventricularis sinister; E ventriculus dexter; F ventriculus sinister; With sulcus inter-ventriculans subsinuosus. H sinus venarum cavarum; J auricula cordis dextra; To apex cordis a arcus aortae; b truncus brachiocephalicus; with a. subclavia sinistra; d branches of truncus pulmonalis; e vv. pulmonales; f v. cava caudalis. gv cava cranialis; hv azygos dextra
1 a. coronaria sinistra, ramus circumflexus, 2 a. coronaria sinistra, ramus interventricularis subsinuosus; 3 ramus et v. distalis ventriculi sinistri; 4 ramus et v marginis ventriculi sinistri; 5 ra mus distalis atrii sinistri; 6 a. coronaria dextra. ramus circumflexus; 7 ramus et v. marginis ventriculi dextri; 8 ramus distalis ventriculi dextri; 9 ramus intermedius atrii dextri; 10 ramus distalis atrii dextri; 11 v. semicircumflexa dextra; 12 sinus coronarius, 13 v. cordis media; 14 v. cordis magna; 15 v. obliqua atrii sinistri or ramus intermedius atrii sinistri; 16 v. collateralis dextra proximalis
The circumferential branch, ramus circumflexus, runs in the coronary sulcus towards the subsinus interventricular sulcus. In the initial part it is covered with the left ear. In the dog, the circumferential branch passes into the subsinus interventricular branch, ramus interventricularis subsinuosus, which extends to the apex of the heart.
Along the course of the circumferential branch, several smaller branches are separated from it into adjacent areas of the interventricular septum of the left ventricular wall. Three main branches - the proximal, marginal and distal branches of the left ventricle, ramus proximalis, ramus marginalis et ramus distalis ventriculi sinistri - provide blood supply to the wall of the left ventricle. Other vessels arising from the circumferential branch of the left coronary artery supply blood to the wall of the left atrium and partially to the interatrial septum. These are the proximal, intermediate and distal branches of the left atrium, rami proximales, intermedii et distales atrii sinistri.
The subsinus interventricular branch, ramus interventricularis subsinuosus, in dogs, as a rule, also arises from the left coronary artery. Through small vessels extending to the sides, it supplies blood to the area along the subsinus interventricular groove, and the stripe on the wall of the right ventricle is wider than on the wall of the left ventricle.
In cats, this vessel only in about half of all examined cases originated from the left coronary artery and in approximately 30% from the right coronary artery. In the first case we are talking about the left coronary, in the second about the average, or uniform, type of blood supply to the heart. In addition to these types of blood supply, a cat also has a third, in which blood enters through two subsinus interventricular branches, rami interventriculares subsinuosi, extending from the right and left coronary arteries.
Right coronary artery, a. coronaria dextra, in the dog it has only a circumferential branch, ramus circumflexus, which runs in the right coronary groove under the right ear and ends on the atrial surface, not reaching the subsinus interventricular groove. In cats, the same picture is observed with the left coronal type of blood supply. With an average type of blood supply, the right coronary artery continues in the form of a subsinus interventricular branch, ramus interventricularis subsinuosus, to the apex of the heart.
The circumferential branch of the right coronary artery in carnivores, along with small branches, gives off four large vessels to the wall of the right ventricle. These are the branch of the conus arteriosus, ramus coni arteriosi, and the proximal, marginal and distal branches of the right ventricle, ramus proximalis, ramus marginalis et ramus distalis ventriculi dextri.
With an average type of blood supply in a cat, the subsinus interventricular branch vascularizes the walls of both ventricles with small branches, and the branch of the interventricular septum, ramus septi interventricularis, also vascularizes the interventricular septum.
The proximal, intermediate and distal branches of the right atrium, rami proximales, intermedii et distales atrii dextri, which supply blood to the interatrial septum, extend into the right atrium from the right coronary artery.
VIENNS
For didactic reasons, the description of the cardiac veins, venae cordis, is given in the direction opposite to the blood flow. From the coronary sinus, sinus coronarius, which is a short large vessel for collecting most of the venous blood, the middle cardiac vein, v., first departs. cordis media. It runs along the subsinus interventricular groove and, dividing into several branches, reaches the apex of the heart, where it anastomoses with the branches of the paraconal interventricular vein, v. interventricularis paraconalis. Due to the fact that the middle cardiac vein runs parallel to the subsinous interventricular branch of the left coronary artery, it is also called the subsinous interventricular vein, v. interventricularis subsinuosa. A branch extends from it into the wall of the right ventricle. In a cat, this is the powerful right proximal collateral vein, v. collateralis proximalis dextra, in a dog - a much smaller vein of the right ventricle, v. ventriculi dextri. Other vessels arising from the coronary sinus at approximately the same level are the oblique vein of the left atrium, v. obliqua atrii sinistri, and distal vein of the left ventricle, v. distalis ventriculi sinistri. The first is in carnivores a rudiment of the left azygos vein, v. azygos sinistra, and collects blood from the wall of the left atrium. The distal vein of the left ventricle is connected to the same area as the branch of the same name of the left coronary artery.
The continuation of the coronary sinus is the great cardiac vein v. cordis is mean. It passes along with the circumferential branch of the left coronary artery in the coronary groove, then passes through its terminal, often paired branch - the paraconal interventricular vein, v. interventricularis paraconalis - in the groove of the same name and in the region of the apex of the heart, anastomoses with the terminal branches of the middle cardiac vein, v. cordis media. The branches of the great cardiac vein are: marginal vein of the left ventricle, v. maryinis ventriculi sinistri, proximal vein of the left ventricle, v. proximalis ventriculi sinistri, and the cat also has the angular vein, v. angularis.
From the paraconal interventricular vein depart: vein of the conus arteriosus, v. coni arteriosi, distal collateral vein, v. collateralis distalis, and vein of the interventricular septum, v. septi interventricularis.
Small veins of the heart, vv. cordis parvae, collect blood from areas of the wall of the right ventricle adjacent to the coronary sulcus and carry it directly to the right atrium. According to their topography, clogged veins can be divided into the vein of the conus arteriosus, V. coni arteriosi, the proximal vein of the right ventricle, v. proximalis ventriculi dextri, marginal vein of the right ventricle, v. marginis ventriculi dextri, and distal vein of the right ventricle, v. distalis ventriculi dextri. In the cat, the last three vessels unite into a common trunk, which can be designated as the right semicircular vein, v. semkircumflexa dextra.
Part of the venous blood from the endocardial area flows directly into the heart cavity through the smallest cardiac veins (thebesian veins), vv. cordis minimae (Thebesii). Their number is greatest in the right atrium, less in the left atrium, even less in the right ventricle and least in the left ventricle. Thebesian veins are very narrow tubules several millimeters long, extending from the muscle capillaries and flowing into the cavities of the heart through the openings of the smallest veins, foramina venarum minimarum. The smallest veins do not have valves.
Rice. 17. Arteries and veins of the interventricular septum of the cat’s heart. The wall of the right ventricle is cut off (magnification 1.5 times) (according to Habermehl, 1959)
A atrium dextrum; In auriculus dexter; With mm. papillares parvi; D, D' septum interventriculare. E m. papillaris subarteriosus; Apex cordis
a arcus aortae; b v. cava caudalis; with v. cava cranialis; d truncus pulmonalis
1 ramus circumflexus, a. coronaria dextra; 2 ramus interventricularis subsinuosus, a. coronaria dextra, 3 ramus interventricularis paraconalis, a. coronaria sinistra; 4 ramus septi interventricularis; 5, 6, 7 ramus interventricularis subsinuosus or paraconalis
Literature used: Anatomy of a dog and a cat (Coll, authors) / Transl. with him. E. Boldyreva, I. Kravets. - M.: “AQUARIUM BUK”, 2003. 580 pp., ill. color on
Download abstract: You do not have access to download files from our server. HOW TO DOWNLOAD HERE
Heart valves
The right atrium from the left, as well as the right ventricle from the left, are separated by septa. Normally, in an adult, the partitions should be solid, there should be no holes between them.
But there must be a hole between the ventricle and the atrium on each side. If we are talking about the left half of the heart, then this is the left atrioventricular opening (ostium atrioventriculare sinistrum). On the right, the ventricle and atrium are separated by the right atrioventricular orifice (ostium atrioventriculare dextrum).
Valves are located at the edges of the holes. These are clever devices that prevent the blood from flowing back. When the atrium needs to send blood to the ventricle, the valve is open. After the ejection of blood from the atrium into the ventricle has occurred, the valve must close tightly to prevent blood from flowing back into the atrium.
The valve is formed by leaflets, which are double layers of endothelium - the inner lining of the heart. Tendon threads extend from the valves, which are attached to the papillary muscles. It is these muscles that control the opening and closing of the valves.
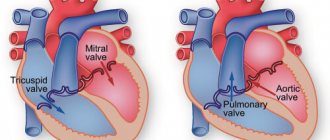
Tricuspid valve (valva tricispidalis)
This valve is located between the right ventricle and the right atrium. It is formed by three plates to which tendon threads are attached. The tendon threads themselves connect to the papillary muscles located in the right ventricle.
On a section in the frontal plane, we cannot see three plasties, but we can clearly see the papillary muscles (outlined in black) and tendon threads attached to the valve plates. The cavities that the valve separates are also clearly visible - the right atrium and the right ventricle.
On a section in a horizontal plane, the three leaflets of the tricuspid valve appear before us in all their glory:
Mitral valve (valva atrioventricularis sinistra)
The mitral valve regulates blood flow between the left atrium and the left ventricle. The valve consists of two plates, which, as in the previous case, are controlled by the papillary muscles through tendon threads. Please note - the mitral valve is the only heart valve that consists of two leaflets.
The mitral valve is outlined in green, and the papillary muscles are outlined in black:
Let's look at the mitral valve in the horizontal plane. Let me note again that only this valve consists of two plates:
Pulmonary valve (valva trunci pulmonalis)
The pulmonary valve is also often called the pulmonary valve or pulmonary valve. These are synonyms. The valve is formed by three flaps that are attached to the pulmonary trunk at its origin from the right ventricle.
You can easily find the pulmonary valve if you know that the pulmonary trunk starts from the right ventricle:
On a horizontal section, you can also easily detect the pulmonary valve if you know that it is always located anterior to the aortic valve. The pulmonary valve generally occupies the most anterior position of all the heart valves. We can easily find the pulmonary valve itself and the three valves that form it:
Aortic valve (valva aortae)
We have already said that the powerful left ventricle sends a portion of fresh, oxygenated blood to the aorta and further in a large circle. The aortic valve separates the left ventricle and the aorta. It is formed by three plates that are attached to the annulus fibrosus. This ring is located at the junction of the aorta and the left ventricle.
When examining the heart in a slice in a horizontal plane, do not forget that the pulmonary valve is in front, and the aortic valve is behind it. The aortic valve is surrounded by all the other valves from this angle:
Internal anatomy and structural features of valves, atria, ventricles
Each part of the heart has its own function and anatomical features. In general, the LV is more powerful (compared to the right), as it forces blood into the arteries, overcoming the high resistance of the vascular walls. The PP is more developed than the left, it receives blood from the whole body, and the left one only from the lungs.
Which side of a person's heart is on?
In humans, the heart is located on the left side in the center of the chest. The main part is located in this area - 75% of the total volume. One third extends beyond the midline into the right half. In this case, the axis of the heart is inclined (oblique direction). This situation is considered classic, as it occurs in the vast majority of adults. But options are also possible:
- dextrocardia (right side);
- almost horizontal - with a wide, short chest;
- close to vertical - for thin people.
Where is a person's heart located?
The human heart is located in the chest between the lungs. It is adjacent to the sternum from the inside, and is limited below by the diaphragm. It is surrounded by the pericardium, the pericardium. Pain in the heart area appears on the left near the mammary gland. The top is projected there. But with angina, patients feel pain behind the sternum, and it spreads along the left side of the chest.
Where is the heart located in the human body?
The heart in the human body is located in the center of the chest, but its main part goes into the left half, and only one third is located on the right side. For most people it has an angle of inclination, but for overweight people its position is closer to horizontal, and for thin people it is closer to vertical.
Location of the heart in the human chest
In humans, the heart is located in the chest in such a way that its anterior and lateral surfaces are in contact with the lungs, and its posterior and inferior surfaces are in contact with the diaphragm. The base of the heart (from above) passes into large vessels - the aorta, pulmonary artery. The apex is the lowest part, it approximately corresponds to the 4-5 space between the ribs. It can be found in this area by lowering an imaginary perpendicular from the center of the left collarbone.
External structure of the heart
The external structure of the heart refers to its chambers; it contains two atria and two ventricles. They are separated by partitions. The pulmonary veins, the vena cava, enter the heart, and the arteries of the lungs, the aorta, carry the blood out. Between the large vessels, at the border of the atria and ventricles of the same name, there are valves:
- aortic;
- pulmonary artery;
- mitral (left);
- tricuspid (between the right parts).
The heart is surrounded by a cavity containing a small amount of fluid. It is formed by the pericardial layers.
What does a human heart look like?
If you clench your fist, you can imagine exactly the appearance of a heart. In this case, the part that is located at the wrist joint will be its base, and the acute angle between the first and thumb will be its apex. What is important is that its size is also very close to a clenched fist.
- Structure and functions of the human heart
This is what a human heart looks like
Borders of the heart and their projection onto the surface of the chest
The boundaries of the heart are found by percussion, by tapping; radiography or echocardiography helps to determine them more accurately. The projections of the cardiac contour onto the surface of the chest are:
- right – 10 mm to the right of the sternum;
- left – 2 cm inward from the perpendicular from the center of the collarbone;
- apex – 5th intercostal space;
- base (upper) – 3rd rib.
What tissues make up the heart?
The heart consists of the following types of tissue:
- muscle - the main one, is called the myocardium, and the cells are cardiomyocytes;
- connective – valves, chords (threads that hold the valves), outer (epicardial) layer;
- epithelium – inner lining (endocardium).
Surfaces of the human heart
The human heart has the following surfaces:
- ribs, sternum – anterior;
- pulmonary – lateral;
- diaphragmatic – lower.
Apex and base of the heart
The apex of the heart is directed down and to the left, its localization is the 5th intercostal space. It represents the top of the cone. The wide part (base) is located on top, closer to the collarbones, and is projected at the level of the 3rd rib.
Human heart shape
The shape of a healthy person's heart is like a cone. Its tip is directed at an acute angle down and to the left of the center of the sternum. The base contains the mouths of large vessels and is located at the level of the 3rd rib.
Right atrium
Receives blood from the vena cava. Next to them is the foramen ovale, which connects the RA and LA in the fetal heart. In a newborn, it closes after the pulmonary blood flow opens, and then completely heals. During systole (contraction), venous blood passes into the pancreas through the tricuspid valve. The RA has a fairly powerful myocardium and a cubic shape.
Left atrium
Arterial blood from the lungs passes into the LA through 4 pulmonary veins and then flows through the opening into the LV. The walls of the LA are 2 times thinner than those of the right one. The shape of the LP is similar to a cylinder.
Right ventricle
It looks like an inverted pyramid. The capacity of the pancreas is about 210 ml. It can be divided into two parts - the arterial (pulmonary) cone and the ventricular cavity itself. In the upper part there are two valves: the tricuspid and the pulmonary trunk.
Left ventricle
It looks like an inverted cone, its lower part forms the top of the heart. The thickness of the myocardium is the largest - 12 mm. There are two openings at the top - for connection with the aorta and LA. Both of them are covered by valves - the aortic and mitral.
- Causes, symptoms and treatment methods for congenital heart disease - bicuspid aortic valve
Why are the walls of the atria thinner than the walls of the ventricles?
The thickness of the walls of the atrium is less, they are thinner, since they only need to push blood into the ventricles. The right ventricle follows them in strength; it throws its contents into the neighboring lungs, and the left one is the largest in terms of the size of its walls. It pumps blood to the aorta, where there is high pressure.
Tricuspid valve
The right atrioventricular valve consists of a sealed ring that limits the opening and leaflets; there may be not 3, but from 2 to 6.
Half of the people have a tricuspid configuration.
The function of this valve is to prevent the reflux of blood into the RA during RV systole.
Pulmonary valve
It prevents blood from passing back into the pancreas after it contracts. The composition contains valves similar in shape to a crescent. In the middle of each there is a knot that seals the closure.
Mitral valve
It has two doors, one is in the front and the other is in the back. When the valve is open, blood flows from the LA to the LV. When the ventricle contracts, its parts close together to allow blood to pass into the aorta.
Aortic valve
Formed by three semilunar-shaped flaps. Like the pulmonary one, it does not contain threads that hold the valves in place. In the area where the valve is located, the aorta expands and has depressions called sinuses.
Adult heart weight
Depending on the physique and total body weight, the weight of the heart in an adult varies from 200 to 330 g. In men, it is on average 30-50 g heavier than in women.
Layers of the Heart
1. Pericardium . This is a dense connective tissue membrane that reliably covers the heart.
The pericardium is a two-layer membrane; it consists of fibrous (outer) and serous (inner) layers. The serous layer is also split into two plates - parietal and visceral. The visceral plate has a special name - epicardium .
In many authoritative sources you can see that the epicardium is the first lining of the heart.
2. Myocardium (myocardium). The actual muscle tissue of the heart. This is the most powerful layer of the heart. The most developed and thick myocardium forms the wall of the left ventricle, as we already discussed at the beginning of the article.
See how the thickness of the myocardium differs in the atria (using the example of the left atrium) and in the ventricles (using the example of the left ventricle).
3. Endocardium (endocardium). This is a thin plate that lines the entire internal space of the heart. The endocardium is formed by endothelium - a special tissue consisting of epithelial cells tightly adjacent to each other. The development of atherosclerosis, hypertension, myocardial infarction and other serious cardiovascular diseases is associated with endothelial pathology.
Topography of the heart
Remember in the last lesson on basic chest topography I said that without knowing topographic lines you will not be able to learn anything related to the chest cavity? Have you learned them? Great, arm yourself with your knowledge, now we will use it.
So, the boundaries of absolute cardiac dullness and relative cardiac dullness are distinguished.
This strange name comes from the fact that if you tap (in medicine this is called “percussion”) the chest, in the place where the heart is located, you will hear a dull sound. When percussed, the lungs are more sonorous than the heart, which is where this term comes from.
Relative dullness is the anatomical ( true ) boundaries of the heart. We can establish the limits of relative dullness during the autopsy. Normally, the heart is covered by the lungs, so the boundaries of relative cardiac dullness are visible only on the preparation.
Absolute cardiac dullness is the boundaries of the part of the heart that is not covered by the lungs. As you understand, the limits of absolute cardiac dullness will be less than the limits of relative cardiac dullness in the same patient.
Since we are now examining anatomy, I decided to talk only about the relative, that is, the true boundaries of the heart. After the article about the anatomy of the hematopoietic system, I generally try to keep track of the size of the articles.
Boundaries of relative cardiac dullness (true boundaries of the heart)
- Apex of the heart (1): 5th intercostal space, 1-1.5 centimeters medial to the left midclavicular line (highlighted in green);
- Left border of the heart (2): a line drawn from the intersection of the third rib with the parasternal line (yellow) to the apex of the heart. The left border of the heart is formed by the left ventricle. In general, I advise you to remember the third rib - you will constantly encounter it as a landmark for various anatomical formations;
- The upper bound (3) is the simplest. It runs along the upper edge of the third ribs (we see the third rib again) from the left to the right parasternal lines (both yellow);
- Right border of the heart (4): from the upper edge of the 3rd (again) to the upper edge of the 5th rib along the right parasternal line. This border of the heart is formed by the right ventricle;
- Inferior border of the heart (5): a horizontal line drawn from the cartilage of the fifth rib along the right parasternal line to the apex of the heart. As you can see, the number 5 is also very magical in terms of determining the boundaries of the heart.
Conduction system of the heart. Pacemakers.
The heart has amazing properties. This organ is capable of independently generating an electrical impulse and conducting it through the entire myocardium. Moreover, the heart can independently organize the correct rhythm of contraction, which is ideal for delivering blood throughout the body.
Once again, all skeletal muscles and all muscular organs are capable of contracting only after receiving an impulse from the central nervous system. The heart is capable of generating an impulse on its own .
The conduction system of the heart is responsible for this - a special type of cardiac tissue that can perform the functions of nervous tissue. The conduction system of the heart is represented by atypical cardiomyocytes (literally translated - “atypical cardiomuscular cells”), which are grouped into separate formations - nodes, bundles and fibers. Let's look at them.
1. Sinatrial node (nodus sinatrialis) . The author's name is the Kissa-Fleck knot. It is also often called the sinus node. The sinatrial node is located between the junction of the superior vena cava into the right ventricle (this place is called the sinus) and the appendage of the right atrium. "Sin" means "sine"; “atrium,” as you know, means “atrium.” We get - “sinatrial node”.
By the way, many who begin to study ECG often wonder what is sinus rhythm and why is it so important to be able to confirm its presence or absence? The answer is quite simple.
The sinus node is the first order pacemaker. This means that normally it is this node that generates excitation and transmits it further along the conduction system. As you know, in a healthy person at rest, the synatrial node generates from 60 to 90 impulses, which coincides with the pulse rate. Such ri, since it is generated exclusively by the synatrial node.
You can find it on any anatomical tablet - this node is located above all other elements of the conduction system of the heart.
2. Atrioventricular node (nodus atrioventricularis) . The author's name is the Ashshof-Tavara knot. It is located in the interprestrial septum just above the tricuspid valve. If you translate the name of this node from Latin, you will get the term “atrioventricular node,” which exactly corresponds to its location.
The atrioventricular node is a second- order pacemaker. If the atrioventricular node has to start the heart, then the sinatrial node is turned off. This is always a sign of serious pathology. The atrioventricular node is capable of generating excitation with a frequency of 40-50 impulses. Normally, it should not generate excitement; in a healthy person, it only works as a conductor.
The antrioventricular node is the second node from above after the sinatrial node. Identify the sinatrial node - it is the highest - and immediately below it you will see the atrioventricular node.
How are the sinus and atrioventricular nodes connected? There are studies that suggest the presence of three bundles of atypical cardiac tissue between these nodes. Officially, these three bundles are not recognized in all sources, so I did not separate them into a separate element. However, in the picture below I have drawn three green tufts - front, middle and back. This is approximately how these internodal bundles are described by the authors who acknowledge their existence.
3. Bundle of His, often called the atrioventricular bundle (fasciculus atrioventricularis) .
After the impulse has passed through the atrioventricular node, it diverges into two sides, that is, into two ventricles. The fibers of the conduction system of the heart, which are located between the atrioventricular node and the point of division into two parts, are called the bundle of His.
If, due to some serious illness, both the synatrial and atrioventricular nodes are switched off, then the His bundle has to generate excitation. third pacemaker . It is capable of generating 30 to 40 pulses per minute.
For some reason I depicted the His bundle in the previous step. But in this one I’ll highlight it and sign it so that you remember it better:
4. Legs of the bundle of His, right and left (crus dextrum et crus sinistrum) . As I already said, the bundle of His is divided into right and left branches, each of which goes to the corresponding ventricles. The ventricles are very powerful chambers, so they require separate branches of innervation.
5. Purkinje fibers . These are small fibers into which the bundle branches crumble. They entwine the entire ventricular myocardium in a fine network, ensuring complete conduction of excitation. If all other pacemakers are turned off, then Purkinje fibers will try to save the heart and the entire body - they are capable of generating a critically dangerous 20 impulses per minute. A patient with such a pulse requires emergency medical attention.
Let's consolidate our knowledge of the conduction system of the heart with another illustration:
Blood supply to the heart
From the very initial part of the aorta - the bulb - two large arteries depart, which lie in the coronary sulcus (see above). On the right is the right coronary artery, and on the left is the left coronary artery.
Here we look at the heart from the anterior (that is, from the sternocostal) surface. In green, I highlighted the right coronary artery from the aortic bulb to the area where it begins to give off branches.
The right coronary artery encircles the heart to the right and backward. On the posterior surface of the heart, the right coronary artery gives off a large branch called the posterior interventricular artery . This artery is located in the posterior interventricular groove. Let's look at the posterior (diaphragmatic) surface of the heart - here we see the posterior interventricular artery, highlighted in green.
The left coronary artery has a very short trunk. Almost immediately after leaving the aortic bulb, it gives off a large anterior interventricular branch , which lies in the anterior interventricular groove. After this, the left coronary artery gives off another branch - the circumflex . The circumflex branch goes around the heart to the left and back.
And now our favorite green color highlights the contour of the left coronary artery from the aortic bulb to the area where it splits into two branches:
One of these branches lies in the interventricular groove. Accordingly, we are talking about the anterior interventricular branch :
On the posterior surface of the heart, the left circumflex coronary artery forms an anastomosis ( direct connection ) with the right coronary artery. I highlighted the anastomosis site in green.
Another large anastomosis is formed at the apex of the heart. It is formed by the anterior and posterior interventricular arteries. To show it, you need to look at the heart from below - I could not find such an illustration.
In fact, among the arteries that supply blood to the heart, there are many anastomoses. The two large ones, which we talked about earlier, form two “rings” of cardiac blood flow.
But from the coronary arteries and their interventricular branches there are many small branches that intertwine with each other in a huge number of anastomoses.
The number of anastomoses and the volume of blood that passes through them are factors of great clinical importance . Imagine that a blood clot got into one of the large arteries of the heart and blocked the lumen of this artery. In a person with an abundant network of anastomoses, blood will immediately flow through bypass pathways and the myocardium will receive blood and oxygen through collaterals. If there are few anastomoses, then a large area of the heart will remain without blood supply, and myocardial infarction .
Forms of blood supply
- Aorta (anatomy) - structure and sections, functions, pathologies
Heart with a right coronary type of blood supply: the right coronary artery (1) and its branches are more developed than the left coronary artery (2)
There are several types of blood supply to the heart. All of them are a variant of the norm and a consequence of the individual characteristics of the formation of heart vessels and their functioning in each person. Depending on the prevailing distribution of one of the coronary arteries on the posterior heart wall, they are distinguished:
- Legal type. With this type of blood supply to the heart, the left ventricle (posterior surface of the heart) is filled with blood primarily from the right coronary artery. This type of blood supply to the heart is the most common (70%)
- Left-handed type. Occurs if the left coronary artery predominates in the blood supply (in 10% of cases).
- Uniform type. With approximately equal “contribution” to the blood supply of both vessels. (20%).
Venous drainage from the heart
The venous system of the heart begins with tiny venules that collect into larger veins. These veins in turn empty into the coronary sinus , which opens into the right atrium. As you remember, all venous blood of the entire body collects in the right atrium, and blood from the heart muscle is no exception.
Let's look at the heart from the diaphragmatic surface. The opening of the coronary sinus is clearly visible here - it is highlighted in green and is indicated by the number 5.
The great vein of the heart lies in the anterior interventricular groove . It begins on the anterior surface of the apex of the heart, then lies in the anterior interventricular groove, then in the coronary groove. In the coronary sulcus, the large vein bends around the heart backward and to the left, flowing on the posterior surface of the heart into the right atrium through the coronary sinus.
Please note - unlike the arteries, the great vein of the heart is located both in the anterior interventricular sulcus and in the coronary sulcus. This is still a large vein of the heart:
The middle cardiac vein passes from the apex of the heart along the posterior interventricular groove and flows into the right end of the coronary sinus.
The small vein of the heart (vena cordis parva) lies in the right coronary sulcus. In the direction to the right and back, it goes around the heart, flowing into the right atrium through the coronary sinus. In this picture, I highlighted the middle vein in green, and the small vein in yellow.
Location anomalies
In typical clinical cases, which are the vast majority, the heart is on the left side. But there are at least two known conditions when this is not the case.
Dextrocardia
It is extremely rare. It is a congenital anomaly. The essence of the deviation (it is not considered a disease in the full sense of the word) is the reverse, mirror arrangement of the heart.
Normally it is on the left, in patients with a similar disorder it is on the right. Further options are possible regarding the localization of other organs.
With isolated dextrocardia, unpaired organs remain in their proper places. Only the heart moves. With systemic, complex transposition is observed. All organs mirror move in the opposite direction.
As a rule, such a deviation does not cause discomfort to the patient. This is normal and physiological in 85-90% of cases. Unfortunately, in the remaining 10-15% of situations, pronounced problems are found.
Usually these are congenital defects of cardiac structures that require surgical care.
In the absence of this, a typical clinical picture of physical and mental retardation in development is revealed.
Possible symptoms include:
- Insufficiently rapid weight gain in early periods of life.
- Drowsiness. The child is not active enough and has little interest in the world around him. Almost does not cry and is not capricious even in the presence of an irritating factor.
- Paleness of the skin.
- Cyanosis (blue discoloration) of the nasolabial triangle, nails, limbs, mucous membranes (the change is especially clearly visible in the gums).
As you grow older, signs of physical, mental retardation, or both phenomena are revealed.
- Slow thinking. Infantility, insufficient growth rate.
- Problems with assimilation of information and its reproduction. Therefore, difficulties are always discovered at school.
- Low body weight. Painful thinness.
- Pale skin.
- Dyspnea. Exercise intolerance or a significant decrease in exercise tolerance.
- Tachycardia, bradycardia. Different types of arrhythmias.
- In adulthood, insufficiently corrected disorders can lead to decreased potency, libido, and infertility.
Fortunately, irreversible changes occur relatively rarely. It is possible to eliminate organic defects and functional disorders, usually by surgical methods.
Then a course of drug treatment is prescribed using cardioprotectors, antihypertensive and antiarrhythmic drugs in short doses if necessary.
It is not difficult to identify dextrocardia. The position of the heart is left-sided. Even with listening, auscultation, not to mention echocardiography, the fact of transposition becomes obvious.
Next, you need to determine whether there are pathological changes in tissues, cardiac structures, or functional disorders.
In the vast majority of cases, there are no problems with well-being. A person grows and develops within normal limits and does not feel discomfort.
Deviation in such a situation is considered more of a feature than a congenital defect.
Dextroposition
Unlike the previous condition, this almost never occurs in healthy people. The point here is not the transposition of organs.
We are talking about a displacement of cardiac structures relative to the normal anatomical position. Such an anomaly also cannot be congenital, except in extremely rare cases.
The process involves the heart and the organ that caused the displacement.
The causes are mostly pulmonary. Associated with abnormal tissue growth, changes in their volume, deformation of the diaphragm, tumors, and muscle pathologies.
The symptoms are always present and they are quite clear:
- Chest pain of unknown origin. With significant transposition, they are found to the right, which is due to a change in position. Reflected sensations are possible.
- Arrhythmia. By type of acceleration of cardiac activity, decrease in contraction frequency, or change in the interval between beats. All options are dangerous and can cause fatal complications.
- Dyspnea. Decreased exercise tolerance. The intensity of the symptom increases as the underlying disease and dextroposition itself progress.
- Paleness of the skin. Also gums, nail plates.
- Cyanosis of the nasolabial triangle. Blue discoloration of the area around the mouth.
- Collaptoid states. They are relatively rare. Preceded by emergency disorders such as stroke or heart attack.
- Instability of blood pressure levels. Rise or fall. Also the change is irregular over several hours and so on for a long time.
The disorder can be diagnosed based on the results of echocardiography using ultrasound techniques. Also, in the most complex and controversial situations, an MRI is prescribed.
If a tumor process is suspected (neoplasia can be hidden, they are not always visible), with contrast enhancement with gadolinium preparations.
The heart is positioned incorrectly, displaced relative to other structures, and deformation of the organ is possible due to compression.
Treatment is surgical in most cases. Its essence is to restore the anatomical integrity of tissues and normalize the position of the heart.
Conservative (medicinal) technique is used as an auxiliary one. Without medications, it will not be possible to correct functional disorders.
Dextroposition poses a great danger to health and life. The problem is not only in the deviation itself, but also in the reason for it.
Attention:
The following condition also refers to anomalies and behaves in most cases unpredictably, therefore requiring careful monitoring by doctors.
Dextroversion
The essence of the disorder is the inverted arrangement of cardiac structures in the normal position of other organs.
The apex of the heart is located in the opposite direction, the organ is rotated on its own axis in the opposite direction, 180 degrees.
Formally, this is also not a disease. And the so-called minor anomaly. Detected by the results of echocardiography or ECG.
It gives practically no symptoms, as well as any disturbances in well-being. There is usually no danger either.
Heart fixation device
The heart is a critical organ. The heart should not move freely in the chest cavity, so it has its own fixation apparatus. Here's what it consists of:
- The large vessels of the heart are the aorta, pulmonary trunk and superior vena cava. In thin people with an asthenic body type, the heart is located almost vertically. It is literally suspended on these large vessels, in which case they are directly involved in fixing the heart;
- Uniform pressure from the lungs;
- The upper pericardial ligament (ligamentun sternopericardiaca superior) and the lower pericardial ligament (ligamentun sternopericardiaca inferior). These ligaments attach the pericardium to the posterior surface of the manubrium of the sternum (superior ligament) and the body of the sternum (inferior ligament);
- A powerful ligament that connects the pericardium to the diaphragm. I did not find a Latin name for this ligament, but I did find a drawing from my favorite atlas of topographic anatomy. Of course, this is the atlas of Yu.L. Zolotko. I have outlined the link in this illustration with a green dotted line: