The heart is a muscular pump that ensures continuous movement of blood through the vessels. Together, the heart and blood vessels make up the cardiovascular system. This system consists of the systemic and pulmonary circulation. From the left side of the heart, blood first moves through the aorta, then through large and small arteries, arterioles, and capillaries. In the capillaries, oxygen and other substances necessary for the body enter the organs and tissues, and from there carbon dioxide, metabolic products, are removed. After this, the blood turns from arterial to venous and again begins to move towards the heart. First along the venules, then through smaller and larger veins. Through the inferior and superior vena cava, blood again enters the heart, only this time into the right atrium. A large circle of blood circulation is formed.
Venous blood from the right side of the heart is sent through the pulmonary arteries to the lungs, where it is enriched with oxygen, and returns to the heart again - this is the pulmonary circulation.
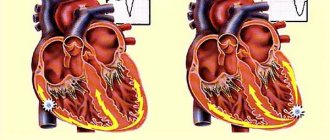
Inside, the heart is divided by partitions into four chambers. The two atria are divided by the interatrial septum into the left and right atria. The left and right ventricles of the heart are separated by the interventricular septum. Normally, the left and right parts of the heart are completely separate. The atria and ventricles have different functions. The atria store blood that flows into the heart. When the volume of this blood is sufficient, it is pushed into the ventricles. And the ventricles push blood into the arteries, through which it moves throughout the body. The ventricles have to do more hard work, so the muscle layer in the ventricles is much thicker than in the atria. The atria and ventricles on each side of the heart are connected by the atrioventricular orifice. Blood moves through the heart in only one direction. In the systemic circle of blood circulation from the left side of the heart (left atrium and left ventricle) to the right, and in the small circle from the right to the left.
The correct direction of blood flow is ensured by the valve apparatus of the heart:
Valves:
- tricuspid
- pulmonary
- mitral
- aortic
They open at the right time and close, preventing blood flow in the opposite direction.
Aortic valve
Closes the entrance to the aorta. It also consists of three valves, which look like crescents. Opens when the left ventricle contracts. In this case, blood enters the aorta. When the left ventricle relaxes, it closes. Thus, venous blood (poor in oxygen) from the superior and inferior vena cava enters the right atrium. When the right atrium contracts, it moves through the tricuspid valve into the right ventricle. Contracting, the right ventricle ejects blood through the pulmonary valve into the pulmonary arteries (pulmonary circulation). Enriched with oxygen in the lungs, the blood turns into arterial blood and moves through the pulmonary veins to the left atrium, then to the left ventricle. When the left ventricle contracts, arterial blood enters the aorta through the aortic valve under high pressure and spreads throughout the body (systemic circulation).
The heart muscle is called the myocardium
There are contractile and conductive myocardium. The contractile myocardium is the actual muscle that contracts and produces the work of the heart. In order for the heart to contract in a certain rhythm, it has a unique conduction system. The electrical impulse to contract the heart muscle occurs in the sinoatrial node, which is located in the upper part of the right atrium and spreads through the conduction system of the heart, reaching every muscle fiber
First, both atria contract, then both ventricles, thereby ensuring the flow of blood to all organs and tissues of the body. The heart muscle has two membranes (external and internal). The inner lining of the heart is called the endocardium. The outer lining of the heart is called the pericardium.
What is the essence of the problem
Bull heart syndrome is another name for cardiomegaly. According to the definition, the disease is characterized by an enlargement of all four or one chamber of the heart, as a result of which the main muscle is not able to perform a pumping function and maintain the central hemodynamics of the body. The heart becomes flabby and exhausted due to illness, and muscle fibers do not stretch because there is not enough strength to function normally.
An increase in heart size is a natural process in some people, particularly in athletes or those who frequently engage in physical labor.
In some cases, the disease occurs without obvious clinical manifestations. This most often occurs in the initial stages of the disease.
In the classic version, the disease clinically manifests itself in the form of rhythm disturbances (arrhythmia), or frequent shortness of breath, swelling and pain in the heart area. These signs can also appear in other diseases of the heart muscle. Therefore, you should not delay visiting a specialist in the field of cardiology, because symptoms of an enlarged heart can usually be identified only with the help of a certain medical examination.
Sincere confession. How to preserve your heart during an epidemic? More details
Conduction system of the heart
The heart, like any organ, has its own nervous system. The nervous system of the heart has several levels. The first and main pacemaker of the heart is the sinus node, located in the right atrium. It is subject to the atrioventricular node, which is located on the border between the atria and ventricles and quite often slows down the heart rate set by the sinus node. Then the nerve impulse goes to the ventricles of the heart along the branches of the Hiss bundle, which are divided into the smallest nerve endings - Purkinje fibers.
Heart disease: causes and prevention
Heart disease has killed more people throughout human history than all wars combined.
Today they continue to subtract at least ten years from the average life expectancy of the world's population. Moreover, heart disease is becoming younger and often affects working people. All this generally negatively affects the quality of life. If you suspect a problem with the cardiovascular system, do not delay visiting a medical facility. With the help of examinations, the doctor will be able to prescribe a suitable course of treatment.
Photo: Human anatomy. In 2 volumes. T.2 / Author: E.I. Borzyak, V.Ya. Bocharov, L.I. Volkova and others / Ed. M. R. Sapina. - M.: Medicine, 1986. - 480 pp.: UGC
Bad habits, poor nutrition, lack of physical activity - these are the main reasons why the cardiovascular system suffers and certain disorders appear.
In addition, in my work I often come across the fact that people deliberately ignore the symptoms of heart disease, considering themselves too young and healthy to develop them. A diseased heart makes itself felt by painful sensations in various locations (back, chest, left arm, neck), weakness, nausea, cough, difficulty breathing, increased sweating, swelling of the legs, snoring. Signs of heart disease are clearly described in material from the reliable resource webmd.com.
In any case, the practical experience of cardiologists suggests that it is necessary to check the heart at least once every six months. This helps prevent many serious heart diseases. The list of the most relevant ones looks like this:
- cardiac ischemia;
- stroke;
- heart attack;
- hypertension.
Heart disease in women and men should be prevented, first of all, by lifestyle correction. It is bad habits, overeating, and low mobility that gradually destroy the heart muscle, which can work for up to 150 years.
It should be remembered that the functioning of the cardiovascular system is disrupted imperceptibly, gradually, but restoring it is not an easy task. It is much easier to make a healthy lifestyle the norm and not have problems with the heart and blood vessels.
"The heart is on the left"
– The top of the organ and 2/3 of its parts are on the left, but 1/3 is behind the sternum in the middle.
Often people claim that they are stabbed in the heart and grab their left side. It is important to understand here: classic heart pain is pain, as a rule, precisely behind the sternum. Pain on the left side can also be cardiac. But they are burning, pressing. Therefore, if you have a stabbing sensation on the left side, the cause may not be cardiological at all. Answer: myth
“During physical and emotional stress, the heart pumps more blood than at rest”
– At rest, the heart pumps about 4.5–5 liters of blood per minute.
But with physical stress, the figure can increase two to three times, sometimes reaching one hundred liters. Let's say an athlete is running a cross-country race. In order for a person to cope with a difficult task, his heart needs to provide the muscles with energy, fill the body with glucose and oxygen. With emotional stress, the situation is even more serious, because our emotions are adrenaline, that is, acceleration. Acute stress, such as the loss of a loved one, increases the risk of heart disease by 21 times, and chronic stress increases the risk by 50 times. Answer: true
Preventive actions
To prevent various pathological conditions in the myocardium, the following rules must be followed:
- stop smoking and drinking alcoholic beverages;
- alternate work with periods of rest;
- Healthy food;
- engage in physical exercise.
To live happily ever after, you should take care of your heart. It is necessary to undergo an annual examination by a cardiologist and do an ECG.
“Body weight has no effect on heart function”
- How it influences!
After all, this organ circulates blood throughout the body. And the more a person weighs, the more his heart muscle is exhausted. Although thin people can have problems, dystrophy is one of them. Body weight should be normal. There is a special formula that can be used to estimate the degree of correspondence between a person’s mass and his height. To do this, you need to divide your weight by your height squared. If the resulting figure ranges from 19 to 25, this is a good indicator. Answer: myth
Ventricular fibrillation (VF)
VF is a very fast, irregular heart rhythm that occurs in the right or left ventricle of the heart. VF is a more serious pathology than VT because the electrical system of the heart and the heartbeat cycle are completely disorganized. The ventricles tremble and the body receives only a small amount of pumped blood or none at all.
When the heart does not pump blood, the body quickly begins to experience oxygen starvation and sudden cardiac arrest occurs.
Symptoms develop immediately: first the pulse disappears, then consciousness, then the ability to breathe. If sudden cardiac arrest occurs, cardiopulmonary resuscitation (CPR) is required to keep the blood circulating until an external defibrillator can be used to restore the heart rhythm. Defibrillation can be performed by a doctor or emergency medical personnel using an external defibrillator by discharging an electric current through plates located on the chest. If the patient has an ICD implanted, defibrillation will occur automatically after a few seconds of VF onset.
Atrial fibrillation (AF)
Atrial fibrillation is the most common arrhythmia, usually a manifestation of other heart diseases (coronary heart disease, valvular disease, myocarditis, etc.) or metabolic disorders (thyrotoxicosis, electrolyte imbalance, etc.). Sometimes it occurs without an obvious cause, and then it is called idiopathic.
The mechanisms of development of atrial fibrillation are still not fully understood. In some patients, it occurs due to the presence of many chaotic circular waves of electrical excitation in the atria.
Atrial fibrillation is usually treated with medications that maintain a normal rhythm or prevent the heart rate from getting too fast. A prerequisite for atrial fibrillation is the use of anticoagulant therapy. It is used to thin the blood to prevent the formation of blood clots.
For the surgical treatment of atrial fibrillation, the method of radiofrequency ablation (RFA) is used, which is used to slow down the heart rate (RFA of the AV junction) or RFA “isolation of the pulmonary veins” is performed to restore sinus rhythm.
Tachycardia
If your heart rate exceeds 100 beats per minute, it is called tachycardia. Tachycardia can be sinus and belong to normal, physiological tachycardia. Tachycardias with a high frequency, which exceed 180 beats per minute, arising in connection with frequent, group extrasystole, additional conduction pathways are classified as a group of non-normal fast heart rhythms.
Physical activity, emotional stress, and certain diseases can cause an accelerated heart rate that exceeds 100 beats per minute.
When your heart rhythm is very fast or your heart beats for no reason at a high frequency and irregularly, it is called tachyarrhythmia.
Pathological tachycardia is harmful for several reasons. Firstly, with a rapid heartbeat, the efficiency of the heart decreases, since the ventricles do not have time to fill with blood, as a result of which blood pressure drops and blood flow to the organs decreases. Secondly, the conditions of the blood supply to the heart itself worsen, since it does more work per unit of time and requires more oxygen, and poor conditions of the blood supply to the heart increase the risk of coronary disease and subsequent heart attack.
Tachycardia is not a disease, but a symptom, since it can occur as a manifestation of many different diseases. The most common causes of tachycardia are disorders of the autonomic nervous system, endocrine system disorders, hemodynamic disorders and various forms of arrhythmia.
content .. 140 141 142 143 144 145 146 147 148 149 ..Heart (Mikhailov S.S.) (human anatomy)
Heart development (human anatomy)
The heart anlage appears in an embryo 1.5 mm long at the end of the 2nd week of intrauterine development in the form of two endocardial sacs arising from the mesenchyme. From the visceral mesoderm, myo-epicardial plates are formed, which surround the endocardial sacs. This is how two heart rudiments arise - cardiac vesicles, lying in the cervical region above the yolk sac. Subsequently, both cardiac vesicles close together, their inner walls disappear, resulting in the formation of one cardiac tube. From the layers of the heart tube formed by the myo-epicardial plate, the epicardium and myocardium are subsequently formed, and from the endocardial layer - the endocardium. In this case, the heart tube moves caudally and turns out to be located ventrally in the ventral mesentery of the foregut and covered with a serous membrane, which, together with the outer surface of the heart tube, forms the pericardial cavity.
The heart tube connects to developing blood vessels (see section Circulatory System, this edition). Two umbilical veins flow into its posterior section, carrying blood from the villous membrane, as well as two vitelline veins, bringing blood from the yolk bladder. Two primary aortas depart from the anterior part of the heart tube, which form 6 aortic arches (see section Circulatory system, this edition). Thus, the blood flows through the tube in one stream.
The development of the heart goes through four main stages - from single-chamber to four-chamber (Fig. 139).
Rice. 139. Embryonic development of the heart. a - three stages of development of the external shape of the heart; b - three stages of the formation of heart septa
Single chamber heart
. Due to the uneven growth of the heart tube, an S-shaped bend is formed, which is accompanied by a change in its shape and position. Initially, the lower end of the tube moves upward and posteriorly, and the upper end moves downward and anteriorly. In an embryo 2.15 mm long (3rd week of development), four sections can be distinguished in the S-shaped heart: 1) the venous sinus, into which the umbilical and vitelline veins flow; 2) the next venous section; 3) the arterial section, curved in the shape of a knee and located behind the venous; 4) arterial trunk.
Two-chambered heart
. The venous and arterial sections grow greatly and a deep constriction appears between them. Both sections are connected only through a narrow short canal, called the auricular canal, which lies at the site of the constriction. At the same time, from the venous section, which is the common atrium, two outgrowths are formed - future cardiac ears, which cover the arterial trunk. Both legs of the arterial section of the heart fuse with each other, the wall separating them disappears, resulting in the creation of one common ventricle. In addition to the umbilical and vitelline veins, two common veins flow into the venous sinus, formed by the fusion of the anterior and posterior cardinal veins. In the two-chamber heart of an embryo 4.3 mm long (4th week of development), there are: a venous sinus, a common atrium with two ears, a common ventricle communicating with the atrium by a narrow auricular canal, and an arterial trunk limited from the ventricle by a slight narrowing. At this stage of development there is only one large circle of blood circulation.
Three-chambered heart
. At the 4th week of development, a fold appears on the inner surface of the common atrium, growing downwards and forming a septum in the embryo 7 mm long (beginning of the 5th week) dividing the common atrium into two: right and left. However, a hole remains in the septum (foramen ovale), through which blood from the right atrium passes into the left. The auricular canal is divided into two atrioventricular openings.
Four chambered heart
. In an embryo 8-10 mm long (end of the 5th week), a septum growing from bottom to top is formed in the common ventricle, dividing the common ventricle into two: right and left. The common arterial trunk is also divided into two sections: the future aorta and the pulmonary trunk, which connect respectively to the left and right ventricles. At the same time, semilunar valves are formed in the truncus arteriosus and its two parts. Subsequently, the superior vena cava is formed from the right common cardinal vein. The left common cardinal vein undergoes reverse development and is transformed into the coronary venous sinus of the heart (see section Circulatory system, this edition).
content .. 140 141 142 143 144 145 146 147 148 149 ..
Diagnostics of cardiac dysfunctions
To diagnose various heart ailments, you should first undergo an electrocardiographic examination. During it, electronic phenomena are recorded, accompanied by muscle contraction.
The structure of the heart chambers includes a cardiomyocyte element, which helps generate the effective potential before contraction. This is determined by electrons, which must be applied to the chest area during the examination.
This helps to identify various failures in the functionality of the heart, organic and functional lesions.
Using electrocardiography, it is possible to determine whether a patient is developing a heart attack, defect, cavitary enlargement and other diseases.
By undergoing an auscultation examination, you can determine the disease. Experienced doctors, using this technique, determine a large number of pathological conditions in structure and pathology.
Using ultrasound, you can see the heart organ, consisting of chambers, see how blood is distributed in them, and determine muscle defects. Ultrasound determines the presence of various diseases, and a diagnosis is made based on the results.
With age, people experience an accumulation of various heart ailments, provoked by various pathologies. Often, disruptions in the cardiovascular system can occur even among those who monitor their health and follow a healthy lifestyle.
The most common pathologies are dilatation of the heart chambers, enlargement of the ventricles or atria, enlargement of the aorta, aneurysm and many others.
How to treat dilated changes
Dilatation is treated with medications and surgery. It is not possible to reduce the stretching of the heart chambers with the help of pills. Treatment helps eliminate inflammatory signs, normalize high or low blood pressure, rheumatoid, atherosclerotic or pulmonary diseases.
You should lead a healthy lifestyle and do everything that your doctor recommends. It is necessary to thin the blood with the help of medications, which will lead to passage through the heart chambers that have undergone any changes.
If all these measures do not help normalize the functioning of the heart, then it is necessary to carry out an operation during which a pacemaker device is implanted into the patient’s body cavity, which helps the heart wall contract effectively.
Diagnostic nuances
Bull heart syndrome is determined using complex diagnostics. It is the combination of several methods and techniques that allows for maximum assessment of the appearance, volume, and function of the heart. The list of studies to make such a diagnosis includes:
- blood analysis;
- chest x-ray;
- electrocardiogram;
- echocardiography;
- CT scan;
- sometimes - a biopsy of the inner surface of the heart ventricles.
All necessary studies are determined by the observing cardiologist. It is based on the severity of symptoms and the person’s condition.
A quieter pulse means you live longer. What should it be like normally? More details
Bradycardia. Slow heart rate
Your heart rate usually beats between 60 and 80 beats per minute.
A reading below 60 beats per minute is called bradycardia. For many people in good physical shape, or if such a rhythm occurs during rest and sleep, then such a rhythm is normal. A distinctive feature of such bradycardia is that with increasing physical activity, the heart rate begins to accelerate, covering the body’s needs with its frequency.
We talk about bradycardia as a disease when the rhythm has a very low frequency, does not respond by increasing frequency to physical activity, or large pauses occur in the rhythmic contraction, which can reach or even exceed more than 2 seconds. Such disturbances lead to fatigue, dizziness and loss of consciousness.
The most common cause of a slow heart rate is:
• Sinus node dysfunction (SU).
• Impaired conduction of the electrical signal from the atria to the ventricles through the atrioventricular node (AV).
When bradycardia is confirmed diagnostically and such a rhythm is the only manifestation, then such a rhythm is effectively corrected by a pacemaker. ICDs can also be used for bradycardia, but only if there are appropriate indications for ICD implantation (life-threatening cardiac arrhythmias).
Tachyarrhythmia
This is an abnormally fast heart rate (usually 100 to 400 beats per minute, which occurs either in the upper chambers of the heart (atrial fibrillation, supraventricular tachycardia) or in the lower chambers (ventricular fibrillation, ventricular tachycardia)).
Causes of tachyarrhythmia:
• Heart diseases such as high blood pressure, coronary artery disease (atherosclerosis), heart valve disease, heart failure, cardiomyopathy, tumors and infections.
• Other medical conditions, such as thyroid disease, some lung diseases, electrolyte imbalances, and alcohol and drug abuse.
• Caused by abnormal accessory pathways or extrasystoles.
Tachyarrhythmias occur when the impulse contracting the heart muscle arrives earlier than normal heart rhythm would suggest. Tachyarrhythmias can begin in the upper or lower chambers of the heart.
Tachyarrhythmia includes various types of cardiac arrhythmias:
• Supraventricular tachycardia.
• Ventricular tachycardia (VT).
• Ventricular fibrillation (VF).
Supraventricular tachyarrhythmias
Rhythm disorders involving the atria are called supraventricular (supraventricular) arrhythmias. This group of rhythm disturbances is the most common, and it is the one that doctors and patients have to deal with most often. There are 5 main types of supraventricular arrhythmias:
• atrioventricular nodal tachycardia;
• Wolff-Parkinson-White syndrome;
• intraatrial tachycardia;
• atrial flutter;
• atrial fibrillation.