If you study the anatomy and structure of the human heart, then read the article. It contains a lot of useful information.
The human heart is located asymmetrically in the chest, with a slight displacement to the left of the midline. This is a small muscular organ, the size of a clenched fist, surrounded on the outside by a membrane - the pericardium or pericardial sac. The heart pumps about seven tons of blood every day to supply nutrition to the human internal organs. It, throughout its entire life cycle, produces an average of 2.55 billion blows .
In another article on our website you can study human anatomy - the structure and location of internal organs . It has a lot of useful information to study.
The final formation of the muscular organ occurs in the tenth week during the period of intrauterine development of the fetus. After birth, it radically changes the principles of hemodynamics - the circulatory system: from nutrition by the mother’s placenta, a transition is made to pulmonary, independent nutrition. From this article you will learn where the human heart is located, what its structure is and much other interesting and useful information. Read on.
Where is a person’s heart located: photo
Location of the heart
The main part of the human heart, or rather two-thirds of its volume, is located on the left side of the center of the chest. And only one of the three parts extends slightly into the right half. This can be seen in the photo above. More details:
- The heart in the human body is located between the lungs.
- It is closely adjacent to the chest from the inside and is surrounded by the pericardial sac.
- In this case, the cardiac “axis” has a slight tilt.
- This arrangement is considered normal and occurs in most people.
But deviations from the standard location of this organ are possible:
- Right-handed location.
- Spread across the diaphragm or horizontal. The position is possible with a wide but short chest.
- Shift closer to vertical position. Occurs in thin people.
In addition, the position of the organ may depend on the somatic constitution of the person. In asthenic people it is vertical. The hypersthenic type is often horizontal, while the asthenic type is vertical.
Consequently, the coefficients of the location standard may undergo minor changes depending on the size of the heart, its individual characteristics, and the physiology of the human body and at the same time not be considered a pathology. And therefore it is possible to talk only about conditional standards, but not about the standard.
How is a cardiac MRI done?
MRI scan at heart level
The procedure is carried out by prior appointment. You will need to fill out forms at the clinic. You should bring with you an identification card, a doctor's prescription (if you have one) and other medical documentation that may be useful for analyzing the results (previous images, ultrasound, etc.).
The scanning procedure takes place in 3 stages:
- 1. Preparatory. In the locker room, you need to remove jewelry, accessories (hairpins, belt, glasses), clothes with metal fittings, and leave electronic devices and gadgets (they may break down). In the diagnostic room, you should lie down on the tomograph platform. For safety purposes, the patient's body is secured with soft straps. It is important to immediately take a comfortable position, since you cannot move during the scanning process. When planning contrast contrast, a catheter is installed in a vein and the device is connected to an injection syringe for automatic drug delivery.
- 2. Active stage. The radiologist goes into a nearby office, where he monitors the procedure and operates the equipment. You can communicate with a specialist at any time via a two-way communication system. After the command not to move, you need to relax, breathe freely, and remain calm. If necessary, the doctor will ask you to hold your breath for a few seconds. A heart scan in native mode lasts about 20 minutes.
- 3. Contrasting. They are not always performed, but only when indicated. On command, an amplifier is injected into the patient’s bloodstream using a syringe-injector, then a second scan is performed. How exactly it is necessary to do an MRI of the heart (with or without contrast) is usually indicated by a cardiologist. If a serious pathology is suspected, a radiologist may recommend enhancement.
Upon completion of the study, dress and take away personal belongings. You can wait for the results at the clinic or, if you go on personal business, return to the center later. Preparing a report takes from 15 minutes to several hours. In complex cases, decoding images takes longer. If necessary, the results are sent by e-mail (the address should be indicated when filling out the forms).
MRI of the heart shows enlarged chambers and inflammatory fibrotic changes in the septum
Functions and work of the human heart: list
Functions and work of the human heart
The heart is the main organ of the human body, and disturbances in its work cause further total disorders, and its failure leads to death. There are several main functions of the human heart. Here is a list of functions and job description:
AUTOMATISM:
- This function is characterized by the independent production of electrical excitation impulses that promote contraction of the heart muscle.
- Due to disruption of this connection, circulatory arrest and further death of a person are possible.
CONDUCTIVITY:
- The structure of the human heart contains conductive pathways that allow the passage of electrical charge within the heart muscle. But it does not act chaotically, but has a certain sequence - from the atrium to the ventricles.
- If the relationship is disrupted, pathological conditions may appear: the development of arrhythmia, heart rhythm disturbances, blockades.
- To correct the situation, medical therapeutic treatment will be required, and in extreme cases, surgical intervention.
REDUCTION:
- In most cases, the cells of the cardiac system provide muscle contraction.
- The mechanism of operation is comparable to the action of the muscles of the iris, biceps, triceps - a signal from atypical cardiomyocytes enters the muscle, under its influence their contraction occurs.
- If muscle contractility disorders occur, a person can experience various types of edema that form due to heart failure.
PUMPING FUNCTION:
- Ensures complete and timely pumping of blood under pressure through the vessels of the human body.
- Pressure is created by the process of contraction and relaxation of the heart.
- If the function fails, human life without additional medical care is impossible.
NUTRITION AND OXYGEN SUPPLY:
- Blood rich in nutrients and oxygen flows through the heart's blood vessels with every contraction of the heart.
- The heart organ is a hollow muscle consisting of four chambers.
- The myocardial septum divides the heart into two parts, each of which has its own functionality. The right half allows venous blood to pass through, pushing it through the artery into the lungs. The left one, receiving blood from the artery, enriched with nutrients and oxygen, conducts it to the aorta, then spreading it throughout the body.
ENDOCRINE FUNCTION:
- The right atrium produces natriuretic hormone, which affects the functioning of the kidneys and the removal of harmful salts from the body.
- It stimulates kidney function while helping to lower blood pressure.
The structure of the human heart is described below. Read on.
Appearance of the fetal heart
The appearance of the heart depends a lot on the period of human development. For example, at the very beginning of fetal development, the heart looks like a tube, which in principle resembles a blood vessel. During the development of the embryo, the walls of such a formation thicken, as muscle fibers begin to actively form, which later become part of the structure of the myocardium. At the same time, the fetal heart has the opportunity to contract.
The first contractile activity of the heart tube is observed on the 22nd day after conception. At first it is weak, but gradually the strength of the contractions increases and after a couple of days blood begins to circulate through the blood vessels of the embryo. Thus, on the 28th day from the beginning of development, the fetus has a primitive blood supply system.
Correct formation of the heart during fetal development allows one to avoid many congenital diseases of this organ. That is why it is extremely important in the first months of pregnancy to avoid various nervous shocks, physical stress, the harmful effects of alcohol, smoking, medications, and infections, which often lead to various heart pathologies.
Chambers in the human heart - structure, quantity: table
Chambers of the human heart
The human heart has four independent main cavities or chambers, separated from each other by partitions, and two additional ones connected to them. Each of them performs its own function. The table below describes the structure and quantity.
| Name | Right cameras | Left cameras |
| Atrium |
There is a flow of blood from the inferior and superior vena cava, bringing venous blood with a high content of carbon dioxide |
The four pulmonary veins drain into the veins and supply blood containing oxygen. |
| Ventricle |
It is connected to the pulmonary artery, which further carries blood to the lungs to enrich them with oxygen. |
The aortic arch departs from the ventricle, through which blood flows to all human organs. It is the largest chamber in size, with a thick layer of muscles. |
| Ear |
|
|
| The main function of the ears is to have a reserve additional volume, which is filled with blood during increased stress. When the heart is functioning well, they hardly function. When the chambers of the heart weaken, the ears, opening towards the atrium, act as a pump, pumping blood into the ventricles | ||
What does an adult's heart look like?
When externally examining a formed and fully developed human heart, one immediately notices an expanded part, or base, and a narrowed part, or apex. The edges of the heart also differ from each other: the left one is more blunt, and the right one, on the contrary, is pointed. The grooves located on the surface of the heart indicate the boundaries within the cavities. The grooves themselves are often covered with fatty tissue, which in pathological cases (with obesity or fatness) is determined throughout the entire musculature of the organ, which does not allow it to function fully.
In a normal state, the weight of the heart averages from 250 to 350 g. In this case, the length of the organ is equivalent to an average of 12-13 cm, width - 9-10 cm, and transverse size - 6-7 cm.
The heart resides and contracts throughout its life in the pericardium, the pericardium. Its role is to protect the heart from other organs. Also in the pericardial sac there is a certain volume of fluid, which in normal condition acts as a “lubricant”, which allows the heart to work smoothly.
In the chest, the heart is located asymmetrically, so outwardly it looks like this: 2/3 of the organ from the center line is to the left, and 1/3 to the right. Also, relative to the longitudinal projection, the heart can have different positions: horizontal, vertical and oblique.
Video How the human heart works
The anterior part of the heart mainly refers to the right ventricle, compared to which the left ventricle is directed posteriorly. Also in front is the right atrium and the adnexal cavity, called the appendage, covering the ascending part of the aorta, is especially noticeable. From the front, the left atrium is almost invisible, while the smaller appendage is in greater contact with the pulmonary trunk.
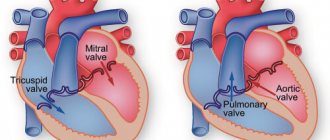
Valves in the human heart - internal structure: diagram with captions
Valves in the human heart - internal structure
Special valves located in the human heart allow blood to flow in a certain direction. Opening one by one, they allow blood to pass through or block its further flow. It is noteworthy that the valves are located along one line of the plane. Above in the picture you can see a diagram with captions.
In the internal structure of the organ there are four valves:
- The mitral valve , a bicuspid valve, is located in the left half of the organ. It consists of two valves that open into the cavity of the ventricles.
- Aortic, tricuspid valve. Located in the lower part of the left ventricle. It prevents backward flow from the aorta.
- Pulmonary tricuspid valve. It regulates the flow of blood into the pulmonary trunk during contraction of the left ventricle, preventing it from returning back.
- The tricuspid or tricuspid valve is located on the right side between the atrium and the ventricle. During contraction, the right ventricle prevents blood from flowing back into the atrium.
Below is even more useful information about the structure of the heart. Read on.
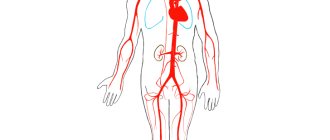
Circulatory system
Circulatory system (animation)
The human cardiovascular system is formed by two circles of blood circulation. With each heartbeat, blood moves in both circles at once.
Pulmonary circulation
- Deoxygenated blood from the superior and inferior vena cava enters the right atrium and then into the right ventricle.
- From the right ventricle, blood is pushed into the pulmonary trunk. The pulmonary arteries carry blood directly to the lungs (to the pulmonary capillaries), where it receives oxygen and releases carbon dioxide.
- Having received enough oxygen, the blood returns to the left atrium of the heart through the pulmonary veins.
Systemic circulation
- From the left atrium, blood moves into the left ventricle, from where it is subsequently pumped through the aorta into the systemic circulation.
- After going through a difficult path, the blood again arrives through the vena cava to the right atrium of the heart.
Normally, the amount of blood pushed out of the ventricles of the heart is the same with each contraction. Thus, an equal volume of blood simultaneously enters the greater and lesser circulation.
What is the difference between veins and arteries?
- Veins are designed to transport blood to the heart, and the job of arteries is to supply blood in the opposite direction.
- In veins, blood pressure is lower than in arteries. Accordingly, the walls of arteries are more elastic and dense.
- Arteries saturate “fresh” tissue, and veins take away “waste” blood.
- In the case of vascular damage, arterial or venous bleeding can be distinguished by its intensity and the color of the blood. Arterial - strong, pulsating, beating like a “fountain”, the color of the blood is bright. Venous - bleeding of constant intensity (continuous flow), the color of the blood is dark.
What structure do the vessels of the human heart have: description
Vessels of the human heart
Like any organ in the human body, the heart also needs nutrients and oxygen. What structure do the vessels of the human heart have? In the structure of the heart, it is customary to distinguish two main arteries that supply blood to the myocardium - description:
- Located on the right side of the organ, it protrudes from the aorta to the back of the heart and provides blood flow to the atrium and ventricle.
- The left artery bypasses the atrium chamber and is located in the anterior groove, supplying blood to the main parts of the heart - the left part, the interventricular wall, and the anterior surface.
The vessels responsible for feeding the heart enriched with blood are called coronary. They branch from the aorta, directly at the valve leaflets. The coronary arteries supply blood to the heart organ, and the coronary veins carry out the outflow of deoxygenated blood.
Functions of the heart - why do we need a heart?
Our blood provides the entire body with oxygen and nutrients. In addition, it also has a cleansing function, helping in the removal of metabolic waste.
The function of the heart is to pump blood through blood vessels.
How much blood does the human heart pump?
The human heart pumps from 7,000 to 10,000 liters of blood in one day. This amounts to approximately 3 million liters per year. That works out to 200 million liters over a lifetime!
The amount of blood pumped per minute depends on the current physical and emotional load - the greater the load, the more blood the body requires. So the heart can conduct from 5 to 30 liters through itself in one minute.
The circulatory system consists of about 65 thousand vessels, their total length is about 100 thousand kilometers! Yes, we didn't make a mistake.
Histology of the heart: what does this human organ look like under a microscope, table
Histology of the heart
The structure of an important organ consists of three main membranes, the cellular structure of which depends on the functions performed. What does this human organ look like under a microscope? In the photo above you see what the histology of heart tissue looks like. More details in the table below. The structure of tissues in section under a microscope looks like this:
| Layer structure | Microscope image |
| Endocardial layer |
|
| Myocardial layer |
|
| Cardiac system | It is possible to consider three types of atypical muscle (cardiomyocytes) cells responsible for transmitting excitation impulses to the layers of the myocardium:
|
| The epicardial layer is the inner side of the pericardium. |
|
Human Heart, Anatomy and Physiology
The human heart is a muscular pump that has been affecting the minds of people for hundreds of years. In 2725 BC e. In Egypt, Imhotep came to the conclusion that the pulse was related to cardiac function. In 400 BC e. Hippocrates wrote about the heart as a strong muscle.
In 1628 William Harvey published an explanation of the process of blood circulation. Between 1857 and 1882, Marey and Dudgeon, independently of each other, created a machine for measuring blood pressure when hypertension was detected in a person.
In recent years, molecular biology has helped to reveal even more complex functions of this engineering masterpiece - the human heart. which confirms the words of the psalmist that you and I are “wonderfully made” (Psalm 139:14).
The term "cardiovascular" describes the heart and blood vessels of the body. Blood vessels are also sometimes called the vascular tree, or bed. In this article we will look at the structure and functions of the human heart.
The heart is a hollow muscular organ that is located in the central part of the chest, but most of it is to the left of the midline.
The human heart consists of two upper chambers called atria and two lower chambers called ventricles. Structurally and functionally, the heart is divided into right and left parts; the right side pumps blood to the lungs, the left side pumps blood throughout the body.
The upper chamber, or atrium, collects blood and pumps it into the ventricle, which then pumps it out of the human heart into the great vessels. To ensure blood flows in one direction, each ventricle has inlet and outlet valves.
Left ventricle.
Blood enters the left ventricle from the left atrium through the mitral valve, which consists of two large leaflets that open when the ventricle is relaxed (diastole).
When the filling of the ventricle is completed and it contracts, the force of contraction “presses” the blood to the bottom of the mitral valve leaflets, causing the valve to close. Thanks to this mechanism, blood flows in one direction - from the ventricle to the aorta.
The outlet valve of the left ventricle is called the aortic valve. It has three leaves, or leaflets, that open during contraction of the ventricle, allowing blood to enter the systemic circulation.
As the ventricle relaxes and its pressure drops below the pressure in the aorta, blood begins to flow back (from the aorta into the ventricle).
This reverse flow of blood causes the aortic valve leaflets to fill from above and thus move closer to each other (touching each other) and slam shut. The valve closes and blood does not flow back into the left ventricle.
Right ventricle.
The inlet valve is a tricuspid valve, which by definition consists of three leaflets. It provides one-way blood flow from the right atrium to the right ventricle.
The blood is then released into the pulmonary artery through the pulmonary valve (consists of three leaflets) and flows to the lungs. The tricuspid and pulmonary valves close and open according to the same principles as the mitral and aortic valves, respectively.
The cusps of the mitral and tricuspid valves are attached to the walls of the ventricles by “cords” of tissue and muscle called chordae tendineae and papillary muscles.
These structures keep the valves from opening backwards, which would cause blood to flow backwards. If these valves, threads or muscles are damaged due to disease processes, then the valves do not close completely and may “leak” (valve insufficiency).
There are also diseases that cause the valves to narrow, which in turn causes a reduction in blood flow through the valves.
As a result, the human heart constantly overcomes increased resistance and increases in size. However, over time, it depletes its reserve of strength and can no longer pump blood as efficiently, which affects the health of the entire body.
The valves can also be affected by both processes at the same time (narrowing and leaking), resulting in weakened cardiac function and impaired circulation.
Cardiac function.
The cardiac function is to pump blood through the systemic circulation (whole body) and the small circulation (pulmonary). The right side of the heart pumps blood to the lungs, where carbon dioxide is removed and oxygenated.
The left side of the heart pumps blood to the rest of the organs; in this way oxygen and nutrients are delivered to them. Waste also enters the bloodstream, but this time through the venous system, so that it is subsequently removed from the body by organs such as the lungs, kidneys and liver.
The contraction and relaxation of the heart is a cardiac cycle that can be felt by feeling the pulsation of blood flowing through the arteries. This can be done by pressing the arteries against the bone, for example in the wrist, lower leg, neck.
Arterial pulsation is created by the build-up of a pressure wave that flows through human arteries from the heart and causes pulsatile expansion of the arterial walls. If we count this pulsation for 60 seconds, we get the pulse rate. In a healthy adult, it is approximately 72 beats per minute (normal range is 65 to 90).
Each cardiac cycle consists of two phases: diastole and systole.
Diastole (or relaxation of the heart muscle) During this phase, the heart muscle relaxes in order to accept a certain volume of human blood flowing into the lumen of the heart. The atria then contract to move blood into the ventricles.
Systole.
The next phase is called systole, or ventricular contraction, during which blood is pumped out of the heart. The atria begin to relax in order to accept additional blood to repeat the cycle.
You can not only feel the pulse, but also monitor the cardiac cycle by listening to heart sounds through the chest wall using a stethoscope. These sounds are described as "lub-dub", where the first "lub" sound indicates the closure of the mitral and tricuspid valves, and the second "dub" sound indicates the closure of the aortic and pulmonary valves.
Additional sounds usually indicate some kind of abnormality of the heart valve and/or muscle function. The most common sounds that indicate valve dysfunction are called murmurs.
These sounds are produced when turbulent blood flow occurs due to structural changes in the valve apparatus. Normally, blood flow is smooth, linear and non-turbulent (non-swirling).
Electrical activity of the heart in humans.
In order for the heart to beat in an orderly manner, it is equipped with nerve pacemakers (a collection of nerve cells in the atria) and a special conduction system that delivers nerve impulses to the heart muscle.
Different parts of the conduction system and even parts of the heart itself are capable of beating at different rates. The conduction system provides sequential, coordinated activation from the atria to the ventricles.
This electrical system ensures that impulses reach all parts of the heart muscle. The electrical axis of the heart is determined using electrocardiogram (ECG) data.
Human cardiac cycle
Human cardiac cycle
In a state of physical and psycho-emotional calm, the heart contracts in the range of 70-80 cycles per minute . One cycle occurs in 0.8 seconds, of which:
- It takes 0.1 seconds for the atria to contract
- 0.3 fractions of a second are spent on the ventricles
- 0.4 remains for the relaxation period
The frequency of the cycle is determined by the heart rhythm: the area of the heart muscle where impulses occur that control the frequency of contractions.
The work of the heart goes through two main phases:
- Ventricular contraction or systole . Venous blood pushes through the pulmonary artery into the vessels of the lungs. There it is saturated with oxygen and then, enriched, it is collected in the left atrium.
- Pause or diastole . The period of relaxation of the heart muscle. At this time, the pockets of the left atrium are filled with blood, then it passes into the left ventricle and, pushed through the valve, goes to the aorta, scattering throughout the body. The blood continues its movement, collecting in the right atrium and then flowing into the right ventricle.
Rhythmic, stable alternation of the phases of calm and contraction is ensured by the appearance and conduction of an electrical nerve impulse through a special system of conducting cells. The impulse originates in the superior sinus node, located in the right atrium. Next, it enters the atrioventricular node and passes along the fibers to the muscles of both ventricles, causing them to contract.
Unusual Facts About the Heart
- The heart rate in a fetus is several times higher than in an adult, and is approximately 140 beats/min, while after 10 weeks the volume of circulating blood is equal to 60 l/day.
- In an adult, the heart rate is approximately 72 times/day, so over the course of approximately 65 years, more than 2 million heartbeats are detected.
- The total length of all blood vessels is more than 120 million meters, which allows you to circle the Earth three times along the equator.
- Blood vessels also pass through adipose tissue, and with obesity, the heart has to pump blood through vessels more than 8 thousand kilometers long.
- One cycle of blood supply lasts approximately 23 seconds and is approximately the same time it takes a person to run 200 meters.
- In one cubic milliliter of blood, there are about 5.5 million red blood cells, which are also called red blood cells. It takes 120 days to fully update them.
- Heart disease is the most common cause of human death. It has been proven that cardiovascular diseases have claimed more lives than all the wars in the entire history of mankind.
Video 10 unknown facts about the human heart. I Vam Science
4.80 avg. rating ( 94 % score) – 5 votes – ratings
Position of the human heart: types, size
Position of the human heart
The size or size of the heart, its position in the human sternum depends on many factors:
- Floor
- Age
- Physiological indications
- Hereditary predisposition
Based on the location of the organ in the human body, there are three types:
- Oblique position . The most common type. The angle of inclination of the placement relative to the cardiac axis is about 45° .
- Horizontal . The silhouette of the heart on x-ray shows a nearly recumbent position. The angle of inclination relative to the axis shows from 35° .
- Vertical arrangement . The silhouette of the heart shows an almost standing position. Tilt angle from 50° to 56°.
Representatives of the brachymorphic type of body structure, with a wide chest and a high position of the diaphragm, have a horizontal heart. People of the dolichomorphic type with a long, narrow chest often have a vertical arrangement of the organ. Consequently, even focusing on the body shape and appearance of the chest, we can talk about the position of the heart organ. A person's gender also affects the position and size of the heart. In women, the heart is more often located horizontally.
The size of the heart muscle directly depends on a person’s age, gender, body weight and height. Its value is influenced by external factors - working conditions, place of residence. The heart increases along with body weight, height, and muscle development. The latter indirectly affects the fact that women's heart muscle is smaller than men's.
Heart diseases
It is not surprising that the number of cardiovascular diseases is increasing in the world. The heart is a complex organ that actually rests (if it can be called rest) only in the intervals between heartbeats. Any complex and constantly working mechanism itself requires the most careful treatment and constant prevention.
Just imagine what a monstrous burden falls on the heart given our lifestyle and low-quality, abundant nutrition. Interestingly, mortality from cardiovascular diseases is also quite high in high-income countries.
The huge amounts of food consumed by the population of wealthy countries and the endless pursuit of money, as well as the associated stress, destroy our hearts. Another reason for the spread of cardiovascular diseases is physical inactivity - catastrophically low physical activity that destroys the entire body. Or, on the contrary, an illiterate passion for heavy physical exercise, often occurring against the background of heart disease, the presence of which people do not even suspect and manage to die right during “health” activities.
Lifestyle and heart health
The main factors that increase the risk of developing cardiovascular diseases are:
- Obesity.
- High blood pressure.
- Increased blood cholesterol levels.
- Physical inactivity or excessive physical activity.
- Abundant, low-quality food.
- Depressed emotional state and stress.
Make reading this great article a turning point in your life - give up bad habits and change your lifestyle.
We have a separate article on our website about how to keep your heart and blood vessels healthy.
The structure of the human heart: age characteristics
The structure of the human heart
After the birth of a child, the heart not only increases in size, it changes its appearance and its proportions. The heart muscle of a newborn lies horizontally and has a spherical shape. At the end of the first year, when the baby begins to actively move, stand and walk, the heart moves into an indirect position. At the age of ten it reaches adult size. Age-related features of the structure of the human heart:
- The ratio of the size of an important organ in relation to body weight in a child is greater than in an adult.
- It grows most rapidly at the beginning of life.
- At 8 months, the heart doubles in size compared to its original size, by the age of 3, three times, at 5 years its mass is multiplied by 4 , and at the age of 16, it increases by 11 times .
Initially, the size and mass of the heart of boys is larger than that of girls. But at the age of 12-13 , during the period of hormonal surge and increased growth of girls, it overtakes and becomes larger. At the age of 16, the girl’s heart size is again inferior in size.
The condition of the entire body depends on the full functioning of the heart muscle, so keeping it healthy is one of the priorities. To avoid the appearance of cardiac pathologies, it is necessary to pay attention to the factors influencing their development:
- A sharp jump in body weight, excess weight
- Bad habits: smoking, alcohol
- Consumption of large amounts of food harmful to the body, irrational diets
- Intense physical activity or, on the contrary, a sedentary lifestyle
- Psycho-emotional conditions: chronic stress, nervous overstrain
Knowing the anatomy of the structure of the heart, its importance in the structure of the body, it is important to make a small effort by giving up habits that are harmful to health. Now you know about the structure of the heart, its functions and age-related characteristics. Good luck!
Preparing for cardiac MRI
Magnetic resonance imaging does not require special organizational measures on the eve of scanning. Before a cardiac MRI, there is no need to follow a diet, stop or take any medications.
Women of reproductive age should make sure that there is no pregnancy (the procedure is contraindicated in the early stages). The best option is to take a blood test for hCG or undergo a urine test. After week 13, native (without contrast enhancement) cardiac tomography can be performed.
Persons with metal implants (endoprosthesis, vascular clips, pins, etc.) will need to obtain a document on the compatibility of the product with a magnetic field. A passport or an extract from the medical institution where the structure was installed will do. After vascular stenting, MRI can be performed no earlier than six months later. The time of the operation must be confirmed with the appropriate certificate. The presence of a pacemaker, defibrillator or other electronic device is an absolute contraindication to MR scanning of any anatomical area. Devices may stop working under the influence of the magnetic field of the tomograph.
It’s worth organizing a light snack 40-45 minutes before leaving the house. Yogurt, a small sandwich or fruit, or an egg will do. This measure will allow you to avoid the manifestation of vegetative reactions (nausea, vomiting, dizziness, etc.) to the drug.
Women supporting lactation can undergo MRI. But you need to purchase formula for the baby in advance or stock up on expressed breast milk for 2-3 times. Natural feeding can be resumed 6-12 hours after contrast administration.
Children undergo MRI if they remain motionless during the scan. If the child is not able to lie for 20-30 minutes in one position, tomography is performed under anesthesia in a hospital setting or an alternative method is found.
Heart rate and blood pressure
The beating heart, by regularly pumping blood out of the ventricles, causes a pulsating movement of the artery walls, called the pulse. This is one of the parameters with which you can easily evaluate the heart rate and elasticity of blood vessels.
Heart rate can be examined using a camera or by touch (palpation) on arteries close to the surface of the skin, most often the arteries:
- jugular
- humeral
- radial
- femoral
During diagnosis, its frequency, amplitude and regularity are also assessed, as well as the duration of the systolic wave or the presence of murmurs over the arteries.
The correct heart rate for an adult at rest is approximately 70 beats per minute. These values increase especially after drinking alcohol, coffee, in stressful situations or after exercise.
Too high pulse values, in the range of 180-200 beats per minute, indicate sinus tachycardia, which requires in-depth diagnosis.
The second parameter that is crucial for assessing the state of the cardiovascular system is blood pressure. This is the pressure that flowing blood exerts on the walls of blood vessels. Pressure values depend on many factors, including:
- force of contraction of the heart muscle,
- diameter and degree of filling of vessels,
- patient's age,
- and even the time of day.
Blood pressure is characterized by two values:
- systolic pressure
- and diastolic pressure.
The first value is the maximum pressure that the blood reaches when the heart contracts, pumping it throughout the body. Diastolic pressure is when the heart is in the diastolic phase and is the minimum blood pressure level between heartbeats.
Normal blood pressure readings should be between 120 and 129 (systolic) and between 80 and 84 (diastolic).
Blood pressure may increase with age, but repeated readings above 140/90 mmHg. indicate high blood pressure that requires treatment.
Anatomy of the human heart: historical and medical excursion
Cardiology, a science that studies the structure of the heart and blood vessels, was identified as a separate branch of anatomy back in 1628, when Harvey identified and presented to the medical community the laws of human circulation. He demonstrated how the heart, like a pump, pushes blood through the vascular bed in a strictly defined direction, supplying the organs with nutrients and oxygen.
The heart is located in the human thoracic region, slightly to the left of the central axis. The shape of the organ may vary depending on the individual structural features of the body, age, constitution, gender and other factors. Thus, dense, short people have a more rounded heart than thin and tall people. Its shape is believed to be approximately the circumference of a tightly clenched fist, and its weight ranges from 210 grams for women to 380 grams for men.
The volume of blood pumped by the heart muscle per day is approximately 7–10 thousand liters, and this work is carried out continuously! The amount of blood may vary due to physical and psychological conditions. Under stress, when the body needs oxygen, the load on the heart increases significantly: at such moments it is able to move blood at a speed of up to 30 liters per minute, restoring the body’s reserves. However, the organ is not able to constantly work for wear and tear: during moments of rest, blood flow slows down to 5 liters per minute, and the muscle cells that form the heart rest and recover.
Heart diseases
The heart is exposed to many negative factors throughout its life, which makes it susceptible to various diseases. For many years, cardiovascular disease was the leading cause of death, much more dangerous than cancer.
Cardiac ischemia
Coronary heart disease - otherwise coronary heart disease - is a chronic disease caused by hypoxia of heart muscle cells, leading to its failure. This is mainly caused by:
- atherosclerosis (an insidious disease in which excess cholesterol and other lipids are deposited on the walls of the arteries),
- less commonly, blockage, narrowing or underdevelopment of the coronary arteries,
- some injuries
- or after carbon monoxide poisoning.
Coronary artery disease is also called angina because its symptoms include severe pain and shortness of breath in the chest during exercise. The pain can spread (most often on the left) to the arms, hands and even jaws.
Myocardial infarction
Myocardial infarction, also known as heart attack, is necrosis of the heart muscle caused by ischemia. This is caused by the closure of the coronary vessel that carries blood to the heart.
Previous coronary heart disease and atherosclerosis are the cause of myocardial infarction in more than 90% of cases.
Myocardial infarction is usually sudden, severe, and manifests itself with severe pain in the chest area. Patients also complain about:
- feeling of shortness of breath,
- breast expansion,
- nausea
- and vomiting.
A heart attack is a very serious disease with a high mortality rate, often leading to many complications and can permanently damage the heart as a pump.
Heart attacks are being diagnosed in increasingly younger people, mostly men under 45, burdened by stress and an unhealthy lifestyle.
Cardiac arrhythmia
Heart rhythm disturbances - so-called cardiac arrhythmias - are a large group of disorders that can be divided into 2 types:
- Supraventricular arrhythmias (such as atrial fibrillation, nodal or atrioventricular tachycardia)
- and ventricular arrhythmias.
Supraventricular disorders are usually found in people without additional heart disease and may be a risk factor for future cardiovascular disease (such as stroke).
Ventricular arrhythmias (including additional ventricular contractions, ventricular fibrillation, ventricular tachycardia) are, in turn, very serious diseases, usually associated with the need to call an ambulance and treatment in a hospital.
There can be many causes of arrhythmias: from complications of coronary heart disease to acquired and congenital heart defects, genetically determined diseases of the conduction system or arterial hypertension.
Arrhythmias can manifest themselves, for example:
- palpitations and tachycardia (i.e. heartbeat too fast)
- feeling short of breath
- dizziness
- fainting.
Myocarditis
Myocarditis - unlike the previously mentioned diseases - this disease occurs as a complication of past infections:
- viral (such as influenza, chickenpox, or rubella)
- or bacterial (staphylococcal, salmonella or pneumococcal infections).
- In young people, this inflammation may also have an autoimmune basis.
Symptoms accompanying this disease:
- rapid fatigue during any physical activity,
- dyspnea,
- heartbeat,
- heat.
Untreated heart inflammation can cause fibrosis to replace normal cells, leading to a significant reduction in heart muscle performance.
Valve defects
Valve defects are a congenital or acquired disease (for example, after severe infections). The most common types of valve defects include:
- valve stenosis - when a narrowed blood outlet makes it difficult for blood to pump properly,
- and valvular regurgitation, which leads to “leakage” of blood and its outflow.
Due to valve defects, the heart works harder and harder, and the disease worsens. Symptoms may include:
- dyspnea,
- chest pain,
- dizziness
- or swelling around the ankles and feet.
Diagnosis of heart diseases
The first tests performed when heart disease is suspected are non-invasive tests that will help rule out other causes if a patient has nonspecific symptoms.
These are the most common:
- Blood tests - in addition to standard blood tests, so-called specific cardiac markers are very useful, that is, enzymes whose concentration increases due to hypoxia and damage to heart muscle cells. The most popular markers are troponins (cTn) and creatine kinase (CK) or B-type natriuretic peptide (BNP). However, such results should be analyzed very carefully because, for example, increased troponin concentrations occur after exercise such as running and this does not indicate a pathological condition.
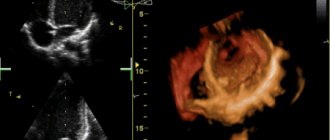
- Magnetic resonance imaging (NMR) is currently one of the most accurate and popular methods of in-depth non-invasive diagnostics in cardiology. It allows you to visualize the processes occurring in the heart, and thanks to its high image resolution, it also allows you to differentiate tissues and evaluate their functions.
- Echocardiography is an ultrasound examination that allows you to evaluate the internal structure of the heart and possible abnormalities.
- Electrocardiogram - This can be used to measure the bioelectrical activity of the heart. It is safe and cheap, with its help you can detect, for example, chronic disorders of the blood supply to the heart, arrhythmia and even the so-called “Silent” myocardial infarction (a previous asymptomatic heart attack that leaves a permanent mark on the heart muscle).
Coronary angiography is an invasive test used in cardiology that requires the patient to stay in the hospital. In this method, a contrast agent is injected into the patient's body through one of the arteries, allowing the coronary network to be visualized on an x-ray image.
Conduction system of the heart
The rhythmic contractions and contractions of the heart and its regular functioning would not be possible if it were not for electrical impulses and regular muscle stimulation maintained by the so-called conduction system of the heart. This consists of:
- sinoatrial node,
- atrioventricular node,
- His bundle,
- Purkinje fibers.
The sinoatrial node, also known as the “pacemaker,” has the ability to spontaneously generate electrical stimulation. Its work can be compared to a simulator that determines the heart rate.
Impulses continue to spread to other structures of the heart through the atrioventricular node, which slows the conduction of impulses and prevents simultaneous contraction of the ventricles and atria. The bundles of His and Purkinje fibers branch out across the cardiac septum and ultimately deliver impulses to the ventricular fibers.
The efficient functioning of the conduction system of the heart ensures the correct rhythm of the heart muscle and subsequent contraction of the atria and ventricles. To evaluate whether this system is working properly, an electrocardiogram (ECG) is performed, which analyzes the electrical activity of the heart.
What harms our heart the most?
Unfortunately, we cannot influence a number of elements that may be a potential factor in the development of cardiovascular diseases. This is for example:
- age (men>55, women>60),
- male gender,
- premature menopause,
- heredity.
However, in developed societies, heart disease is affecting more and more young people. It turns out that our health is greatly influenced, first of all, by our lifestyle. Increasingly long hours of sedentary work, computer and television entertainment, and poor diet are the main culprits for such high rates of cardiovascular diseases.
Doctors list several of the most important risk factors for heart disease:
- overweight and abdominal obesity
- smoking
- little physical activity
- high cholesterol
- alcohol abuse
Experts indicate that about 150 minutes of moderate-intensity aerobic physical activity (such as walking or jogging) will greatly improve our heart health and function.
Combined with a less fatty diet and quitting smoking, regular exercise is sure to be the key to health and our heart's best friend. In keeping with the principle that prevention is better than cure, let's join elgreloo.com to take care of heart prevention and enjoy a long life.