Published: 05/27/2021 11:45:00 Updated: 05/28/2021
Coronary heart disease is a chronic or acutely developing disease characterized by partial or complete cessation of blood supply to the heart muscle.
The cause of this phenomenon is spasm and thrombosis of the coronary arteries, usually due to their atherosclerotic changes.
Organ ischemia is most often manifested by paroxysmal chest pain - angina pectoris; with a sharp and pronounced disturbance of blood flow in the vessels, myocardial infarction develops.
What is coronary heart disease?
Coronary heart disease is a very broad concept that includes many pathological conditions: from angina pectoris to myocardial infarction with its complications and consequences. IHD occurs when the heart muscle lacks its own blood supply and there is a discrepancy between the myocardium's need for oxygen and its delivery.
Oxygen-rich blood is delivered to the heart muscle through vessels called coronary arteries. When these vessels are damaged, coronary circulation is disrupted, and the myocardium finds itself in conditions of hypoxia (oxygen starvation), which leads to persistent disruption of the functioning of the heart.
The course of the disease, its forms and complications
Classification of IHD
differs from the classifications of other diseases: since coronary disease itself is a state of imbalance between the supply of oxygenated blood to the myocardium and the heart’s need for it, it is difficult to draw an unambiguous line between its forms and complications.
Thus, both myocardial infarction and heart failure are both clinical forms of the disease (acute and chronic
) and complications caused by a lack of myocardial oxygenation.
In this regard, the medical community talks about the clinical classification of forms of coronary artery disease
in the following order:
- Sudden coronary
death (cardiac arrest).
- Angina pectoris
: distinguish between angina pectoris (new, stable, unstable or progressive) and angina at rest (spontaneous/vasospastic/variant/Prinzmetal).
- Myocardial infarction.
- Post-infarction cardiosclerosis.
- Heart
failure (acute and chronic).
- Violations heart
rhythm.
- Silent myocardial ischemia.
- Hibernating myocardium.
- Stunned myocardium.
- Syndrome X.
The development of the disease is not linear, and clinical forms can replace each other. If you do not follow the recommendations of your doctor, chronic forms of IHD
may be complicated by an acute form (heart attack or sudden
coronary
death).
At the same time, after an acute form of IHD (the same heart attack), chronic
consequences
of ischemia
in the form of post-infarction cardiosclerosis
Both acute and chronic forms of IHD can lead to serious consequences for the body
Why does pathology occur?
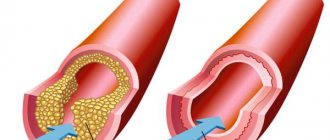
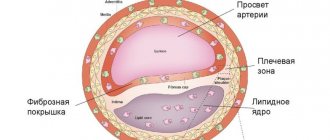
The main cause of the disease is damage to the coronary arteries by atherosclerosis, in which cholesterol plaques appear in the vessels. After some time, a blood clot may form at the site of the plaque, which partially or completely blocks the artery, blocking the supply of oxygen to the heart muscle.
As a rule, narrowing of the lumen of the vessel up to 50% occurs without any clinical manifestations. Vivid symptoms appear when the artery is blocked by 70% or more.
Very rarely (up to 5% of cases) IHD is caused by:
- congenital anomalies of the origin of the coronary arteries;
- Marfan, Ehlers-Danlos syndromes - hereditary pathologies of connective tissue;
- infective endocarditis - inflammation of the inner lining of the heart caused by pathogenic pathogens;
- Kawasaki syndrome is a systemic vasculitis affecting medium and small arteries;
- syphilitic aortitis is a complication of syphilis, in which inflammation of individual layers or the entire thickness of the aortic wall occurs;
- overdose of vasoconstrictors, narcotic drugs.
Treatment
Treatment for coronary heart disease usually involves lifestyle changes and, if necessary, certain medications and medical procedures.
Lifestyle change.
By deciding to start a healthy lifestyle, you will begin a long journey leading to the health of your arteries:
- Quit smoking
- Eat healthy
- Regular exercise
- Fighting excess weight
- Limiting stress
Drugs
Various drugs are used to treat IHD:
Modifiers of fat metabolism.
By lowering the level of low-density lipoprotein, these drugs reduce the substrate deposited in the arteries. The use of high-density lipoproteins also reduces cholesterol deposition. Your doctor will be able to choose a drug from a variety of groups, such as statins, niacin, fibrates, and bile acid sequestrants.
Aspirin.
Your doctor may recommend taking aspirin or another antiplatelet drug daily. These drugs reduce the blood's ability to clot, which helps prevent blood clots in the coronary arteries. If you've already had a heart attack, aspirin can help prevent further attacks. In some cases, aspirin should not be taken, such as if you have a bleeding disorder or if you are taking another anticoagulant. So you should first consult your doctor.
Beta blockers.
These drugs slow the heart rate and lower blood pressure, which reduces the heart's need for oxygen. If you have had a heart attack, taking beta blockers can help prevent further attacks.
Nitroglycerine.
Nitroglycerin relieves angina pain by dilating the coronary arteries and reducing the heart's need for oxygen.
Angiotensin-converting enzyme inhibitors and angiotensin II receptor blockers.
These similar drugs lower blood pressure and prevent the progression of coronary artery disease. If you have had a heart attack, taking these medications will help reduce your risk of subsequent attacks.
Calcium channel blockers.
These drugs relax the coronary arteries, which improves blood flow to the heart. They also control hypertension.
Procedures that improve blood flow
Sometimes more aggressive treatment is required:
Coronary artery stenting
Angioplasty and stenting.
For this procedure, the doctor inserts a long, thin tube (catheter) into the narrowed area of the coronary artery. A deflated balloon is placed into this area. This balloon is then inflated, widening the artery. The stent usually remains in the lumen of the vessel to prevent re-narrowing of the artery.
Coronary artery bypass grafting (CABG).
The surgeon creates a shunt that bypasses the blocked section of the coronary artery, using vessels from other parts of the body. This allows blood to be delivered to the heart by bypassing a narrowed or completely closed section of the coronary artery. Since this requires open heart surgery, CABG is performed in cases of multiple lesions of the coronary arteries.
Risk factors
Risk factors for developing CHD include:
- dyslipidemia - high levels of lipids and/or lipoproteins in the blood;
- diabetes. The disease itself does not cause narrowing of the coronary arteries, but it significantly complicates the course of atherosclerosis;
- arterial hypertension;
- excess body weight;
- smoking. Smoking patients suffer from atherosclerosis more often and more severely. They develop multifocal arterial damage: atherosclerosis affects not only the arteries of the heart, but also the vessels responsible for the blood supply to the brain, head tissue, upper and lower extremities, and kidneys;
- sedentary lifestyle;
- male gender;
- heredity - the presence of atherosclerosis, ischemic heart disease, and arterial hypertension in close relatives.
It is worth noting that a hereditary factor causes IHD only in 20% of cases. Most often, the disease is a consequence of an unhealthy lifestyle.
Causes
Atherosclerosis
It is believed that IHD begins with damage to the inner layer of the coronary arteries, sometimes from childhood. Damage can be caused by various factors such as:
- smoking;
- arterial hypertension (high blood pressure);
- high cholesterol;
- diabetes;
- radiation therapy to the chest (used for some types of tumors);
Once the artery wall is damaged, fatty deposits, consisting of cholesterol and cellular breakdown products, begin to accumulate in the vessel. This process is called atherosclerosis. When these plaques begin to disintegrate and crack, platelets from the bloodstream try to close the defect, forming a blood clot. The resulting blood clot can block a coronary artery, which in turn can lead to a heart attack.
Clinical forms of the disease
When diagnosing IHD, the clinical form of the disease must be indicated. The differential diagnosis of angina pectoris or myocardial infarction, the most common manifestations of coronary artery disease, is of key importance. Other clinical forms of IHD are much less common.
Angina pectoris is a type of coronary artery disease that manifests itself as chest pain. A dangerous condition is unstable angina, in which an exacerbation of coronary heart disease occurs and the prerequisites for the development of myocardial infarction appear.
Myocardial infarction or heart attack is a critical manifestation of coronary artery disease. During a heart attack, a coronary artery becomes obstructed, which can lead to serious damage or complete death of the myocardium.
Types of cardiac ischemia
- Angina (stable and unstable) is chest pain caused by a lack of oxygen supply to the myocardium.
- Myocardial infarction (primary, repeated) - partial or complete blockage of the artery through which blood flows to the heart.
- Post-infarction cardiosclerosis is the presence of parts of the heart that died during a heart attack and which were replaced by connective tissue.
- Heart failure is a violation of the pumping function of the heart, as a result of which the body does not receive sufficient oxygen supply.
- Sudden arrhythmic death is the death of a person within an hour after the onset of acute manifestations of the disease.
Symptoms of coronary heart disease
The main symptom of the disease is pain behind the sternum, which can radiate under the shoulder blade, to the left arm, neck, and lower jaw. The more pronounced the ischemia, the more severe the pain becomes.
As the pathology develops, the level of physical activity at which pain occurs becomes less and less significant. For example, if at the beginning of the disease a person felt pain in the heart area when climbing the stairs to the fifth floor, then with severe narrowing of the arteries, pain can occur even during normal everyday activities (cleaning the apartment, preparing food, brushing teeth).
With myocardial infarction, the pain behind the sternum becomes very severe and is not relieved even by nitroglycerin. Also during a heart attack a person may experience:
- nausea, vomiting;
- tachycardia;
- dyspnea;
- dizziness;
- cold sweat;
- panic attack;
- fainting.
Symptoms and forms of IHD
With different forms of coronary heart disease, symptoms may differ. There are several forms of the disease.
Angina pectoris
The condition is characterized by attacks of squeezing or burning pain behind the sternum, which usually appears during physical and emotional stress.
It can radiate to the left arm, neck, shoulder, lower jaw, subscapular region, upper abdomen. For this reason, angina pectoris is also called “angina pectoris.” The duration of pain is usually several minutes. Depending on the stability of the course of the disease, stable and unstable forms of angina are distinguished. The first occurs only after physical or psycho-emotional stress, with increased blood pressure, tachycardia. As the disease progresses, the amount of activity available to a person decreases, and in the fourth class of pathology, he can no longer make any movement without developing attacks of chest pain.
Unstable angina can be new - a month or less after the onset of symptoms, progressive and early post-infarction. Progressive angina is characterized by a decrease in the load tolerated, for example, a decrease in the distance that a person can walk without the appearance of symptoms.
Unstable angina requires examination and treatment in a hospital; the risk of myocardial infarction is high.
Myocardial infarction
Develops acutely.
Due to a prolonged decrease in blood flow or its complete cessation to certain areas of the heart muscle, necrosis of the area of the heart muscle occurs - necrosis. The affected area can be of different sizes depending on the diameter of the affected vessel, which is why the disease is often called large-focal or small-focal myocardial infarction. The pain in this condition is intense, pressing and squeezing in nature, and attacks of burning “dagger” pain are also common. In many patients, it has a typical localization in the retrosternal region, but it can also involve the area to the left of the sternum or spread to the entire surface of the chest. In this case, the patient experiences “fear of death”, melancholy, a feeling of doom arises, and may be restless and very excited.
The localization of pain during myocardial infarction can be almost any; for example, sometimes pain occurs even in the abdomen. There is also a painless form.
With small focal lesions, the symptoms may be blurred, and diagnosis by ECG can be difficult.
Spontaneous Prinzmetal ischemia
Substernal pain occurs against the background of spasm of the coronary vessels and is not associated with exercise. Most often, the condition develops at night, between midnight and eight o'clock in the morning. Spastic angina is characterized by regularity and cyclicity, often repeating several attacks in a row with a short interval.
Post-infarction cardiosclerosis
After a heart attack, dead muscle cells are replaced with connective tissue. In this case, conductivity in the myocardium is disrupted, which may be accompanied by sensations of interruptions in the work or prolonged cardiac arrest, periodic fainting and dizziness. There may also be attacks of rapid heartbeat, chest pain, shortness of breath, pale or blue discoloration of the skin.
Heart failure
A disease in which the heart cannot fully perform its function of providing the tissues of various organs with a sufficient amount of blood. The condition is manifested by shortness of breath, swelling, fatigue, and poor tolerance to physical activity.
Heart rhythm disturbances
Arrhythmias are of various types. Accompanied by a feeling of palpitations or a decrease in heart rate. The patient may experience severe weakness, dizziness, nausea, and possible loss of consciousness. There are also asymptomatic forms of pathology, which become an accidental finding on the ECG.
Silent myocardial ischemia
It occurs without characteristic attacks of angina pectoris. It is usually detected accidentally on an ECG and after special diagnostic exercise tests.
Sudden cardiac death
More often it occurs due to ventricular fibrillation or flutter - erratic contraction of the heart muscle at high frequency. The condition develops unexpectedly and is manifested by the following symptoms:
- weakness;
- dizziness;
- loss of consciousness;
- noisy and rapid breathing;
- dilated pupils;
- decrease in respiratory rate;
- absence of heart contractions.
Sometimes the heart can be returned to the correct rhythm, but if this was not done in the first minutes, then the brain cells die from hypoxia, and an irreversible coma develops.
How is diagnosis carried out?
If coronary heart disease is suspected, a thorough examination of the patient is carried out, which may consist of various diagnostic tests:
- Blood chemistry.
When conducting a biochemical blood test, a lipid profile is necessarily performed, aimed at determining the level of lipids (fats) of various blood fractions. Lipid profile indicators include:
- total cholesterol;
- low and high density lipoproteins;
- triglycerides;
- atherogenic coefficient.
Also, during a biochemical study, the level of glucose, C-reactive protein, and creatinine is determined.
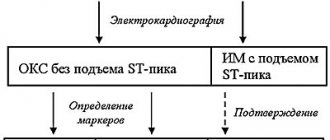
- Electrocardiography (ECG).
Electrocardiography is a method of recording and studying the electric fields that arise during the work of the myocardium. If a patient has coronary artery disease, characteristic changes in the ST segment and T wave appear on the ECG.
In addition to the classic ECG, which is performed at rest, ECG tests with physical activity can be used. For example, such tests include bicycle ergometry - a technique for conducting an ECG under conditions of dosed exercise on an exercise bike. This functional test allows you to identify hidden (asymptomatic) IHD and determine blood flow reserves during physical activity.
Another ECG method that can be used to diagnose coronary artery disease is Holter monitoring, which monitors the work of the heart throughout the day. Electric fields are recorded using a portable device - a Holter monitor.
- Echocardiography (ultrasound of the heart).
Echocardiography reveals a wide range of changes in myocardial function that are not always detected during an ECG. During the examination, the doctor can see on the monitor the condition of the heart valves and changes in the size of the myocardial cavities. Echocardiography with Doppler can detect vascular damage and impaired blood flow.
Ultrasound of the heart can be performed both at rest and under conditions of dosed physical activity.
- Scintigraphy.
Study of the heart muscle by introducing radioactive isotopes into the body and subsequently recording their radiation. The uptake of isotopes by heart cells occurs in proportion to the blood flow in it. Therefore, in the presence of affected vessels, the scintigram (image of the myocardium) reveals areas of reduced accumulation of the pharmaceutical.
- Coronary angiography.
This technique is the gold standard in diagnosing coronary artery disease and assessing the degree of arterial damage. During the procedure, a contrast agent is injected into the right and left coronary arteries through catheters. After this, using an X-ray machine, images of the vessels are taken in different projections, which makes it possible to assess their patency. Based on the results of the study, further treatment tactics are selected.
Measures to prevent cardiovascular pathology
To avoid developing heart disease, you need to stop smoking and reduce your alcohol consumption.
Severe stress is also one of the predisposing factors to the occurrence of IHD. It is impossible to remove stress from life, but you can react to it correctly: humans are evolutionarily designed in such a way that muscle work is necessary after any stress. If you are worried or upset, then you need to squat, jog, or walk – the muscles should get tired. In case of severe anxiety, you may need to use sedatives, for the selection of which you need to consult a doctor.
Regular exercise with moderate physical activity is useful for the prevention of ischemia. You also need to monitor your weight and blood pressure. All persons over 40 years of age must be examined annually - take a biochemical blood test to check the level of cholesterol in the blood, and do an ECG.
Treatment of coronary heart disease
There are three main methods of treating IHD.
- Drug treatment, which may include taking antihypertensive drugs, antiplatelet agents, statins, beta blockers, ACE inhibitors, nitrates and other drugs.
- Stenting is the dilation of blood vessels by installing stents (thin metal tubes) into them. The procedure is carried out under the control of coronary angiography.
- Coronary bypass surgery is a surgical operation that is performed in case of severe damage to the coronary arteries and a large number of atherosclerotic plaques. During the operation, new pathways are formed for blood movement to bypass the narrowing sites. Shunts are created from the patient's own arteries. Coronary bypass surgery not only restores blood supply to the heart, but also eliminates the risk of re-development of coronary artery disease.
Also, a mandatory element of treatment is lifestyle changes (giving up bad habits, following a diet, dosed physical activity).
Diagnostics
The doctor will ask you some questions, perform an examination, and take standard laboratory tests. You may then be referred to additional research methods:
Electrocardiogram (ECG).
An electrocardiogram records the electrical impulses of your heart. An ECG can provide information about both a previous myocardial infarction and one that is currently occurring. In some cases, Holter monitoring may be performed. This is a type of ECG that is recorded by a portable sensor for 24 hours while performing normal activities. Some signs indicate reduced blood flow to the heart.
Echocardiogram.
This test uses sound waves to create an image of your heart. While recording an echocardiogram, it is possible to determine the structure of the heart and its contractility. Areas that move more slowly may have been affected during the infarction. So you can suspect IHD.
Stress test.
If your symptoms occur primarily during exercise, your doctor may order an ECG while walking on a treadmill, known as a stress test. In some cases, drug stimulation of the heart is used instead of physical activity.
Some stress tests are performed while the echocardiogram is being recorded. For example, your doctor may give you an ultrasound before and after exercise. Or drug stimulation is possible during ECHO recording.
Another stress test, known as a nuclear stress test, helps measure blood flow in the heart muscle during rest and exercise. This test is very similar to a standard stress test, but in addition to the ECG, the doctor receives images of the heart. Microscopic doses of radioactive materials such as thallium or a drug known as “cardiolite” are injected into your blood, and special sensors detect areas of reduced blood flow in the heart.
Cardiac catheterization or coronary angiography.
You are injected with a special dye to visualize the heart's blood flow. The dye is injected into the heart arteries using a long, thin, soft tube (catheter), usually passed through an artery in the thigh to the arteries of the heart. This procedure is called cardiac catheterization. The dye shows areas of narrowing and blocks in the arteries on X-rays. If you have a block that requires treatment, a balloon may be inserted and inflated into the blockage to improve blood flow. To fix the lumen of the artery in this position, it is possible to install a stent (mesh metal tube).
CT scan.
A CT scan can help your doctor visualize the coronary arteries. CT scan shows calcification within fatty deposits that narrow the coronary arteries. IHD is characterized by significant calcium deposition in the coronary arteries. CT angiography also uses a contrast agent to help create images of the coronary arteries.
Magnetic resonance angiography (MRA).
This test combines MRI technology with the injection of a contrast agent to identify areas of narrowing or blockage in the coronary arteries. However, some details may not be as clear as with coronary angiography.
Prevention measures
Measures to prevent IHD include:
- proper nutrition. Avoid consuming saturated fats, which increase cholesterol levels. The diet should include as many polyunsaturated fatty acids as possible, which have an antiatherogenic effect and prevent the development of cardiovascular diseases. Useful foods for the cardiovascular system - ocean fish, seafood, vegetable oils (sesame, olive, rapeseed);
- active lifestyle. Physical activity improves blood circulation, normalizes blood pressure, and prevents weight gain;
- blood pressure control;
- giving up alcohol and smoking;
Also, do not forget about timely diagnosis. to visit a cardiologist not when pain in the heart appears, but regularly (once a year). This is especially important if you are at risk of developing coronary heart disease.
Prevalence of the disease
In Russia, about 5.1-5.3% of the population suffers from ischemic heart disease.
At the same time, coronary heart disease remains the main cause of mortality and disability in the population. Worldwide, deaths from pathologies of the cardiovascular system account for a third of diagnosed cases. In Russia, this figure is higher and amounts to 57%, of which 29% are deaths due to myocardial ischemia. Myocardial ischemia mainly affects people over 40 years of age. In young and middle age, coronary heart disease is more often detected in men; with increasing age, the ratio of cases evens out.
Lifestyle and Home Remedies
Lifestyle changes will help you prevent or slow down the development of CHD.
Quit smoking.
Smoking is one of the most important risk factors for the development of coronary artery disease. Nicotine constricts blood vessels and increases heart function. Carbon monoxide reduces the amount of oxygen in the blood and damages the lining of the arteries. Quitting smoking is one of the best ways to reduce your risk of developing CHD.
Blood pressure control.
Ask your doctor to monitor your blood pressure at least every 2 years. You may be advised to check your blood pressure more frequently if your blood pressure readings are higher than normal or if you have a history of heart disease. Ideal blood pressure is below 120 systolic and 80 diastolic measured in millimeters. mercury column.
Controlling cholesterol levels.
Check your cholesterol levels at least every 5 years. Your doctor may recommend testing more frequently if your cholesterol levels become elevated. Low-density lipoprotein levels should be below 130 mg/dL or 3.4 mmol/L. If you have other risk factors for developing coronary artery disease, you should keep your cholesterol level to no more than 100 mg/dL (2.6 mmol/L).
Control of diabetes mellitus.
Maintaining blood glucose concentrations at normal levels reduces the risk of coronary artery disease.
Physical activity.
Physical exercise will help you achieve and maintain a healthy body weight, control diabetes, cholesterol levels, and blood pressure - the main risk factors for developing coronary artery disease. If your doctor approves, exercise for 30 to 60 minutes every day.
Eat healthy.
Heart-healthy foods including fruits, vegetables, and whole grains—low in saturated fat, cholesterol, and salt—will help control weight, blood pressure, and cholesterol levels. It is preferable to eat fish dishes once or twice a week.
Stress control.
Limit stress as much as possible. Practice stress management techniques such as muscle relaxation and deep breathing.
In addition to making lifestyle changes, remember the importance of regular medical checkups. Most risk factors, such as cholesterol, high blood pressure and diabetes, have no symptoms in the early stages. Early diagnosis and treatment can set the stage for heart health.
Also ask your doctor about regular flu vaccinations. IHD and other cardiovascular diseases increase the risk of developing complications of influenza.
Alternative Treatment
Omega-3 fatty acids are a type of unsaturated fatty acid that has anti-inflammatory effects.
Fish and fish oil are the richest sources of omega 3 fatty acids. Fatty fish such as salmon, herring and, to a lesser extent, tuna are rich in omega-3 fatty acids. Adding fish oil to food also brings benefits, but to a lesser extent than eating fish itself.
Flax and flaxseed oil also contain high amounts of omega-3 fatty acids, but various studies have not found this source to be as effective as eating fish.
Other sources of omega-3 fatty acids: Walnuts, canola oil, soybeans, soybean oil. These foods contain lower amounts of omega-3 fatty acids than fish, and their effect is less pronounced.
Other supplements to help lower blood pressure and cholesterol:
- alpha-linolenic acid;
- artichokes;
- barley;
- beta-sitosterol (found in dietary supplements and some margarines);
- white plantain, psyllium;
- cocoa;
- coenzyme Q 10;
- garlic;
- oat bran;
- sitostanol (found in dietary supplements and some margarines);
Prognosis and care
Coronary heart disease is a progressive disease with a rapid transition to the chronic phase and a conditionally unfavorable prognosis. High-quality treatment can slow down the development of pathology, but not completely stop it.
If a heart attack develops as a result of coronary artery disease, a person requires serious treatment and long-term recovery. With severe damage, patients may experience anxiety-depressive reactions and changes in behavior. General weakness, fatigue, and excitability cannot be ruled out. In these conditions, you should strictly, on time, follow the doctor’s instructions, follow the regimen and diet. Working relatives do not always have the opportunity to provide proper help and care. For this, people turn to special medical institutions.
A good example is the private boarding house “Idyll” in Yekaterinburg. Here, guests live in comfortable rooms under the 24-hour supervision of qualified doctors and medical staff. Each type of disease has its own rehabilitation program. Sick people receive full care, including the help of a psychologist. They can walk and spend pleasant leisure time.