Bypass grafting of the arteries of the lower extremities below the inguinal ligament are:
- femoral-popliteal bypass surgery,
- femoral-tibial bypass,
- femoral-distal popliteal bypass.
Above the inguinal ligament the following is performed:
- aortofemoral bypass surgery,
- aorto-bifemoral bypass (aorto-femoral bifurcation bypass),
- aorto-iliac bypass surgery,
- iliofemoral bypass,
- femoro-femoral cross bypass,
- aorto-mesenteric bypass, depending on which vessel needs bypass.
Read more about types of aortic bypass surgery
Aortofemoral bypass surgery, femoral-popliteal bypass surgery, femoro-tibial bypass surgery and other types of bypass surgery create new pathways for delivering blood to tissues, bypassing diseased arteries. Arterial bypass surgery does not cure artery disease. This type of treatment (surgery) is used when drug therapy and minimally invasive procedures (balloon angioplasty of arteries, arterial stenting) do not relieve the existing symptoms of the disease.
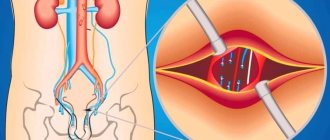
Aortofemoral bypass surgery (aortobifemoral bypass surgery)
This is the implementation of a shunt connecting the aorta to the femoral arteries, which bypasses the diseased arteries and increases blood flow to the patient's legs.
Access to the aorta is achieved either by a midline laparotomy or by a Robe oblique transverse incision. The femoral arteries are accessed through a vertical incision in both groin areas. Using thin threads, the shunt is sutured above and below the blocked arteries. Then the tissue is sutured layer by layer over the shunt.
Subclavian-femoral / axillary-femoral / axillary-bifemoral bypass
This type of bypass is used in some difficult situations.
Instead of the aorta as the source of blood, the subclavian or axillary artery is used. An incision is made below the collarbone and in one or two groin areas. The shunt is sutured with thin threads to the subclavian or axillary artery and femoral artery(s). Pain in the area of postoperative sutures can be observed for several days.
The operation time varies widely, depending on the person’s weight, scar tissue changes, and the severity of the disease.
Methods and techniques of execution
Bypass surgery is a abdominal operation that involves the formation of an additional blood flow path to the heart, bypassing the affected segments of the coronary arteries. They operate both planned and emergency. There are two methods of creating anastomoses in cardiac surgery: mammarocoronary (MCB) and aortocoronary (CABG). In the aortocoronary route, the great saphenous vein of the thigh or vein of the leg is used as a replacement substrate, and in the case of MCS, the internal thoracic artery is used.
Sequencing
- The heart is accessed (usually through an incision in the sternum).
- Simultaneous collection of grafts with sternotomy (removal of a vessel from another part of the body).
- Cannulation of the ascending aorta and vena cava, connection of the artificial blood circulation machine (CAB) (consists of pumping through a special device - a membrane oxygenator, which saturates the venous blood with oxygen, while allowing it to bypass the aorta).
- Cardioplegia (cardiac arrest by cooling).
- Application of shunts (suturing of blood vessels).
- Prevention of air embolism.
- Restoration of cardiac activity.
- Suturing the incision and draining the pericardial cavity.
Then the functioning of the anastomosis is checked using special techniques. Sometimes a minimally invasive operation is performed without connecting the AIK. It is performed on a beating heart and has a lower risk of complications and a shorter recovery time. However, this type of intervention requires extremely high qualifications of the surgeon.
For more information about the technique of performing CABG, watch the video in the block below.
Stenting or bypass surgery, which is better?
Stenting is a minimally invasive method for the treatment of obliterating vascular atherosclerosis. If patients apply in a timely manner and the disease is not advanced, performing such a procedure has an advantage.
If the situation does not allow stenting (blockage of vessels over a long distance, impossibility of passing a stent through a blocked vessel), then bypass surgery is performed. There are situations that require a hybrid approach in the treatment of atherosclerosis of the arteries of the lower extremities. For example, narrowing of the iliac artery and blockage of the femoral artery. In this case, stenting of the iliac artery and femoropopliteal bypass is performed.
In the postoperative period, the patient of our department remains under the supervision of the attending physician in superior wards for 5-7 days, where dressings and care of postoperative wounds are performed.
I often ask what disability group is given after bypass surgery. The issue of disability is resolved at the MSEC at the place of residence.
For what diseases is bypass surgery performed?
The presence of cholesterol plaques in blood vessels (atherosclerosis). In a healthy person, the walls of blood vessels and arteries are a smooth surface without any obstructions or narrowings. In a person suffering from atherosclerosis, blockage of blood vessels occurs due to cholesterol plaques. If the disease is neglected, it can lead to the death of tissues and organs.
Cardiac ischemia. The traditional case of bypass surgery is coronary (coronary) heart disease, in which the coronary arteries supplying the heart are affected by cholesterol deposits in the vessel. The main symptom of this disease is narrowing of the lumen of blood vessels, which leads to insufficient oxygen supply to the heart muscle. In such a situation, complaints often arise of pain behind the sternum or in the left half of the chest, the so-called angina pectoris or angina pectoris.
Having excess weight. A shunt inserted into the stomach divides it into large and small. The small intestine connects to the small intestine, causing the volume of food eaten and the absorption of nutrients to be significantly reduced.
Article on the topic
Rules of life after coronary artery bypass surgery
Impaired blood flow in the vessels of the brain . Insufficient blood supply to the brain (ischemia) can be either limited or global. Ischemia impairs the brain's ability to function normally and, if left untreated, can lead to tumors or brain infarction. Treatment of cerebral ischemia is carried out by a neurologist in a hospital with the help of medications (vasodilators, drugs against the formation of blood clots and to thin the blood, nootropic drugs to improve brain function) or through surgery (in the later stages of the disease).
Reviews from patients after bypass surgery
There are a large number of methods for restoring blood circulation in the heart muscle: stenting, ballooning and others. Bypass surgery is the most radical possible technique, allowing you to resume oxygen supply by replacing the vessel. Patients who undergo such an intervention always feel an improvement in their condition. It is associated with the complete disappearance of symptoms, increased exercise tolerance and quality of life. We never recommend refusing to carry out this procedure in cases where there are reasoned indications for it, because only in this way does the patient have a chance of recovery.
Prediction of how long you can live after surgery
If blood flow in the coronary arteries is completely restored after coronary bypass surgery and the patient takes all prescribed therapy, then the prognosis is considered favorable.
Restoring adequate blood supply to the myocardium can relieve the patient from pain associated with myocardial ischemia, reduce the number of angina attacks, and improve exercise tolerance.
Long-term results of surgical intervention:
- restoration of working capacity;
- reducing the risk of developing myocardial infarction;
- reducing the risk of sudden death from acute coronary syndrome;
- improving exercise tolerance;
- increase in life expectancy;
- medications are taken only for prophylactic purposes.
How long do you live after heart bypass surgery?
The average lifespan of a shunt is 10 years. To assess the viability of the shunt, coronary angiography is performed, based on the results of which a decision is made on the need for repeated surgical treatment. A full course of rehabilitation after cardiac surgery allows you to maximize the service life of the installed shunt.
Reviews from patients who have undergone bypass surgery are mostly positive. After the operation, the heart undergoes remodeling; during this period, patients note a deterioration in their health, and it seems to them that the operation was unsuccessful. However, after a while, after a complete restructuring of the blood supply to the myocardium, the patients’ well-being significantly improves, exercise tolerance increases, and chest pain goes away. In the long term, reviews are mostly positive.
A gentle surgical option to restore adequate blood supply to the myocardium is cardiac stenting. The essence of the operation is to insert a special stent into the coronary vessel, which, after deployment, completely opens the lumen of the affected artery and restores blood flow. The rehabilitation period after stenting surgery is much shorter than with bypass surgery, because The intervention is not performed on an open heart, but a stent is inserted through the groin or through the arm.
Rehabilitation
Recovery after surgery is a set of measures aimed at returning to everyday life, adequate physical activity and professional activities.
The entire period is divided into several stages:
- The stationary period is aimed at expanding the motor regime. The patient is allowed to sit down, then stand, walk around the ward, etc., increasing the load on the heart every day under the strict supervision of the staff.
- Long-term observation. After discharge from the cardiology center, recovery after cardiac bypass surgery continues at home. The patient is usually on sick leave to avoid overload and colds. You can return to work no earlier than six weeks after discharge (the period is determined individually). For a driver or builder, it is usually extended to another three months. The patient should visit the local doctor and cardiologist 3, 6 and 12 months after the intervention. During each visit, he undergoes an ECG, determines the biochemical spectrum of lipids, a general blood test, and, if necessary, a chest x-ray. The main principle of the rehabilitation process at this stage is lifestyle modification. The concept implies adequate sleep (at least 7 hours), frequent split meals with the obligatory inclusion of polyunsaturated fatty acids in the diet, quitting smoking and alcohol abuse, sufficient physical activity, maintaining normal body weight (waist circumference in women <80 cm, in men < 94 cm). Despite the significant improvement in well-being and the disappearance of chest pain, the patient needs to adhere to the constant intake of certain medications. These include blood thinners, cholesterol lowerers, and antihypertensives.
- Sanatorium-resort. Patients are recommended to undergo a rehabilitation course in a specialized institution. A comprehensive program usually includes cardio training, exercise therapy and physical therapy.
Restoring vascular patency using CABG, as a rule, significantly improves the quality of life of patients: angina attacks disappear, the likelihood of a heart attack after bypass surgery decreases, and ability to work is restored. The need for medications is reduced to a preventive minimum. However, it is worth noting that the risk of repeated thrombosis exists, and only if you follow lifestyle recommendations will you be able to maintain your health for a long time.
2.Preparation for bypass surgery
Before undergoing brain bypass surgery, it is necessary to conduct a medical examination and some standard tests: ECG, general and clinical blood and urine tests, fluorography. Special examinations before brain bypass surgery include the following:
- MR, CT or intra-arterial angiography;
- Balloon examination of arterial occlusion;
- Dopplerography of cerebral arteries.
2 weeks before surgery, the patient should not smoke, drink or take drugs. It is also necessary to stop taking non-steroidal anti-inflammatory drugs.
Visit our Neurosurgery page
Patients and methods
We observed 104 patients aged 16 to 52 years (48 women, 56 men) with unilateral non-purulent forms of otitis media, which were caused by persistent DST and combined with deformation of the nasal septum and chronic hypertrophic rhinitis. Exclusion criteria from the study were bilateral lesions of the middle ear, adenoid vegetations, neoplasms of the nasal cavity and nasopharynx, inflammation of the SNP, cicatricial adhesions (stenoses) in the area of the nasopharyngeal anastomosis S.T. All patients underwent examination and treatment in the otorhinolaryngology department of the State Budgetary Healthcare Institution of the Moscow Scientific and Practical Center of Otorhinolaryngology named after. L.I. Sverzhevsky DZM. The examination of patients was dynamic in nature, carried out every 15 days and included the collection of complaints and anamnesis of the disease; examination of ENT organs, X-ray examination of the SNP and temporal bones; endoscopic examination of the nasal cavity, nasopharynx and anterior active rhinomanometry (APRM); otomicroscopy, tuning fork hearing testing, pure tone threshold audiometry (TPA) and impedance measurement. To objectively assess the functional state of the TM, a computer analyzer of the middle ear AT 235 h (Interacustics, Denmark) was used in two modes: ETF1 - Williams test for non-perforated PD, ETF2 - Toynbee test - in the presence of perforation of TM. The observation period for patients was 1 year. All digital material was subjected to statistical processing, which was performed using computer programs Statistica Data Miner, StatSoft Inc.
Surgical treatment included BP shunting, septoplasty with splinting of the nasal septum according to the method of A.I. Kryukova et al. and lower sparing conchotomy [8]. Postoperative hemostasis was performed using original sectional hydrotampons, which were removed 24 hours after surgery [9]. Conservative treatment of DST began immediately after myringotomy. Transudate (if present) was removed, a shunt was installed, and drugs with anti-inflammatory and proteolytic effects were administered transtympanically. In the early stages after surgery, the nasal cavity was toileted with targeted anemization of the mucous membrane of the mouth of the auditory tube (on the side of the affected ear). The patient also used decongestants on his own. From the 3rd day of treatment, CT catheterization was performed. From the 10th to the 15th day after surgery - electrical stimulation of the CT according to the method of R.G. Antonyan [10]. Next, the patient independently carried out CT ventilation.
Complications
Complications after bypass surgery can occur during surgery and after discharge. As stated above, the risk of adverse effects is assessed before intervention and depends on the background condition of the body. The most common problems include:
- acute renal failure;
- thrombosis;
- cardiac arrest;
- rhythm disturbances;
- myocardial infarction;
- infection, including sepsis;
- pneumonia;
- bleeding;
- pericarditis and cardiac tamponade;
- pulmonary edema;
- cardiogenic shock;
- neurosis.
A long-term complication is stenosis of the shunts due to non-compliance with the doctor’s recommendations. In this case, the patency of the vessels becomes more difficult again, and a typical clinical picture of angina occurs. This situation requires repeated coronary artery bypass grafting.