Table of contents
- Etiology and pathogenesis
- Clinical manifestations
- Treatment methods
“Veins in the legs” (varicose veins, varicose veins, varicose veins, “spider veins”) are an external manifestation of chronic venous insufficiency, which is associated with a violation of the reverse flow of blood from the extremities to the heart. Mild forms of this pathology (“spider veins” or venous telangiectasias) cause cosmetic defects and can cause physical or psychological discomfort to patients, while severe forms can lead to serious complications, including the formation of ulcers, necrosis and malnutrition of the limb.
In our company you can purchase the following equipment for removing spider veins on the legs:
- M22 (Lumenis)
Clinical signs of varicose veins in the form of “spider veins” or so-called “leg veins” occur more often in women. This is due to hormonal characteristics, and this dependence can be traced in any age group.
As for statistics, in the United States, varicose veins in one form or another are recorded in 23% of the adult population, and if we take into account mild forms of the disease (what patients usually call “leg veins”), the figure increases to 80% in men and 85% among women .
Varicose veins in men
Treatment of varicose veins should be comprehensive: the treatment plan is selected by the doctor. It is advisable to adjust your lifestyle. The following are useful for healthy veins: − therapeutic exercises;
− walking;
− swimming;
− skiing;
− cycling.
To help blood flow more actively through the veins, massage of the buttocks, thighs, legs, and feet is useful. This should be light stroking and shaking of the muscles (from the buttocks to the feet), without affecting the areas of the dilated veins themselves. The duration of the procedure is 5–10 minutes daily [1].
An important place in treatment is given to special drugs that improve the tone of the veins - venotonics.
Venotonics are local and systemic
For example, local, or external, includes Detragel®. It contains three components that, thanks to an innovative delivery system, quickly penetrate the skin and help fight heaviness and swelling in the legs [5]. Detragel® does not leave a sticky feeling or marks on clothing and skin [6,7].
As a rule, local agents are recommended to be used together with systemic venotonics (those taken orally, in tablets), such as Detralex®. It works at any stage of varicose veins, acts on the cause of varicose veins from the inside and helps cope with pain and swelling in the legs. The drug is convenient to use: only 1 tablet of 1000 mg per day [8].
Varicose veins are a non-gender disease. It must be treated as soon as possible, starting from the first signs of the disease. Approaches involve lifestyle changes, wearing special compression stockings (there are comfortable knee socks for men) and the use of medications prescribed by a doctor.
* The only combination of heparin, phospholipids and escin registered in the Russian Federation according to GRLS, September 2019
1. Tamozhanskaya A.V., Koval M.V. Comprehensive physical rehabilitation of patients with varicose veins of the lower extremities at the outpatient stage // Slobozhansky scientific and sports bulletin, 2012. No. 2. pp. 125-128.
2. Seliverstov E.I., Avakyants I.P., Nikishkov A.S., Zolotukhin I.A. Epidemiology of chronic venous diseases // Phlebology, 2021. No. 1. P. 35-43.
3. The Relationship Between Varicose Veins and Alcohol Consumption. West Florida Vein Center, 11.2014. URL:. https://www.westfloridaveincenter.com/2014/11/relationship-varicose-veins-alcohol-consumption/ ( accessed 12/04/19 )
4. Russian clinical guidelines for the diagnosis and treatment of chronic venous diseases 2021. URL: https://phlebology-sro.ru/upload/iblock/23d/rossiyskie-klinicheskie-rekomendatsii-po-khzv-2018.pdf (access date 04.12. 19)
5. Instructions for medical use of the drug Detragel®.RU.: LP-001044.
6. V.Yu. Bogachev et al. “Modern transdermal phlebotropic therapy. Detragel is in focus." RMJ, 2021 No. 6 (11), 61-65
7. Bogachev V. Yu., Boldin B. V., Turkin P. Yu., Lobanov V. N. Local drugs in the treatment and reduction of the incidence of adverse reactions after sclerotherapy of reticular veins and telangiectasis. Angiology and vascular surgery. 2021. 25(4):102-7
8. Instructions for medical use of the drug Detralex®. RU No. LP-003635.
Etiology and pathogenesis
There are a large number of factors that contribute to the appearance of clinical symptoms of chronic venous insufficiency. In most cases, it occurs due to increased pressure in the superficial veins .
Some people have congenital weakness of the venous walls , but the pressure in the vessels may be normal.
An important role is played by weakness of the valvular apparatus of the veins , and it has been proven that this factor is inherited. The specific genes responsible for valve failure have not yet been identified. It was noted that in female relatives the probability of dilated veins appearing in the legs (if parents have this pathology) is 43%, while in male relatives it is only 19%.
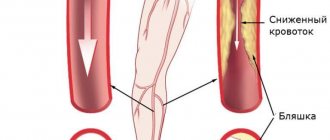
Prolonged standing on your feet causes an increase in hydrostatic pressure in the vessels, which contributes to both chronic varicose veins and valvular insufficiency. If the function of the proximal valves is impaired, excess pressure spreads from the deep veins to the superficial ( Fig. 1 ) - this condition progresses rapidly, becoming irreversible. Women are especially susceptible to this type of vascular pathology, since their venous walls and valves periodically become more distensible under the influence of cyclical increases in progesterone levels.
Rice. 1. Schematic representation of the superficial veins ( spider veins ) and their connection with the reticular veins and deeper feeding veins ( feeder veins )
A fairly common cause of visible vein patterns on the legs is pregnancy . Under the influence of hormonal changes, the distensibility of vascular walls and valves increases. At the end of pregnancy, the enlarged uterus compresses the inferior vena cava, exacerbating venous hypertension and secondary distension of the veins of the lower extremities.
Depending on the contribution of each of these mechanisms to the pathogenesis of varicose veins, the clinical manifestations of leg veins may spontaneously regress after childbirth, or may persist in the future.
1.2. Anatomy of the veins of the lower extremities
The first attempt to create a classification of the superficial venous network of the lower extremities in our country belongs to the famous domestic anatomist V. N. Shevkunenko (1949). He believed that the reduction of the primary venous network that occurs during embryogenesis leads to the emergence of main subcutaneous trunks. In accordance with this, he divided all possible structural options into three types: a) the type of incomplete reduction; b) extreme reduction type and c) intermediate type (Fig. 1.3)
Rice. 1.3.
Types of variability of the superficial veins of the lower extremities [Shevkunenko V.N., 1949]. a — type of incomplete reduction; b — type of extreme reduction; c - intermediate type
If in the superficial venous system, mainly on the lower leg, the intermediate type of vein structure dominates, then for the deep veins the main form is most common, which is the result of an extreme degree of reduction of the primary venous network. In this form, the deep veins are represented by two equal trunks with a small number of anastomoses between them. In the scattered form, the veins of the lower leg are multi-trunked, with a large number of anastomoses. The intermediate form occupies a middle position. All three types of structure of the superficial venous system of the lower extremities (main, diffuse and intermediate) have been studied in sufficient detail and do not cause significant controversy. Much more disagreement exists in the description of the structural features of the deep veins at various levels of the lower limb, especially their relationship with each other. The sources of the inferior vena cava are the veins of the foot, where they form two networks - the cutaneous venous plantar network and the cutaneous venous network of the dorsum of the foot. The common dorsal digital veins, which are part of the cutaneous venous network of the dorsum of the foot, anastomose with each other, form the cutaneous dorsal venous arch of the foot. The ends of this arch continue proximally in the form of two longitudinal venous trunks: the lateral marginal vein (v. marginalis lateralis) and the medial vein (v. marginalis medialis). The continuation of these veins on the lower leg are, respectively, the small and large saphenous veins.
On the plantar surface of the foot, a subcutaneous venous plantar arch is distinguished, which widely anastomoses with the marginal veins and sends intercapitate veins into each interdigital space, which anastomose with the veins forming the dorsal arch. The deep venous system of the foot is formed from paired companion veins accompanying the arteries. These veins form two deep arches: dorsal and plantar. The superficial and deep arches are connected by numerous anastomoses. From the dorsal deep arch the anterior tibial veins (vv. tidiales anteriores) are formed, from the plantar (vv. tidiales posteriores) - the posterior tibial veins, receiving the peroneal veins (vv. peroneae). Thus, the dorsal veins of the foot pass into the anterior tibial veins, and the plantar medial and lateral veins form the posterior tibial veins.
Venous valves are present only in the largest veins of the foot. Their location and quantity are variable. The superficial venous system of the foot is connected to the deep system by vessels that do not have valves. This fact is of no small importance in clinical practice, since the introduction of various medicinal and contrast agents into the superficial veins of the foot in the distal direction ensures their unhindered entry into the deep venous system of the lower limb. Thanks to this anatomical feature, it is also possible to measure venous pressure in the deep veins of the foot segment by puncture of the superficial vein of the foot. According to a number of authors, there are about 50 such vessels at the level of the foot, of which 15 are located at the level of the sole.
The venous system of the leg is represented by three main deep collectors (anterior, posterior tibial and peroneal) and two superficial - great and small - saphenous veins. Since the main load in the implementation of outflow from the periphery is borne by the posterior tibial veins, into which the peroneal veins drain, it is the nature of their damage that determines the severity of the clinical manifestations of disorders of venous outflow from the distal parts of the limb.
The great saphenous vein of the lower extremity (v. saphena magna), being a continuation of the medial marginal vein (v. marginalis medialis), passes to the lower leg along the anterior edge of the inner malleolus, then passes along the medial edge of the tibia and, bending around the medial condyle of the femur from behind, in the area of the knee joint passes to the inner surface of the thigh.
The small saphenous vein (v. saphena parva) is a continuation of the external marginal vein of the foot (v. marginalis lateralis). Passing behind the lateral malleolus and heading upward, the small saphenous vein is first located along the outer edge of the Achilles tendon, and then lies on its posterior surface, approaching the midline of the posterior surface of the leg. Usually, starting from this area, the vein is represented by one trunk, less often - two. At the border of the middle and lower third of the leg, the small saphenous vein penetrates the thickness of the deep fascia and is located between its layers. Having reached the popliteal fossa, it pierces the deep layer of fascia and flows into the popliteal vein. Less commonly, the small saphenous vein, passing above the popliteal fossa, flows into the femoral vein or tributaries of the deep vein of the thigh, and sometimes ends in some tributary of the great saphenous vein. Often in its terminal section the vein bifurcates and flows into the deep or saphenous veins in separate trunks. In the upper third of the leg, the small saphenous vein forms numerous anastomoses with the system of the great saphenous vein.
The large and small saphenous veins have a large number of deep branches along their length. The deep veins of the leg in its upper third form the popliteal vein, the sources of which are the posterior and anterior tibial veins.
Superficial veins communicate with deep veins through perforating veins or perforators (vv. perforantes). Yu. H. Loder (1803) divided these veins into direct ones, connecting the main trunks of the saphenous veins with the deep ones, and indirect ones, ensuring the connection of the tributaries of the saphenous veins with the deep venous highways. Since that time, terminological confusion has persisted in the literature regarding the veins connecting the superficial and deep venous systems. R. Linton defined direct perforating veins as veins connecting superficial veins with deep ones, and communicating veins as veins connecting superficial veins with muscular ones. Often in literature and practice, the terms “perforators” and “communicators” are considered equivalent and are used arbitrarily. In the domestic literature, it is currently generally accepted to consider the communicant veins flowing into the main trunks of the deep veins to be direct, and the communicant veins connecting the superficial veins with the muscular tributaries of the deep veins to be indirect. The sections of communicating veins at the level of passage (perforation) of the intrinsic fascia of the leg are called perforating. Many authors combine the concepts of perforating and communicating veins into a single group of internal perforating veins. Starting from the surface with one or more tributaries, after merging, the trunk of the vein passes through the fascia, flowing into the deep or muscular vein independently or dividing into branches. In this regard, some authors distinguish, respectively, several forms of communicating veins: simple, complex, atypical, branching and collecting. Other researchers believe that the perforator vein provides directed transfer of blood from the axes of the superficial veins to the deep veins through perforation of the superficial aponeurosis. The communicating vein promotes indifferent diffusion of blood between various axes or sections of the superficial veins into the supraaponeurotic spaces. In this case, the division of these veins follows the main topographic groups - medial, lateral and posterior.
In each lower limb, up to 155 perforators are described, called “permanent” and identified in at least 75% of studies and surgical interventions performed for varicose veins. The connection between the saphenous and deep veins is carried out mainly indirectly, that is, through the muscular veins. The number of direct communicating veins on the lower leg ranges from 3 to 10. There are much more indirect communicating veins than direct ones. Most perforators are located along the axes of the “power” lines. This arrangement meets a functional need. The simplest perforator vein complex is represented by the simple vein of Cockett. It contains: 1) a supraaponeurotic segment, originating in the nearest axis of the superficial vein; 2) a transaponeurotic segment, perforating the superficial aponeurosis through a larger or smaller lumen, which in some cases allows the passage of arterioles and nerve branches together with the vein; 3) a subaponeurotic segment, ending very quickly in the nearest axis of the deep vein; 4) valve apparatus, classically including one or two supraaponeurotic valves, one to three subaponeurotic valves, a mandatory element of which is the presence of an attachment ring corresponding to the thickening of the venous wall.
The diameter of the communicating veins is also variable. According to various sources, normally it ranges from 0.1 to 4 mm. In pathological processes, ectasia of the communicating veins can reach 7-8 mm or more. From the point of view of practical surgery, in our opinion, the classification of the French phlebological school is most acceptable. They divide perforating veins into minimal (1-1.5 mm), medium (2-2.5 mm) and volumetric (3-3.5 mm). The term "megavena" is used for vessels with a diameter of more than 5 mm.
Thanks to recent anatomical, ultrasound and endoscopic studies of the venous system of the lower extremities, it has become possible to clearly recognize venous valves, which have the appearance of a transparent veil and are able to resist the powerful hemodynamic shocks of muscle pumps. The number, location and direction of the leaflets of the valve structures of the veins are also quite variable. The statement that all veins connecting the superficial and deep venous systems have valves that allow blood to pass only into the depths cannot be considered absolutely reliable, since valveless perforating veins have been identified on the foot and leg. The veins of the leg also have valves, the valves of which are oriented towards the superficial veins in some cases and in the opposite direction in others. Functioning passively depending on the direction of blood flow, the valve apparatus of the veins of the lower extremities prevents retrograde discharge of blood, protecting venules and capillaries from sudden pressure drops during the operation of the muscular-venous mechanisms of the foot, leg and thigh. Hence the mutual dependence of the localization and function of the valves.
Significant variability in the structure of the superficial venous network of the lower extremities is aggravated by discrepancies in the names of veins and the presence of a large number of eponyms, especially in the names of perforating veins. To eliminate such discrepancies and create a unified terminology for the veins of the lower extremities, the International Interdisciplinary Consensus on Venous Anatomical Nomenclature was created in 2001 in Rome. According to it, all veins of the lower extremities are conventionally divided into three systems:
- Superficial veins.
- Deep veins.
- Perforating veins.
Superficial veins lie in the space between the skin and the deep (muscular) fascia. The GSV is located in its own fascial sheath, formed by the splitting of the superficial fascia. The trunk of the SVC is also located in its own fascial sheath, the outer wall of which is a superficial layer of muscular fascia. Superficial veins provide the outflow of approximately 10% of the blood from the lower extremities. The deep veins are located in spaces deeper than this muscular fascia. In addition, deep veins always accompany arteries of the same name, which does not happen with superficial veins.
Rice. 1.24.
Superficial veins of the lower extremities
The deep veins provide the main drainage of blood - 90% of all blood from the lower extremities flows through them. Perforating veins perforate the deep fascia, connecting the superficial and deep veins. The term “communicating veins” is reserved for veins that connect certain veins of the same system (i.e., either superficial to each other, or deep to each other).
Main superficial veins:
1.
Great saphenous vein (GSV) - vena saphena magna, in English literature - great saphenous vein (GSV). Its source is the medial marginal vein of the foot. It goes up the medial surface of the leg and then the thigh. Drained into the BV at the level of the inguinal fold. Has 10-15 valves. The superficial fascia splits into two layers, forming a canal for the GSV and cutaneous nerves. On the thigh, the trunk of the GSV and its large tributaries in relation to the fascia can take three main types of mutual arrangement: - i-type, in which the trunk of the GSV lies entirely subfascially from the SPS to the knee joint; - h-type, in which the trunk of the GSV accompanies a large tributary located suprafascially. At a certain point it pierces the fascia and flows into the GSV. Distal to this location, the trunk of the GSV is usually much smaller in diameter than its tributary; - s-type, extreme degree of h-type, while the trunk of the GSV distal to the confluence of the tributary is aplastic. In this case, it seems that the trunk of the GSV at some point abruptly changes direction, perforating the fascia. The existing fascial canal is considered by many authors as a protective outer “cover” that protects the GSV trunk from excessive stretching when the pressure in it increases.
2.
The most constant tributaries:
2.1
. Intersaphenous vein(s) [vena(e)) intersaphena(e)], in English literature - intersaphenous vein(s) - runs (run) along the medial surface of the leg. Connects the GSV and SSV. Often has connections with perforating veins of the medial surface of the leg.
2.2
. Posterior thigh circumflex vein (vena circumflexa femoris posterior), in English literature - pos terior thigh circumflex vein. It may have its source in the SVC, as well as the lateral venous system. It rises from the back of the thigh, wraps around it, and drains into the GSV.
2.3
. Anterior surrounding thigh vein (vena circumflexa femoris anterior), in English literature - anteri or thigh circumflex vein. May have its source in the lateral venous system. It rises along the anterior surface of the thigh, going around it, and drains into the GSV.
2.4
. Posterior accessory great saphenous vein (vena saphena magna accessoria posterior), in English literature - posterior accessory great saphenous vein (the segment of this vein on the lower leg is called the posterior arched vein or vein of Leonardo). This is the name of any venous segment on the thigh and lower leg, running parallel and posterior to the GSV.
2.5.
Anterior accessory great saphenous vein (vena saphena magna accessoria anterior), in English literature - anterior accessory great saphenous vein. This is the name of any venous segment on the thigh and lower leg, running parallel and anterior to the GSV.
2.6.
Superficial accessory great saphenous vein (vena saphena magna accessoria superficialis), in English literature - superficial accessory great saphenous vein. This is the name of any venous segment on the thigh and lower leg, running parallel to the GSV and more superficial relative to its fascial sheath.
3.
Small saphenous vein (vena saphena parva), in English literature - small saphenous vein. It has its source in the external marginal vein of the foot. It rises along the back surface of the leg and flows into the popliteal vein, most often at the level of the popliteal fold. Receives the following tributaries:
3.1.
Superficial accessory small saphenous vein (vena saphena parva accessoria superficialis), in English literature - superficial accessory small saphenous vein. It runs parallel to the trunk of the SVC above the superficial layer of its fascial sheath. It often drains independently into the popliteal vein.
3.2.
Cranial extension of the small saphenous vein (extensio cranialis venae saphenae parvae), in English literature cranial extension of the small saphenous vein. Previously called the femoropopliteal vein (v. femoropoplitea). It is a rudiment of an embryonic intervenous anastomosis. When there is an anastomosis between this vein and the posterior circumferential femoral vein from the GSV system, it is called the vein of Giacomini.
4.
Lateral venous system (systema venosa lateralis membri inferioris), in English literature - lateral ve nous system. Located on the anterior and lateral surface of the thigh and lower leg. It is assumed that it is a rudiment of the lateral marginal vein system that existed in the embryonic period.
5.
Inguinal venous plexus (confluens venosus subin guinalis), in English literature - confluence of su perficial inguinal veins. It is the terminal section of the GSV near the anastomosis with the BV. Here, in addition to the last three tributaries listed, three fairly constant tributaries flow into: the superficial epigastric vein (v. epigastrica superficialis), the external pudendal vein (v. pu denda externa) and the superficial vein surrounding the ilium (v. circumflexa ilei superficialis). In the English-language literature there is a long-established term Crosse, denoting this anatomical segment of the GSV with the listed tributaries.
Rice. 1.5.
Perforating veins of the lateral and posterior surfaces of the lower extremities
Rice. 1.6.
Perforating veins of the anterior and medial surfaces of the lower extremities
There is no doubt that only the main clinically significant venous collectors are listed and have proper names. Considering the high diversity of the structure of the superficial venous network, other superficial veins not included here should be named by their anatomical location. The deep veins, as already indicated, are located deeper than the muscular fascia and often accompany the arteries of the same name.
Perforating veins are one of the most numerous and diverse venous systems in shape and structure. In clinical practice, they are often called by the names of the authors involved in their description. This is not only inconvenient and difficult to remember, but sometimes it is not entirely historically correct. Therefore, in the above international consensus it is proposed to name perforating veins according to their anatomical location.
Thus, all perforating veins of the lower extremities should be divided into 6 groups, which are divided into subgroups:
1.
Perforating veins of the foot
1.1. Dorsal perforating veins of the foot
1.2. Medial perforating veins of the foot
1.3. Lateral perforating veins of the foot
1.4. Plantar perforating veins of the foot
2.
Perforating veins of the ankle
2.1. Medial perforating veins of the ankle
2.2. Anterior perforating veins of the ankle
2.3. Lateral perforating veins of the ankle
3.
Perforating veins of the leg
3.1. Medial perforating veins of the leg
3.1.1. Paratibial perforating veins
3.1.2. Posterior tibial perforating veins
3.2. Anterior perforating veins of the leg
3.3. Lateral perforating veins of the leg
3.4. Posterior perforating veins of the leg
3.4.1. Medial gastrocnemius perforating veins
3.4.2. Lateral gastrocnemius perforating veins
3.4.3. Intercapital perforating veins
3.4.4. Paraachillary perforating veins
4.
Perforating veins of the knee joint
4.1. Medial perforating veins of the knee joint
4.2. Suprapatellar perforating veins
4.3. Perforating veins of the lateral surface of the knee joint
4.4. Subpatellar perforating veins
4.5. Perforating veins of the popliteal fossa
5.
Perforating veins of the thigh
5.1. Medial perforating veins of the thigh
5.1.1. Perforating veins of the adductor canal
5.1.2. Perforating veins of the groin area
5.2. Perforating veins of the anterior thigh
5.3. Perforating veins of the lateral thigh
5.4. Perforating veins of the posterior thigh
5.4.1. Perforating veins of the posteromedial thigh
5.4.2. Sciatic perforating veins
5.4.3. Perforating veins of the posterolateral thigh
5.5. Pudendal perforating veins
6.
Perforating veins of the buttocks
6.1.
Superior gluteal perforating veins
6.2.
Middle gluteal perforating veins
6.3.
Inferior gluteal perforating veins
Clinical manifestations
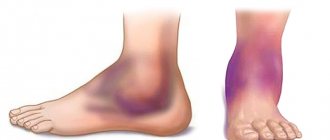
The manifestation of chronic venous insufficiency is extremely diverse - it varies from small “spider veins” to large protrusions of large veins above the surface of the skin, with ulcerations and necrotic changes.
In the context of this article, we will describe only mild varicose veins, also called “spider veins” or, in other words, telangiectasia. They can form various patterns on their legs: tree-like (branching), arachnid (star-shaped), linear (simple), spotted (pantiform) ( Fig. 2 ).
Rice. 2. Typical localization of superficially dilated veins on the thigh of a 42-year-old woman
In the absence of timely treatment, veins appearing through the skin in the legs can increase in size, occupying an increasingly larger area. In the future, damage to larger and deeper vessels may occur with the formation of corresponding clinical symptoms and complications.
Treatment methods
Patients with spider veins turn to specialists mainly with complaints about an aesthetic defect. The choice of treatment method should begin with a thorough assessment of the patient's condition, which includes examination of pathologically altered veins, medical history, examination of family history and the patient's expectations regarding future therapy. Based on a comprehensive assessment, it should be determined whether a particular method can solve the patient's problem.
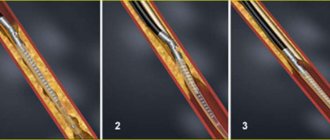
Sclerotherapy is one of the most commonly used medical procedures to treat varicose veins. A sclerosing substance is injected into abnormally dilated vessels, causing destruction of the endothelium with subsequent formation of a fibrous cord. The limiting factor is that vessels with a diameter of 4 mm or more can be eliminated in this way.
Laser coagulation is indicated for the treatment of large varicose veins; its effectiveness for telangiectasia remains controversial. A combination of sclerotherapy and laser treatment is possible , when a sclerosing agent is injected into large afferent and efferent vessels, and then the laser coagulates small branches.
The gold standard for the removal of superficial veins with a vessel depth of up to 5 mm is the 1064 nm Nd:YAG laser. Radiation of this wavelength has a maximum penetration depth and is well absorbed by hemoglobin. Regardless of the success of local therapy for local manifestations of chronic venous insufficiency, it is necessary to examine the pressure in the deeper vessels of the lower extremities - if it is elevated, then the corresponding symptoms will return sooner or later. Therefore, the treatment of such patients should be approached comprehensively, starting to solve the problem by eliminating the main pathogenetic factor.
The use of Nd:YAG laser is recommended to be combined with sclerotherapy or surgical removal of deep-lying vessels.
Questions from our users:
- treatment of spider veins on legs
- laser spider vein removal
- spider veins on the face ultrasound treatment
- What is the best way to remove spider veins on the face?