Pelvioperineal reflux (PPR) is a pathological condition characterized by retrograde blood flow from the intrapelvic veins into the superficial veins of the perineum and lower extremities [1–3]. It is registered in 25-62% of patients with pelvic varicose veins (PVD) [4-6]. The clinical manifestation of PPR is varicose transformation of the veins of the external genitalia, perineum, and posteromedial surface of the thighs. Instrumental diagnosis of this pathology is based on the use of radiation research methods, the choice of which is the subject of active debate among researchers [7–9]. Some of them, in addition to ultrasound angioscanning (USAS) of the pelvic veins, consider oophorography and pelvic venography (OGTP) as a mandatory component of the examination of patients with vulvar (VV) and perineal varicose veins (PV) regardless of the presence of symptoms of pelvic venous congestion (PVP) [3 , 9-11]. Other authors [12-14], guided by the principle of reasonable sufficiency, argue that to determine treatment tactics and select a method for eliminating PPR and varicose veins of the perineum and vulva (phlebectomy or scleroobliteration) in patients with VBT without signs of TVP, it is quite sufficient to perform an ultrasound scan of the pelvic and perineal veins .
The purpose of this study is to determine the diagnostic value and feasibility of performing OGTF in patients with VBT, VV and PV.
Briefly about the diagnostic method
Contrast venography (venography, ascending contrast venography or contrast venography) is an x-ray examination of deep or superficial veins using a contrast agent that provides an image of the blood vessel.
Phlebography determines the patency of the deep veins, the presence of blood clots, valve function and allows for a general assessment of the condition of the deep veins. Phlebography can be used when deep vein thrombosis is suspected, but ultrasound diagnostics cannot accurately exclude it. The study allows us to reliably assess the condition of the iliac veins in obese patients, when it is impossible to conduct a detailed ultrasound scan.
Contrast venography is most often used either during endovascular surgery on the deep veins (angioplasty or installation of a vena cava filter). We use retrograde venography to assess the integrity of venous valves when planning surgery for venous outflow reflux after venous thrombosis.
Interpretation of results
All X-rays, MRI or CT images obtained as a result of the examination should be interpreted only by a radiologist. The resulting conclusion is transferred to the patient’s attending physician, who referred him for the venography procedure.
example of the results of CT phlebography of the legs, done for more effective preparation for phlebectomy surgery
In the protocol of venography of the lower extremities with a normal X-ray picture, you can see phrases such as the function of the valvular apparatus of the veins is preserved, the patency of the veins is normal, no filling defects or “breakage” of the contrast were detected. In the case of thrombosis, these changes are present due to complete or partial obstruction of the venous lumen for contrast.
Regarding MRI phlebography of the brain, we can say that the examination protocol is complex, with many nuances that are understandable only to specialists. In the absence of pathological formations, the corresponding phrase is indicated in the conclusion; if present, the location, size and topographic relationship of the pathological formation and healthy tissue are indicated.
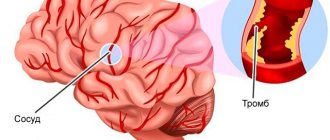
When performing transuterine venography, varicose veins of the small pelvis can be identified, and then their detailed characteristics are also given. The development of thrombophlebitis and phlebothrombosis is also manifested by a break and a defect in contrast filling.
Preparing for diagnosis
- You cannot eat for four hours before the test, and you can only drink water.
- Patients who are allergic (particularly to iodine) or have already had a reaction to contrast should inform their doctor.
- A sedative may be prescribed to calm the patient.
- You may be asked to follow certain dietary restrictions before the test, depending on your specific procedure.
- Tell your doctor about the medications, herbs, or supplements you take. You may be advised to stop taking some of these medications before the test.
How is the diagnosis carried out?
During the procedure, the patient lies on a special X-ray table. The area where the catheter will be inserted is cleared (usually a vein in the arm so that any necessary medications can be administered during the procedure). Sometimes local anesthesia is administered.
A contrast solution is delivered through the catheter. The dye injection causes a warm sensation that can spread throughout the body. The contrast may also cause mild nausea. About 18% of patients experience discomfort from the contrast solution. To fill the deep venous system with dye, a thick tape (or tourniquet) is sometimes placed around the ankle, or the limbs may be angled. The patient is asked to keep his leg still. The doctor watches the movement of the solution through the vein using a fluoroscope. At the same time, a series of photographs are taken.
When the study is completed, saline is injected into the same catheter to clear the veins of contrast, then the catheter is removed and a bandage is applied to the injection site.
Features of phlebography (by location of the veins being examined):
Venography of the lower extremity: the patient is positioned leaning on an inclined X-ray table. The table is tilted so that the legs are raised or lowered. The catheter is inserted into the selected leg or arm. The procedure may take 30 to 45 minutes.
Adrenal venography: the patient lies supine on the X-ray table. The catheter is inserted into the femoral vein. Under the guidance of fluoroscopic visualization, he carefully targets either the renal or suprarenal veins in the abdominal cavity. The procedure takes about 1 hour.
Abdominal venography: the patient lies supine on an x-ray table. The catheter is inserted into the femoral artery. The procedure takes about 1 hour.
Clinical examination
The simplest and most common method for diagnosing pathology of the venous system of the body is a clinical examination of the patient. An examination and interview by a competent specialist (phlebologist, vascular surgeon, angiologist) with sufficient clinical experience will help to suspect and diagnose venous diseases in the early stages of the disease, which will significantly increase the chances of achieving the greatest success in treatment. A clinical examination involves an analysis of the patient’s complaints, a competent history taking and a thorough examination of the patient.
Complaints specific to venous diseases should be considered: pain and heaviness in the calf muscles (dull, aching in nature, more often disturbing in the evening or during prolonged static loads: long stay in the “sitting”, “standing” position); fatigue and numbness of the legs; periodic night cramps.
Objective signs of chronic venous insufficiency should be considered: the appearance of telangiectasia (spider veins, hemangiomas); varicose veins of the saphenous veins; swelling of the lower extremities; trophic skin disorders (the appearance of areas of hyperpigmentation, peeling of the skin on the legs, the appearance of trophic ulcers, varicose eczema, dermatitis)
Unfortunately, clinical examination data alone are often insufficient to determine the nosological variant of venous diseases and determine further treatment tactics. In such cases, numerous instrumental techniques for examining the patient come to the rescue.
After diagnosis
After phlebography, observation in the clinic is necessary for at least 24 hours. Depending on the procedure, you may be advised to rest in bed for a certain period of time.
Patients should drink plenty of fluids to flush any remaining contrast solution from the body. The area where the catheter was inserted may be sore for several days. If you notice swelling, redness, pain, or fever, tell your doctor. In most cases, the patient can resume normal activities the next day.
Precautionary measures
After the contrast agent is removed, an allergy may develop within another half hour, so the patient must be monitored.
During the normal course of the procedure, the superficial veins are evenly filled with a contrast agent without defects. If there are filling defects
, which still remain on repeated images (sharp interruptions in the flow of contrast agent, large veins remain empty), then these are signs of thrombosis.
Tight application of a tourniquet, support on the limb being examined, delay in taking x-ray images, improper administration of a contrast agent, movement of the limb being examined, severe edema, thrombosis, phlegmon of the subcutaneous fat cell, obesity can cause distorted results.
Possible complications
Phlebography can cause complications such as phlebitis, tissue damage, and deep vein thrombosis in the healthy leg. Complications are quite rare, but they must be taken into account when planning treatment so that the risk of the study does not exceed the risk of the disease for which it is being performed.
A rare side effect (up to 1% of cases) is a serious allergic reaction to the contrast dye. It usually appears 30 minutes after the dye injection and requires medical attention.
Possible risks include blood clot formation in the vein, bleeding, damage to blood vessels, or infection at the site where the catheter was inserted.
Some people may experience an allergic reaction to iodine-based contrast dye. This can cause symptoms such as nausea, sneezing, vomiting, hives, and sometimes a life-threatening reaction called anaphylactic shock (especially in older patients with chronic dehydration or mild kidney failure).
Phlebography of the brain
Application
phlebographic visualization of veins and venous sinuses of the brain
Phlebography (venography) of the brain is performed exclusively using an MRI or CT scanner, without the introduction of a radiocontrast agent. This is due to the fact that obtaining a series of targeted images, performed layer by layer, is sufficiently informative even without introducing contrast.
This type of study allows you to confirm or exclude pathology of the venous sinuses, as well as the superficial and deep veins of the brain. This pathology can be caused by various diseases (inflammatory - meningoencephalitis, tumors, brain injuries, diseases of the blood system), but their danger lies in the occurrence of thrombosis of the veins of the specified localization. As a rule, phlebography examines the venous sinuses of the brain, the vein of Galen, and the internal veins of the brain.
Preparation for the procedure
No special preparation is required for MRI venography of the brain. You are allowed to eat at any time, including breakfast on the day of the study. The only thing a patient should take care of before an MRI is to remove all metal objects (watches, jewelry, glasses), and also leave credit cards, removable dentures, ballpoint pens, hearing aids and some others outside the office items. In the case where the patient has implanted ferromagnetic (capable of magnetization when exposed to a strong magnetic field) medical supplies, for example, pacemakers, stents, vascular clips, hearing aids, MRI venography is absolutely contraindicated for him. In this case, it is possible to perform a study using a CT machine.
How is the research conducted?
Cerebral venography is performed as a routine examination using a tomograph. The patient is invited to enter the room with the MR unit and is placed on a movable table, which will gradually move to the center of the ring formed by the magnet. At this time, special equipment catches and records signals reflected from the internal structures of the brain, including from blood vessels, resulting in the formation of a certain picture that allows one to confirm or exclude a preliminary diagnosis. In general, the study does not cause discomfort to the patient and takes from 20 to 30 minutes.