Causes of obliterating atherosclerosis of the arteries
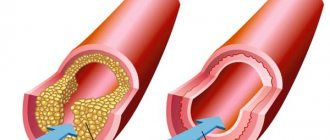
The disease causes severe circulatory failure in the legs, dooms patients to excruciating suffering and makes them unable to work. The process is localized mainly in large vessels (aorta, iliac arteries) or medium-sized arteries (femoral, popliteal arteries).
The most striking sign of ischemia of the lower extremities is intermittent claudication, characterized by the appearance of pain, a feeling of numbness and compression in the leg muscles when walking. This sensation forces the patient to stop, after which the pain and compression gradually disappear, but when the load is resumed, the pain returns. The affected leg is usually paler than the opposite leg and cold to the touch. Even minor injuries (scratches, bruises, abrasions) heal poorly and can cause ulcers. The feeling of numbness and pain at rest is often also caused by ischemia of the nerve trunks (ischemic neuritis). Prolonged course of the disease leads to the development of gangrene and inevitable amputation.
The degree of damage to the vascular bed is based on the walking distance. The pain forces the patient to stop, waiting for it to disappear. Without treatment, the disease continues to progress, which leads to a decrease in walking distance, limitation of the patient’s physical activity, and the inability to lead a normal lifestyle. Unfortunately, most often patients associate these pain sensations simply with muscle fatigue due to age, or with venous problems, defining the pain as a cramp, thus delaying seeking medical help and deepening the degree of damage to the arterial bed. In severe cases, the patient cannot walk 10 meters without stopping, but then it gets even worse: pain appears at rest, initially passing in an upright position, but after a short period of time the pain becomes constant, taking painkillers becomes ineffective. Gradually, the lumen of the artery narrows, leading to complete closure. Doctors are forced to admit that patients seek medical attention. help is late when the damage to the limbs is irreversible.
Risk factors:
- smoking;
- regular increase in blood pressure;
- high concentration of total cholesterol and its components in the blood;
- overweight (obesity);
- sedentary lifestyle (hypodynamia);
- diabetes;
- cardiovascular diseases in close relatives.
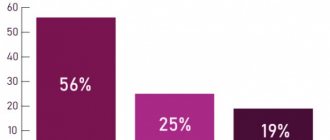
Damage to the vascular system of the lower extremities is a life-threatening condition, and ranks third in the structure of mortality from cardiovascular diseases. This figure is due to the development of such a severe complication as gangrene of the limb, which often leads to the need for amputation, and with high amputation, the mortality rate is 25%. Along with this, it should be noted that 50% of patients die within a year without amputation after the diagnosis of “critical ischemia”.
Symptoms of obliterating atherosclerosis of the arteries of the lower extremities
Pay attention to the following symptoms in yourself or your loved ones:
- fatigue in the calf muscles or thigh muscles when walking 500 meters or less,
- a feeling of leaden heaviness in the legs or muscle pain that makes you stop when walking,
- changes in the skin on the legs in the form of peeling, thinning, hair loss.
Important!
These are signs of atherosclerotic damage to the arteries of the lower extremities. An examination by a vascular surgeon is required in the near future. Do not be surprised if, when diagnosing lesions of the arteries of the lower extremities, your carotid arteries are checked and a cardiological examination is prescribed. Atherosclerosis is a systemic disease, and, as a rule, different groups of blood vessels are affected.
If sharp pain in the foot or lower leg occurs simultaneously with paleness and coldness of the skin, you must immediately call an ambulance, otherwise you may not have time to save the limb.
Definition
Vessels of the legs - arteries, arterioles, capillaries, veins and venules that supply blood to the tissues of the lower extremities.
Healthy leg blood vessels are an important component of human health. They supply the legs with blood, oxygen and nutrients, allowing a person to lead a full, active life. When the vessels of the legs are exposed to diseases, without proper and timely treatment this leads to serious consequences. The arteries of the lower extremities are paired. Here are the main ones:
- femoral artery (continuation of the iliac artery)
- popliteal artery (divides into tibial arteries)
- artery of the foot.
The veins of the lower extremities are divided into superficial and deep. The deep veins are paired; they accompany the arteries and participate in the process of blood drainage. Excessively dilated blood vessels in the legs are not only an aesthetic problem, but also a sign of pathological processes in the body.
The main methods for diagnosing obliterating atherosclerosis of the arteries of the lower extremities:
- measurement of the ankle-brachial index (the ankle-brachial index is a parameter that allows you to assess the adequacy of arterial blood flow in the lower extremities);
- duplex scanning of the arteries of the lower extremities is the “gold standard” for screening patients (detection and follow-up);
- MSCT angiography of the aorta and arteries of the lower extremities is the “gold standard” of preoperative examination and in cases where information from ultrasound scanning is insufficient;
- X-ray contrast angiography.
Indications and contraindications for the treatment method
Patients who are in good general condition are selected for bypass surgery. Therefore, a detailed assessment of comorbidities, obesity and other life-threatening factors is carried out. Only an immediate threat to life is a reason for risk in patients with severe concomitant diseases.
It is necessary to evaluate the vascular bed in detail using diagnostic ultrasound and angiography in order to formulate a clear concept for the operation.
A careful assessment of the saphenous veins is necessary, since the success of bypass surgery and the duration of the bypass operation depend on their quality. The use of artificial prostheses as shunts is an operation of despair, since such shunts close in half of the cases within 2 years.
Treatment methods for obliterating atherosclerosis of the arteries of the lower extremities:
Conservative therapy
In the early stages of obliterating atherosclerosis of the arteries of the lower extremities, conservative treatment is indicated, which must be comprehensive, and all unfavorable factors causing vasospasm must be excluded. A necessary condition for successful treatment is quitting smoking(!). Physical activity is of paramount importance. Patients with intermittent claudication should walk daily for 30-45 minutes - this promotes the development of small arteries, leads to an increase in muscle strength and an increase in the distance traveled without pain.
If pain and compression appear in the leg muscles, the patient should stop, and after these sensations disappear, continue walking. Often, cycling or swimming are much better tolerated than walking (however, they do not replace it). Correction of increased blood pressure, normalization of blood cholesterol levels, blood glucose levels in patients with diabetes mellitus. Drugs are used that reduce the tone of small vessels, increase the flexibility of red blood cells and prevent the formation of blood clots in the vessels. Physiotherapeutic and balneological procedures, hyperbaric oxygenation are also used.
Surgical treatment of arteriosclerosis of the arteries of the lower arteries, vessels
Reconstructive operations:
- X-ray endovascular treatment methods.
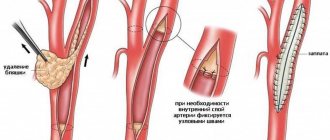
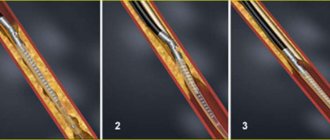
Under the control of X-rays using special long thin instruments, through a small puncture in the femoral artery (less often other arteries), we can reach the affected vessel (area of blood vessels) of the lower extremities. Modern technical capabilities make it possible to expand a section of the vessel from the inside with a special balloon and, if necessary, install a thin metal frame (stent) that prevents re-narrowing.
- Open surgical interventions.
For patients with blockage of a vessel lasting no more than 7-9 cm, the internal modified layer of the artery with atherosclerotic plaque and blood clots is removed (endarterectomy). With a more significant spread of the occlusive process, pronounced calcium deposition in the artery wall, a bypass of the blood flow (bypass) or resection of a section of the artery and its replacement with a synthetic prosthesis or biomaterial (prosthetics) is indicated.
Amputation
If, despite the treatment, ischemia of the affected limb increases and gangrene progresses, amputation is indicated: its level must be strictly individual and carried out taking into account the blood supply to the limb.
How is the examination carried out?
The doctor examines and interviews the patient and prescribes a comprehensive examination. It includes laboratory tests and vascular diagnostics. Various methods, including instrumental ones, help to assess the condition of blood vessels.
Today, examination of the blood vessels of the legs is carried out using modern equipment. These are angiography, Doppler ultrasound, magnetic resonance angiography and others. Once the diagnosis is made, the patient is prescribed treatment and given recommendations regarding his lifestyle. If the condition is not severe, standard drug treatment and prevention of atherosclerosis are prescribed. If there are vascular diseases of the extremities, the patient is advised to immediately stop smoking, move more, consume less salt and animal fats, and control weight. When the vessels are significantly affected and drug treatment does not bring results, the patient is recommended to undergo surgery. Read more about how obliterating atherosclerosis of the arteries of the lower extremities is treated in the following publication.
Symptomatic interventions:
- Sympathectomy
(intersection of the nerve plexuses responsible for spasm (narrowing) of the arteries) is performed for repeated blockages of the arteries and in addition to reconstructive operations. This operation improves blood circulation in the extremities by dilating small arteries. - Revascularization osteotomy
is also an adjuvant technique that improves blood circulation by stimulating the formation of new small vessels in the lower extremities after bone injury. - Arterialization of the venous bed
is rarely used at this time, since its implementation is associated with various technical difficulties, and long-term results are worse than the methods described above.
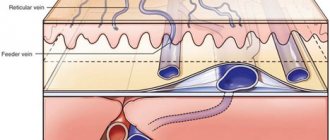
Basics of the venous system of the lower extremities
The peculiar structure of venous vessels and the composition of their walls determines their capacitive properties. Veins differ from arteries in that they are tubes with thin walls and lumens of relatively large diameter. Just like the walls of arteries, the composition of the venous walls includes smooth muscle elements, elastic and collagen fibers, among which there are much more of the latter.
In the venous wall, structures of two categories are distinguished: - supporting structures, which include reticulin and collagen fibers; - elastic-contractile structures, which include elastic fibers and smooth muscle cells.
Under normal conditions, collagen fibers maintain the normal configuration of the vessel, and if the vessel is exposed to any extreme impact, then these fibers maintain it. Collagen vessels do not take part in the formation of tone inside the vessel, and they also do not affect vasomotor reactions, since smooth muscle fibers are responsible for their regulation.
Veins consist of three layers: - adventitia - outer layer; - media - middle layer; - intima - inner layer.
Between these layers there are elastic membranes: - internal, which is more pronounced; - external, which differs very little.
The middle lining of the veins consists mainly of smooth muscle cells, which are located along the perimeter of the vessel in the form of a spiral. The development of the muscle layer depends on the width of the diameter of the venous vessel. The larger the diameter of the vein, the more developed the muscle layer is. The number of smooth muscle elements increases from top to bottom. The muscle cells that make up the tunica media are located in a network of collagen fibers that are highly convoluted in both the longitudinal and transverse directions. These fibers straighten only when a strong stretch of the venous wall occurs.
Superficial veins, which are located in the subcutaneous tissue, have a very developed smooth muscle structure. This explains the fact that superficial veins, unlike deep veins located at the same level and having the same diameter, perfectly resist both hydrostatic and hydrodynamic pressure due to the fact that their walls have elastic resistance. The venous wall has a thickness that is inversely proportional to the size of the muscle layer surrounding the vessel.
The outer layer of the vein, or adventitia, consists of a dense network of collagen fibers, which create a kind of frame, as well as a small number of muscle cells that are longitudinally located. This muscle layer develops with age and can be most clearly observed in the venous vessels of the lower extremities. The role of additional support is played by venous trunks of more or less large size, surrounded by dense fascia.
The structure of the vein wall is determined by its mechanical properties: in the radial direction the venous wall has a high degree of extensibility, and in the longitudinal direction it has a low degree. The degree of vessel distensibility depends on two elements of the venous wall - smooth muscle and collagen fibers. The rigidity of the venous walls during their strong dilatation depends on collagen fibers, which prevent the veins from stretching too much only under conditions of a significant increase in pressure inside the vessel. If changes in intravascular pressure are physiological in nature, then smooth muscle elements are responsible for the elasticity of the venous walls.
Venous valves
Venous vessels have an important feature - they have valves, with the help of which centripetal blood flow in one direction is possible. The number of valves, as well as their location, serves to ensure blood flow to the heart. On the lower limb, the largest number of valves are located in the distal sections, namely slightly below the place where the mouth of the large inflow is located. In each of the trunks of the superficial veins, the valves are located at a distance of 8-10 cm from each other. Communicating veins, with the exception of valveless perforators of the foot, also have a valve apparatus. Often, perforators can flow into deep veins with several trunks that resemble candelabra in appearance, which prevents retrograde blood flow along with the valves.
Vein valves usually have a bicuspid structure, and how they are distributed in a particular segment of the vessel depends on the degree of functional load. The framework for the base of the venous valve leaflets, which consist of connective tissue, is the spur of the internal elastic membrane. The valve leaflet has two endothelial-covered surfaces: one on the sinus side, the second on the lumen side. Smooth muscle fibers located at the base of the valves, directed along the axis of the vein, as a result of changing their direction to transverse, create a circular sphincter that prolapses into the sinus of the valve in the form of a kind of attachment rim. The valve stroma is formed by smooth muscle fibers, which run in fan-shaped bundles onto the valve leaflets. Using an electron microscope, you can detect oblong-shaped thickenings - nodules, which are located on the free edge of the valve leaflets of large veins. According to scientists, these are peculiar receptors that record the moment when the valves close. The leaflets of an intact valve are longer than the diameter of the vessel, so if they are closed, longitudinal folds are observed on them. The excessive length of the valve leaflets, in particular, is due to physiological prolapse.
The venous valve is a structure that has sufficient strength that can withstand pressures of up to 300 mmHg. Art. However, part of the blood is discharged into the sinuses of the valves of large veins through the thin tributaries that do not have valves flowing into them, which is why the pressure above the valve leaflets decreases. In addition, the retrograde blood wave is scattered against the rim of the attachment, which leads to a decrease in its kinetic energy.
With the help of fibrophleboscopy performed during life, you can imagine how the venous valve works. After the retrograde wave of blood enters the sinuses of the valve, its leaflets begin to move and close. The nodules transmit a signal that they have touched to the muscle sphincter. The sphincter begins to expand until it reaches the diameter at which the valve flaps open again and reliably block the path of the retrograde blood wave. When the pressure in the sinus rises above the threshold level, the opening of the draining veins occurs, which leads to a decrease in venous hypertension to a safe level.
Anatomical structure of the venous system of the lower extremities
The veins of the lower extremities are divided into superficial and deep.
The superficial veins include the cutaneous veins of the foot, located on the plantar and dorsal surfaces, large and small saphenous veins and their numerous tributaries.
The saphenous veins in the foot area form two networks: the cutaneous venous plantar network and the cutaneous venous network of the dorsum of the foot. The common dorsal digital veins, which enter the cutaneous venous network of the dorsum of the foot, as a result of the fact that they anastomose with each other, form the cutaneous dorsal arch of the foot. The ends of the arch continue in the proximal direction and form two trunks running in the longitudinal direction - the medial marginal vein (v. marginalis medialis) and the marginal lateral vein (v. marginalis lateralis). On the lower leg, these veins are continued in the form of the large and small saphenous vein, respectively. On the plantar surface of the foot, a subcutaneous venous plantar arch stands out, which, widely anastomosing with the marginal veins, sends the intercapitate veins to each of the interdigital spaces. The intercapitate veins, in turn, anastomose with those veins that form the dorsal arch.
The continuation of the medial marginal vein (v. marginalis medialis) is the great saphenous vein of the lower limb (v. saphena magna), which along the anterior edge of the inner side of the ankle passes to the lower leg, and then, passing along the medial edge of the tibia, goes around the medial condyle, exits to the inner thigh at the back of the knee joint. In the area of the lower leg, the GSV is located near the saphenous nerve, through which the skin on the foot and lower leg is innervated. This feature of the anatomical structure must be taken into account during phlebectomy, since damage to the saphenous nerve can cause long-term and sometimes life-long disturbances in the innervation of the skin in the lower leg area, as well as lead to paresthesia and causalgia.
In the thigh area, the great saphenous vein can have from one to three trunks. In the area of the oval-shaped fossa (hiatus saphenus) there is the mouth of the GSV (saphenofemoral anastomosis). At this point, its terminal section bends through the seropid process of the lata fascia of the thigh and, as a result of perforation of the cribriform plate (lamina cribrosa), flows into the femoral vein. The location of the saphenofemoral anastomosis can be 2-6 m below where the pupart's ligament is located.
Along its entire length, the great saphenous vein is joined by many tributaries that carry blood not only from the area of the lower extremities, from the external genitalia, from the area of the anterior abdominal wall, but also from the skin and subcutaneous tissue located in the gluteal region. In normal condition, the great saphenous vein has a lumen width of 0.3 - 0.5 cm and has from five to ten pairs of valves.
Permanent venous trunks that drain into the terminal portion of the great saphenous vein:
- v. pudenda externa - external genital, or pudendal, vein. The occurrence of reflux along this vein can lead to perineal varicose veins;
- v. epigastrica superfacialis - superficial epigastric vein. This vein is the most constant tributary. During surgery, this vessel serves as an important landmark by which the immediate proximity of the saphenofemoral anastomosis can be determined;
- v. circumflexa ilei superfacialis – superficial vein. This vein is located around the ilium;
- v. saphena accessoria medialis – posteromedial vein. This vein is also called the accessory medial saphenous vein;
- v. saphena accessoria lateralis – anterolateral vein. This vein is also called the accessory lateral saphenous vein.
The external marginal vein of the foot (v. marginalis lateralis) continues with the small saphenous vein (v. saphena parva). It runs along the back of the lateral malleolus, and then goes up: first along the outer edge of the Achilles tendon, and then along its back surface, located next to the midline of the back surface of the leg. From this moment on, the small saphenous vein may have one trunk, sometimes two. Next to the small saphenous vein is the medial cutaneous nerve of the calf (n. cutaneus surae medialis), thanks to which the skin of the posteromedial surface of the leg is innervated. This explains the fact that the use of traumatic phlebectomy in this area is fraught with neurological disorders.
The small saphenous vein, passing through the junction of the middle and upper thirds of the leg, penetrates the zone of deep fascia, located between its layers. Reaching the popliteal fossa, the SVC passes through a deep layer of fascia and most often connects with the popliteal vein. However, in some cases, the small saphenous vein passes over the popliteal fossa and connects with either the femoral vein or tributaries of the deep femoral vein. In rare cases, the SVC flows into one of the tributaries of the great saphenous vein. In the area of the upper third of the leg, many anastomoses are formed between the small saphenous vein and the system of the great saphenous vein.
The largest permanent estial tributary of the small saphenous vein, which has an epifascial location, is the femoropopliteal vein (v. Femoroplitea), or vein of Giacomini. This vein connects the SVC with the great saphenous vein located on the thigh. If reflux occurs along the Giacomini vein from the GSV basin, this can cause varicose veins of the small saphenous vein. However, the opposite mechanism can also work. If valvular insufficiency of the SVC occurs, then varicose transformation can be observed in the femoropopliteal vein. In addition, the great saphenous vein will also be involved in this process. This must be taken into account during surgery, since if preserved, the femoropopliteal vein may be the reason for the return of varicose veins in the patient.
Deep venous system
Deep veins include veins located on the back of the foot and sole, on the lower leg, as well as in the knee and thigh area.
The deep venous system of the foot is formed by paired companion veins and arteries located near them. The companion veins encircle the dorsum and plantar region of the foot in two deep arcs. The dorsal deep arch is responsible for the formation of the anterior tibial veins - vv. tibiales anteriores, the plantar deep arch is responsible for the formation of the posterior tibial (vv. tibiales posteriores) and receiving peroneal (vv. peroneae) veins. That is, the dorsal veins of the foot form the anterior tibial veins, and the posterior tibial veins are formed from the plantar medial and lateral veins of the foot.
In the lower leg, the venous system consists of three pairs of deep veins - the anterior and posterior tibial veins and the peroneal vein. The main load for the outflow of blood from the periphery is placed on the posterior tibial veins, into which, in turn, the peroneal veins drain.
As a result of the fusion of the deep veins of the leg, a short trunk of the popliteal vein (v. poplitea) is formed. The knee vein receives the small saphenous vein, as well as the paired veins of the knee joint. After the knee vein enters this vessel through the lower opening of the femoropopliteal canal, it begins to be called the femoral vein.
The sural vein system consists of the paired gastrocnemius muscles (vv. Gastrocnemius), which drain the sinus of the gastrocnemius muscle into the popliteal vein, and the unpaired soleus muscle (v. Soleus), which is responsible for drainage into the popliteal vein of the sinus of the soleus muscle.
At the level of the joint space, the medial and lateral gastrocnemius veins flow into the popliteal vein through a common mouth or separately, emerging from the heads of the gastrocnemius muscle (m. Gastrocnemius).
Next to the soleus muscle (v. Soleus) the artery of the same name constantly passes, which in turn is a branch of the popliteal artery (a. poplitea). The soleus vein drains independently into the popliteal vein or proximal to the place where the opening of the gastrocnemius veins is located, or flows into it. The femoral vein (v. femoralis) is divided by most specialists into two parts: the superficial femoral vein (v. femoralis superfacialis) is located further from the place where the deep vein of the thigh flows into it, the common femoral vein (v. femoralis communis) is located closer to the place where it the deep vein of the thigh enters. This division is important both anatomically and functionally.
The most distal major tributary of the femoral vein is the deep femoral vein (v. femoralis profunda), which joins the femoral vein approximately 6-8 cm below where the inguinal ligament is located. A little lower is the place where the tributaries, which have a small diameter, enter the femoral vein. These tributaries correspond to small branches of the femoral artery. If the lateral vein that surrounds the thigh has not one trunk, but two or three, then at the same place its lower branch of the lateral vein flows into the femoral vein. In addition to the above vessels, the femoral vein, in the place where the mouth of the deep vein of the thigh is located, most often contains the confluence of two companion veins, forming a para-arterial venous bed.
In addition to the great saphenous vein, the common femoral vein also receives the medial lateral vein, which runs around the thigh. The medial vein is more proximal than the lateral vein. The place of its confluence can be located either at the same level with the mouth of the great saphenous vein, or slightly above it.
Perforating veins
Venous vessels with thin walls and varying diameters - from a few fractions of a millimeter to 2 mm - are called perforating veins. These veins are often characterized by an oblique course and are 15 cm long. Most perforating veins have valves that serve to direct the movement of blood from the superficial veins to the deep veins. Along with perforating veins, which have valves, there are valveless, or neutral, veins. Such veins are most often located in the foot. The number of valveless perforators compared to valved ones is 3-10%.
Direct and indirect perforating veins
Direct perforating veins are vessels through which the deep and superficial veins are connected to each other. The most typical example of a direct perforating vein is the saphenopopliteal anastomosis. The number of direct perforating veins in the human body is not so large. They are larger and in most cases are located in the distal areas of the limbs. For example, on the lower leg in the tendon part there are the perforating veins of Cockett.
The main task of indirect perforating veins is to connect the saphenous vein with the muscular vein, which has a direct or indirect connection with the deep vein. The number of indirect perforating veins is quite large. These are most often very small veins, which are mostly located where muscle masses are located.
Both direct and indirect perforating veins often communicate not with the trunk of the saphenous vein itself, but only with one of its tributaries. For example, the perforating veins of Cockett, which run along the inner surface of the lower third of the leg, where the development of varicose and post-thrombophlebic disease is quite often observed, is not connected to the deep veins by the trunk of the great saphenous vein itself, but only by its posterior branch, the so-called vein of Leonardo. If this feature is not taken into account, this can lead to relapse of the disease, despite the fact that the trunk of the great saphenous vein was removed during the operation. In total, there are more than 100 perforators in the human body. In the thigh area, as a rule, there are indirect perforating veins. Most of them are in the lower and middle third of the thigh. These perforators are located transversely, with their help the great saphenous vein is connected to the femoral vein. The number of perforators varies – from two to four. Under normal conditions, blood through these perforating veins flows exclusively into the femoral vein. Large perforating veins can most often be found immediately near the place where the femoral vein enters (Dodd's perforator) and where it exits (Gunther's perforator) from the Gunter's canal. There are cases when, with the help of communicating veins, the great saphenous vein is connected not to the main trunk of the femoral vein, but to the deep vein of the femur or to a vein that runs next to the main trunk of the femoral vein.
Prognosis after treatment method
General surgical complications:
- Bleeding during surgery is a rare occurrence; usually blood loss is 300-500 ml and does not require replacement.
- Suppuration of postoperative wounds - can be observed in weakened patients with diabetes and a purulent process on the foot. Most often the course is favorable, but it delays the patient’s recovery.
Specific complications:
- Reperfusion syndrome is a limb condition associated with the restoration of blood flow against the background of critical ischemia. It is characterized by severe swelling of the limb, pain, and hyperemia. Usually goes away within 2-3 weeks after surgery.
- Lymphorrhea is a prolonged leakage of lymph from incisions. A rare complication in our clinic, the cause of which is damage to enlarged lymph nodes in the groin area during surgical access to the femoral artery.
- The formation of false mycotic shunt aneurysms is a rare complication that occurs when an infection is associated with an autovenous shunt. This is a dangerous condition as it can lead to late shunt rupture or thrombosis.
- Thrombosis of an autovenous shunt can be early or late. Early thrombosis is associated with insufficient outflow through the shunt due to poor arteries below the shunt or high blood clotting. Late thrombosis is associated with the progression of atherosclerosis in the outflow or inflow arteries and scarring of the shunt itself. The use of anticoagulants and control angiography after bypass surgery can eliminate the causes of early thrombosis. To prevent later complications, observation by a vascular surgeon is necessary.
Possible complications during treatment
In situ femoral-tibial bypass.
This method involves the use of the patient’s own great saphenous vein, which remains in its usual place, but with the help of special techniques, arterial blood flow is allowed through it into small arteries on the lower leg and foot. Femoro-tibial bypass is the mainstay of treatment for critical ischemia and impending gangrene. Success, with the correct indications for surgery, is achieved in 90% of patients with incipient arterial gangrene (necrosis of the fingers, arterial trophic ulcers). The ability to walk on your own leg is preserved. A venous bypass can be made from the veins of the legs or arms if the main saphenous vein is not preserved.
Peroneal artery bypass
The smallest artery of the leg is the least affected by the atherosclerotic process. However, its capacity is often not enough for the full operation of the autovenous shunt, which leads to thrombosis. The peculiarity of operations on the peroneal arteries is the need to clearly assess the volume of blood flow. To unload the artery, special techniques are often used - unloading fistulas with veins far from the anastomosis.
Multi-storey "jumping" shunts
Patients are often denied leg preservation due to the lack of a good length and patent artery in the lower leg, however, we often see individual sections and branches of arteries with preserved blood flow. Our leading vascular surgeon I.M. Kalitko For such situations, a technique for multi-story bypass of the lower leg arteries has been developed. Often several short bypasses are performed to individual patent segments of the arteries. An important condition for the normal operation of such a complex reconstruction is a reliable assessment of the incoming and distributed blood volume. When shunts are overloaded, unloading fistulas can be used.
Methods for diagnosing the disease
The diagnosis is made by a phlebologist. He examines the patient lying and standing. The doctor needs to distinguish reticular varicose veins from telangiectasia, the initial stage of livedo reticularis, Klippel-Trenaunay syndrome, Maffucci syndrome, Bloom's syndrome, and port wine stain.
Ultrasound in duplex mode is prescribed. Using ultrasound, the condition of the vein valves is assessed. The diagnosis is established if a violation of the reticular blood flow is confirmed, i.e., there is obstruction and reflux of the superficial vessels.
An ultrasound scan is performed. Dopplerography shows the direction of blood movement. During the scan, the doctor asks you to hold your breath, strain, and simulate walking while lying down. An image of green and red vessels is displayed on the screen. The red color shows the extent of the pathological area, and the green color shows the functionality of the venous valve. The direction and speed of blood movement is indicated.