Phlebothrombosis of deep veins is today considered one of the most complex pathologies of modern angiology.
This disease is characterized by the formation of a thrombus (blood clot) in the lumen of the deep veins, which partially or completely blocks the blood flow in the vessel. The most common location of blood clots is the large veins of the leg.
The main distinguishing feature of phlebothrombosis is the weak fixation of the thrombus in the vessel, associated with the addition of inflammation of the vein, so its separation and further travel through the vascular system is difficult to predict.
The disease has a long latent course and is often accompanied by a dangerous and complex complication - thromboembolism of various vessels (pulmonary artery, coronary vessels of the heart, renal vessels, arteries and veins of the brain), which occurs after the separation of a blood clot or part of it.
Phlebothrombosis of the veins of the lower extremities occurs quite often, so it is necessary to know the causes, symptoms, diagnosis and treatment methods of the disease.
Pulmonary embolism is a dangerous complication of phlebothrombosis of the veins of the lower extremities
What is deep vein thrombosis?
Thrombosis (phlebothrombosis) of the deep veins of the lower extremities is the result of the formation of blood clots (thrombi) that obstruct the outflow of blood in the main venous vessels of the thighs and legs. The resulting blood clot blocks blood flow and makes it difficult for venous blood to rise from the legs to the lungs and heart.
Neglect of timely treatment can lead to complications, and in isolated cases, death.
Women are more susceptible to the disease than men, but the risk of developing the disease in women increases when taking combined oral contraceptives.
Diet for thrombophlebitis
A large amount of fresh vegetables, fruits, fiber, nuts, cereals, whole grain breads. Among products of plant origin, the following also have a beneficial effect on venous diseases:
- ginkgo biloba,
- ginger,
- red capsicum,
- valerian root,
- garlic,
- hawthorn berries.
Nutritional supplements and vitamins:
- vitamins C, A, E and B6,
- linseed oil,
- magnesium and calcium (in combination),
- Pycnogenol
Symptoms of deep vein thrombosis of the leg and thigh
The deep veins in the lower extremities (great and common femoral veins, popliteal vein, deep veins of the leg) are located far from the surface, so there are no visible signs of thrombosis in the early stages.
The first symptoms to look out for may be:
- pain and increased sensitivity;
- stiffness of movements;
- feeling of heaviness and pressure in the muscles.
Important:
discomfort in the legs is a reason to consult a doctor.
Make an appointment
With the further development of the disease, obvious signs appear:
- change in skin color;
- swelling starting from the foot;
- expansion of superficial veins;
- local temperature increase.
Important:
If you experience any of the symptoms described above, consult your doctor immediately. The appearance of these signs signals the transition of the disease to the acute stage.
The risk group for the development of phlebothrombosis includes:
- Pregnant women, especially in the second - early third trimesters, and women in the postpartum period.
- People who are overweight and lead a sedentary lifestyle and sedentary work.
- Elderly people especially with diseases of the musculoskeletal system.
- Patients with cancer.
- Patients with decompensated forms of cardiovascular diseases.
- Persons whose activities involve heavy lifting or changes in atmospheric pressure.
Primary risk factors for thrombosis:
- frequent or extensive surgical operations;
- wearing a central venous catheter;
- severe injuries to the legs or pelvis;
- prolonged immobility (bed rest, wearing a cast);
- individual blood characteristics (high blood clotting, high levels of homocysteine or fibrinogen);
- oncology;
- heredity (antithrombin deficiency, pathologies of the system, blood circulation or homeostasis, problems with the secretion and absorption of proteins C and S).
Important:
congenital hereditary and individual characteristics are the most dangerous risk factors for thrombosis.
Thrombosis in a pregnant woman: causes
During pregnancy, a number of serious changes occur in the female body. First of all, they are associated with hormonal changes, which affect the functioning of the blood coagulation system, causing the blood to become more viscous and thick. Another reason is the increase in the size of the uterus. It begins to exert a compressive effect on the inferior vena cava, causing disruption of the blood flow, leading to stagnation in the vessels of the legs. Another factor is increased body weight. The above leads to the development of thrombophlebitis. It can occur either as an independent disease or as a complication of thrombosis. Aggravating factors in this case are:
- The woman is over 35 years old;
- Congenital antithrombin deficiency;
- Long-term use of contraceptives;
- Serious injuries in the past;
- Presence of autoimmune diseases.
Diagnosis of deep vein thrombosis
After a visual examination and medical history, the doctor prescribes a general blood test and a coagulogram to determine the patient’s condition and blood clotting indicators. Next, ultrasound duplex scanning of the veins is prescribed to assess hemodynamic parameters and identify structural changes in the walls of the venous vessels. Along with ultrasound, the doctor may perform plethysmography and contrast venography.
If ultrasound is not possible, alternative diagnostic methods are:
- MSCT (multispiral computed tomography);
- MRA (magnetic resonance angiography).
The listed diagnostic tools are sufficient to make a diagnosis and choose an effective treatment method.
Symptoms of phlebothrombosis
Phlebothrombosis is often asymptomatic due to the fact that the thrombus partially closes the lumen of the vessel and does not interfere with the laminar flow of venous blood through the vessels. This condition is the most dangerous in its course, because the first manifestation of the disease may be pulmonary embolism due to the detachment of a blood clot from the vessel wall, which was not diagnosed in a timely manner. In some cases, the disease can progress so rapidly that several days pass from the onset of the disease to the formation of a blood clot (1-5).
The symptoms of phlebothrombosis are specific and depend on the location of the thrombosed vessel:
1. Deep vein thrombosis of the leg is accompanied by:
- swelling of the feet, ankles and legs in general;
- pain on palpation of the limb below the knee;
- local hyperthermia of the skin of the lower leg and ankle area as a result of the inflammatory process and increased blood circulation in the superficial vessels of the lower limb;
- the occurrence of pain, discomfort and tension in the calf muscles after prolonged sitting, standing in an upright position or excessive physical activity, as well as when making movements on the back of the foot. These signs may subside at rest, especially if the limb is in an elevated position;
2. With phlebothrombosis affecting the popliteal, superficial and deep femoral vein,
the following symptoms appear:
- pain in the femoral and popliteal region;
- swelling of the limb is more widespread and covers almost the entire limb, including limiting mobility.
3. With phlebothrombosis of the iliofemoral vessels
(ileofemoral thrombosis) with complete blockage of the lumen of the vessel (common femoral vein, deep femoral vein and/or external iliac vein), an acute disturbance of blood circulation in the venous vessels occurs. The following symptoms appear:
- general body temperature rises;
- pain can spread not only to the entire limb, but also appears in the inguinal, iliac and lumbosacral regions, in the lower abdomen;
- swelling appears throughout the entire limb, and swelling can also spread to the groin area, perineum, and even to the area of the gluteal muscles and abdomen;
- The appearance of a pale bluish color of the skin of the affected limb is characteristic.
- On the affected side, dilated (dilated) areas of superficially located veins appear; they can also be visible in the groin area and on the abdominal wall.
According to the degree of hemodynamic disturbances that occur in the limb with iliofemoral phlebothrombosis, three forms are distinguished:
- 1) White painful swelling
(Phlegmasia alba dolens) caused by severe spasm (narrowing) of the arteries located next to the thrombosed vein. The patient experiences severe pain. During the examination, pallor and swelling of the limb are observed, and a decrease in the pulse in it and a decreased local temperature are determined by touch; - 2) Blue painful edema
(Phlegmasia coerulea dolens) is a more severe form and develops as a result of white phlegmasia. The venous and arterial blood supply to the lower limb is disrupted. During the examination, the limb is cyanotic, there is pronounced swelling, involving the area of the perineum and pelvis, the pulsation of the vessels of the diseased limb is not palpable, resulting in severe pain. In the absence of emergency medical care, the patient quickly develops gangrene of the limb; - 3) Venous gangrene
is a necrotic lesion that is a consequence of impaired arterial and venous circulation. When the iliac vein is included in the pathological process, characteristic symptoms arise: swelling of the limb, perineum with genitals, lower part of the body, and sharp dilatation of the vessels of the anterior abdominal wall is observed.
4. Other forms of phlebothrombosis:
- Phlebothrombosis of the inferior vena cava (IVC) usually occurs suddenly, but is often a consequence of the progression of bilateral ileofemoral phlebothrombosis.
- thrombosis of the subrenal, renal and hepatic segments of the IVC. The degree of manifestation of the clinical picture depends on the degree of hemodynamic disturbances and on the localization of the thrombus in the IVC. If the thrombus does not close the lumen of the vessel and is located parietally and blood flow in the subrenal segment of the IVC remains, then clinical signs may not appear. However, the likelihood of pulmonary embolism is high. If blockage of the renal veins occurs, acute renal failure occurs, manifested by lower back pain, oliguria, anuria, followed by possible death. With phlebothrombosis of the hepatic segment of the IVC, hemodynamics in the hepatic veins are disrupted, as a result of which the liver enlarges, ascites appears, jaundice, and the vessels of the anterior abdominal wall and lower part of the chest dilate.
Conservative treatment methods
Bed rest
Before the examination, all patients are prescribed bed rest. When diagnosing occlusive and parietal forms of venous thrombosis, it is canceled, in other cases it is maintained until blood flow is restored and the threat of thrombus separation is eliminated.
Compression jersey
According to indications for deep vein thrombosis, compression stockings of 2 or 3 compression classes are used.
Important:
Elastic compression can only be used as prescribed by a doctor. In some cases it is contraindicated.
Drug therapy
Injections of direct anticoagulants (sodium heparin, etc.) are mandatory for everyone in the treatment of deep vein thrombosis of the lower extremities. They prevent the formation of blood clots.
Having passed the acute stage, they switch to indirect anticoagulants (warfarin, etc.)
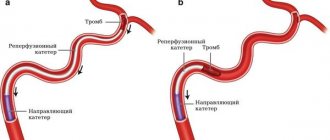
In addition to anticoagulants, thrombolytic therapy may be prescribed, aimed at restoring blood flow and destroying formed blood clots.
Sometimes in the acute stage a combination of direct and indirect anticoagulants may be used, depending on the specific case.
Surgery
Surgery for deep vein thrombosis of the legs is rarely required.
The operation is prescribed for:
- restoration of vein patency;
- maintaining the function of venous valves;
- preventing pulmonary thromboembolism.
Treatment of ileofemoral thrombosis
All patients without exception with an established diagnosis of “ileofemoral thrombosis” are required to be hospitalized in an angiosurgical hospital. The patient must be transported in a supine position. Until medical assistance is provided, he must adhere to the strictest bed rest. If it is not possible to perform a qualitative examination of the victim, then he is prescribed anticoagulants, fibrinolytics and thrombolytics for up to 10 days.
General recommendations for the management of patients with acute ileofemoral thrombosis:
- Anticoagulant drugs: low molecular weight Heparin, Logiparin, Fraxiparin.
- Eliminating pain, removing the patient from a state of shock.
- Relieving spasm from blood vessels, normalizing hemodynamics.
- Drugs for thrombolysis: Streptokinase or Urokinase. However, it should be remembered that the use of thrombolytic drugs is always associated with the risk of bleeding and death of the patient. Therefore, thrombolysis drugs are prescribed only to patients under the age of 50 years in whom acute thrombosis occurred no later than 7 days before visiting the doctor. In this case, patients must have vena cava filters installed, otherwise there is a high probability of small particles of a blood clot spreading through the bloodstream and developing a pulmonary embolism.
- Fibrinolysis activator drugs: Complamin, Teonicol, Nicotinic acid (intravenous administration), Pyrogenal (intramuscular administration).
- Normalization of rheological blood parameters is carried out with the help of drugs Trental, Eufillin, Actovegin, etc.
- If inflammation develops, antibiotics are indicated.
Surgery for ileofemoral thrombosis is prescribed only for vital indications: if the patient is diagnosed with floating blood clots that pose a threat to pulmonary embolism, or if complications of thrombosis develop. These include: embologenic thrombosis, a high risk of developing gangrene against the background of blue phlegmasia, ascending thrombosis.
There are also relative indications for surgery, including:
- Lack of effect from drug treatment for 2-3 days.
- The duration of thrombosis is more than 8 days.
- Senile age.
Thrombectomy is the main method of surgical intervention for ileofemoral thrombosis. It should be remembered that with blue phlegmasia, conservative therapy is useless in 100% of cases. The prognosis for blue phlegmasia is largely determined by how timely the surgical intervention was performed (before the development of gangrene). In this case, patients are indicated for radical throbectomy. The risk of pulmonary embolism increases when thrombectomy is performed on the right iliac vein.
Consequences of the disease: what is the danger of deep vein thrombosis of the lower extremities?
Postthrombophlebitic syndrome (PTPS)
Acute thrombosis of the lower extremities leads to a complex of hemodynamic disorders and the development of chronic venous insufficiency, united under the abbreviation PTFS. The consequences can be assessed after completion of the subacute stage of deep vein thrombosis of the legs (3 months after the end of the acute stage).
PTSD is expressed in the following symptoms:
- heaviness and pain in the area of maximum venous stagnation;
- swelling;
- phlebeurysm;
- trophic disorders (pigmentation, dermatitis, eczema, tissue compaction, trophic ulcers).
Pulmonary thromboembolism
Deep vein thrombosis is scary because the detached blood clot has a direct path to the lungs. Entering the pulmonary arteries through the right side of the heart, the thrombus causes disruption of gas exchange and provokes oxygen starvation. Depending on the size of the blood clot, the consequences can be different: from a normal cough with fever to pulmonary infarction, hypotension, tachycardia and fainting.
Venous gangrene
An overgrown blood clot can completely block a venous vessel and lead to stagnation of blood in the leg below the formation of the blood clot. Stopping blood flow causes tissue necrosis. The prognosis for the preservation of the affected areas is unfavorable. Delay threatens amputation and blood poisoning.
Causes of thrombophlebitis
The main causes of venous thrombosis:
- inflammatory process (local and/or general),
- slowing down the flow of blood through the venous vessels, leading to venous stagnation (for example, due to varicose veins),
- hereditary or acquired tendency of the blood to form blood clots (coagulopathies or thrombophilic conditions),
- damage to the venous wall (sometimes even minor trauma to the vessel, for example, catheterization of a vein).
Prevention
Recommendations for the prevention of deep vein thrombosis of the lower extremities: diet, exercise, clothing.
To prevent thrombosis, you need to pay attention to three things.
- Proper food: sufficient fluid in the diet and a healthy, balanced diet.
- Movement: morning exercises, five-minute walk every hour during sedentary work or static load on the legs.
- Care: compression stockings if there are risk factors and comfortable shoes.
Other articles by the author
- Chronic venous insufficiency
- Thrombophlebitis
- Deep vein thrombosis of the lower extremities
- Phlebeurysm
- Telangiectasias (vascular networks and spider veins on the legs)
Recommendations for changing the lifestyle of patients with thrombophlebitis
- Elevated position of the lower extremities during rest and sleep;
- Avoid prolonged static loads;
- Avoiding heavy physical activity (weight lifting);
- Avoid overheating and dehydration (long stay in the bathhouse);
- Wear compression hosiery of the required compression class (determined by a specialist);
- Limiting static loads (avoid sitting for long periods of time, standing without moving);
- Constant physical activity - walking, swimming, cycling;
- Selection of comfortable shoes and orthopedic insoles.