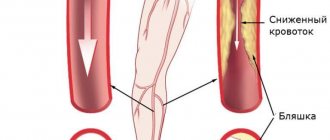
Occlusion of the femoral artery is a violation of its patency (blockage).
As a result of the occlusion, arterial, oxygenated blood stops flowing to the lower leg. Ischemia develops (local anemia).
Femoral artery occlusion occurs mainly in men. Persons over 50 years of age account for up to 75% of cases of the disease.
Femoral artery occlusion can be:
- segmental, affecting only a limited area of the artery;
- complete, when the entire artery is affected;
- combined with occlusions of other arteries of the lower extremities.
Diagnosis of acute ischemia during examination by a vascular surgeon
The classic picture of acute ischemia is determined by six symptoms:
- Sudden leg pain
- Pale skin
- Absence or deficit of movement in the affected limb
- Absence of pulse in the affected limb
- Decreased skin sensitivity
- Decreased skin temperature
The pain may be constant or with passive movement of the affected limb. With an embolic blockage, the pain is usually sudden and very intense. With thrombosis, the pain intensity is much less, and sometimes there is a progressive increase in intermittent claudication.
Symptoms of vascular occlusion
Acute occlusion of the vessels of the extremities is manifested by a symptom complex, designated in the English literature as the “complex of five Ps” (pain - pain, pulselessness - lack of pulse, pallor - pallor, paresthesia - paresthesia, paralysis - paralysis). The presence of at least one of these signs makes one think about possible acute occlusion of the vessels of the extremities.
Sudden pain distal to the site of occlusion occurs in 75-80% of cases and is usually the first sign of acute occlusion of the vessels of the extremities. If collateral circulation is preserved, pain may be minimal or absent. More often, the pain is diffuse in nature with a tendency to intensify, and does not subside when the position of the limb changes; In rare cases of spontaneous resolution of occlusion, the pain disappears on its own.
An important diagnostic sign of acute occlusion of the vessels of the extremities is the absence of pulsation of the arteries distal to the site of occlusion. In this case, the limb first turns pale, then acquires a cyanotic tint with a marbled pattern. Skin temperature is sharply reduced - the limb is cold to the touch. Sometimes, upon examination, signs of chronic ischemia are revealed - wrinkled and dry skin, lack of hair, brittle nails.
Disorders of sensitivity and motor sphere in acute occlusion of the vessels of the extremities are manifested by numbness, tingling and crawling sensations, decreased tactile sensitivity (paresthesia), decreased muscle strength (paresis) or lack of active movements (paralysis) first in the distal and then in the proximal joints . In the future, complete immobility of the affected limb may occur, which indicates deep ischemia and is a formidable prognostic sign. The end result of acute vascular occlusion can be gangrene of the limb.
Ultrasound duplex scanning
Ultrasound duplex scanning allows you to determine the patency of the arteries, localize the site of blockage of the vessel and the state of blood flow below the site of occlusion. Often, in acute ischemia, this diagnosis is enough to determine treatment tactics and send the patient to the operating table. With an embolism or rupture, the arteries below the blockage are usually empty or thrombosed, and blood flow in them is not detectable. Blood flow in the veins is sharply slowed down. With thrombosis, blood flow can be detected below the site of blockage, but its speed is sharply reduced; most often, blood flow through the main vessels cannot be detected, but blood flow can be seen through collaterals. As a rule, this is due to
Causes of femoral artery occlusion
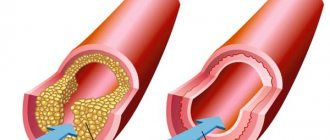
The cause of occlusion of the femoral artery in the majority (75-80%) of cases is obliterating atherosclerosis. Atherosclerosis is a disease in which cholesterol plaques are deposited on the walls of the artery, which over time block the lumen of the vessel. Also, occlusion of the femoral artery can be caused by injury, blood clot, and some other reasons.
Factors contributing to the development of occlusion
, are:
- smoking;
- high blood pressure;
- hereditary predisposition;
- improper diet (fatty foods);
- diabetes.
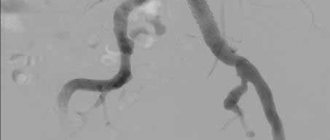
Angiography
To resolve the issue, surgical tactics require information about the patency of the arteries of the affected limb. The choice of technique for restoring blood circulation depends on the condition of the inflow pathways to the affected limb and the vascular bed below the site of blockage. In addition, angiography can distinguish embolism from thrombosis against the background of atherosclerotic narrowing. During an angiographic examination, endovascular treatment can be undertaken in the form of thrombectomy and angioplasty of the affected segments or local thrombolytic therapy can be performed.
Arterial embolism is an acute blockage of a vessel by a thrombus or other object brought from other parts of the vascular bed. Most often, vascular surgeons deal with thromboembolism from the heart cavity during a heart attack or atrial fibrillation, from the cavity of the aneurysm of the vessel overlying the blocked artery.
Consequences of acute cessation of blood flow
The sudden cessation of blood flow leads to the phenomenon of acute ischemia. The organs and tissues that are supplied by this artery lack nutrition and oxygen, so they begin to slowly die. The most specialized tissues are affected first—nervous, muscle, and finally skin. The body tries to restore blood circulation by opening additional bypass pathways for blood flow, so sometimes tissue death is stopped. But the likelihood of such an outcome is low. In any case, acute ischemia leads either to gangrene or to the development of chronic circulatory deficiency - critical ischemia.
Prognosis and prevention
The most important prognostic criterion for acute occlusion of the vessels of the extremities is the time factor. Early surgery and intensive therapy can restore blood flow in 90% of cases. If treatment is started late or is absent, disability occurs due to the loss of a limb or death. With the development of reperfusion syndrome, death can occur from sepsis, renal failure, or multiple organ failure.
Prevention of acute vascular occlusion of the extremities involves timely elimination of potential sources of thromboembolism and prophylactic administration of antiplatelet agents.
Stages of acute ischemia
1. Sudden pain in the leg, coldness, reduction in walking distance. If the collateral vessels are good, ischemia may stop at this stage with the development of intermittent claudication or critical ischemia. Most often, this stage is observed with thrombosis of altered arteries, if their lumen was previously narrowed and collateral circulation developed. At this stage, the operation is carried out after the necessary additional examination and preparation. The color of the leg may be pale or take on a bluish tint (cyanosis). The result of surgical treatment is excellent. Recovery of leg function is most often complete.
2. The symptoms described above are accompanied by weakness in the leg, which gradually worsens to the point of paralysis. However, passive movements in the fingers and other joints are possible. Such phenomena are associated with the death of nerve endings and blockade of nerve impulse transmission along the nerves. This stage of ischemia is an absolute indication for emergency surgery, since independent restoration of blood flow is impossible, and delay in intervention will lead to gangrene. Timely surgery restores blood flow with minimal loss of limb function. Numbness of the foot and fingers remains, and swelling of the leg persists for a long time.
3. Muscle death begins, first there are foci of muscle necrosis, muscle pain, and dense swelling of the lower leg. Then comes numbness of the fingers, ankle joint, and knee joint (muscle contracture). The muscles die completely. If the muscles are partially lost after restoration of blood flow and a long postoperative period, the leg may be preserved, but walking will be difficult. In the case of muscle contracture, amputation is necessary, since restoration of blood flow leads to the death of a person from poisoning with decay products.
Preparing for stenting
Before performing stenting surgery, the patient must be properly examined for vascular lesions and risks of complications. A set of laboratory tests and a coagulogram must be performed before surgery. Considering the patient's load on antithrombotic drugs, it is necessary to exclude possible sources of bleeding (stomach ulcer, bleeding hemorrhoids).
On the eve of the intervention, a light sedative is administered, allowing the patient to sleep well and not be nervous. Before the operation, the patient will shave the site of the intended access. In the preoperative room, the nurse will place a urinary catheter and an intravenous needle for infusions. In the operating room, a pressure cuff is placed on the shoulder and sensors for continuous ECG recording are fixed on the chest.
Diagnosis of thrombosis or embolism
In addition to the clinical picture, it is necessary to use special research methods for diagnosis.
Ultrasound diagnostics makes it possible to clarify the nature of occlusion and identify atherosclerotic plaques during thrombosis. Thrombosis differs from embolism in the initial damage to the arteries; in embolism, the arteries are most often not affected.
Angiography is performed on the operating table to clarify the receiving vascular bed and allows you to determine the nature of the surgical intervention
Multislice computed tomography is performed when there is time for a detailed diagnosis and allows you to very accurately identify the nature of the lesions and determine treatment tactics.
Atherosclerosis of the vessels of the lower extremities
In the last decade, endovascular techniques such as balloon angioplasty and stenting (endoprosthetics) have become widespread in the treatment of atherosclerotic lesions of the arteries of the lower extremities. Recommendations of the most famous European, American and Russian societies of angiologists and vascular surgeons (TASC, ACC/AHA, ROAC, CIRSE) consider them as the method of choice for segmental stenoses and occlusions of the arterial bed of the pelvis and lower extremities, regardless of the location of the lesion.
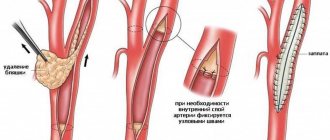
Rice. 1. Stages of endovascular stenting for atherosclerotic lesions of the superficial femoral artery (SFA): a) occlusion of the SFA, b) recanalization of the artery occlusion using a guide, c) implantation of an intravascular stent into the affected vessel, d) after the intervention - the patency of the artery is completely restored.
Rice. 2. Endovascular stenting for atherosclerotic lesions of the pelvic arteries: a) stenosis of the common iliac artery (arrow), total occlusion of the external iliac artery (double arrow), b) after the intervention - the patency of the pelvic arteries is completely restored (arrows).
Most experts from the most developed countries recommend that in emergency situations, when the disease threatens limb amputation, first of all, endovascular interventions are performed for any extent and nature of the lesion, hoping to maintain arterial patency within 12–24 months. postoperative observation. The basis for this is the rapid resolution of clinical symptoms, as well as the fact that endovascular interventions retain the possibility of repeated percutaneous interventions or traditional vascular operations.
Despite the high effectiveness of endovascular methods for treating atherosclerotic lesions of the arteries of the pelvis and lower extremities, the accumulated long-term world experience has made it possible to establish that in some clinical situations, X-ray surgical interventions have certain limitations.
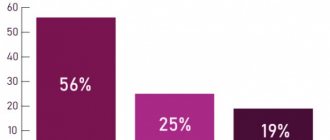
According to the most modern Charing Cross congress (England, London, May 2013), classical endovascular stenting of arteries in the femur and popliteal area with constant movement leads to long-term complications in 10-30% of cases, accompanied by fractures of the metal structure of the stent or restenosis inside it. In this regard, 81% of the participants in this congress voted against the implantation of traditional intravascular stents in the area of the arteries of the lower extremities.
Taking into account the recommendations of leading experts in the endovascular treatment of atherosclerotic lesions of the arteries of the lower extremities, the team of Professor S.A. Kapranov in their daily practice uses only the most modern instruments to restore vascular patency, the use of which ensures the preservation of the patient’s own tissues and does not require intravascular implantation in most cases prostheses and leads to a positive clinical result in 93% of patients. In the vast majority of cases, we try to achieve not a “cosmetic” result of the operation, accompanied by “beautiful” endovascular pictures after implantation of intravascular stents, which, as a rule, are provided to patients in most medical institutions, but to restore the patency of the patients’ own vessels.
!!! INNOVATION - for the treatment of atherosclerotic lesions of the arteries of the pelvis and lower extremities, our team primarily uses the most modern endovascular devices designed to eliminate the main cause of the disease - atherosclerotic plaques and thrombotic masses. These include the AngioJet (USA), TurboHawk (USA) systems for atherectomy and Ocelot (USA) for restoring the patency of extended vascular occlusions, which received international recognition at international congresses on endovascular surgery in 2010-2013.
Rice. 3. Endovascular thrombectomy from the iliac arteries with the AngioJet system: a) thrombosis of the external iliac artery (arrows), b) after the intervention - the patency of the artery is completely restored (arrows) - STENT IMPLANTATION IS NOT NECESSARY!
Rice. 4. The principle of endovascular removal of plaques from vessels: a) enlarged image of a carbon knife inside the catheter, b) the catheter is passed through the affected area of the artery, c) as it moves, the catheter cuts off atherosclerotic plaques, d) the cut atheromatous masses enter the catheter storage cone.
Rice. 5. Endovascular atherectomy from the arteries of the lower extremities: a) occlusion of the superficial femoral artery, b) an atherectome catheter cuts off plaques inside the vessel, c) after the intervention, the patency of the vessel is completely restored - STENT IMPLANTATION IS NOT NEEDED!, d-e) cut atheromatous masses inside the catheter and after removing them
!!! INNOVATION - even in those critical situations when the process of endovascular treatment requires dilatation or implantation of intravascular stents, the team of Professor S.A. Kapranov uses only the most modern materials - drug-coated balloon catheters, which increase the effectiveness of treatment in the long term by 32- 56%, and endovascular prostheses with a 5-year guarantee against breakage!!!
Request a call back Get a free consultation