Deep vein thrombosis of the lower extremities is a disease in which blood clots form in the lumen of the vein. The thrombus can completely cover the lumen of the vessel or only partially, settling on one of its walls. Vein thrombosis can occur in every patient with varicose veins of the lower extremities; in this case, the superficial and communicating (connecting) veins are more likely to thrombose. Deep vein thrombosis affects not only patients with chronic venous disease of the lower extremities, but also patients with blood diseases, diabetes mellitus, kidney disease, neurological pathology, pregnant women, cancer patients, people with disorders in the blood coagulation system or the so-called hypercoagulation syndrome.
The causes of deep vein thrombosis are as follows:
- expansion of the vein lumen and decrease in blood flow speed,
- violation of the integrity of the inner lining of the vessel, which creates an obstacle to blood flow and causes a delay of blood cells in this area, subsequently a blood clot forms there;
- Blood viscosity decreases, that is, the blood becomes thick, this occurs due to dehydration, fever, and endocrine disorders.
But the main cause of deep vein thrombosis is stagnation of venous blood in the legs or impaired venous outflow from the lower extremities. Against the background of the described reasons, after infectious diseases, surgical treatment, injuries of the lower extremities or significant physical activity, a blood clot forms. And the cause of stagnation can be a prolonged static position of the legs; this happens if a person is in a stationary position for a long time, standing on his feet or with his legs down. This applies mainly to representatives of the following professions: drivers, salesmen, teachers, machine operators, surgeons, hairdressers. Blood clots can often form during long flights, in those who work at a computer or sit in front of the TV for a long time.
The main danger of deep vein thrombosis of the lower extremities is that part of the thrombus, especially when its uppermost part or “thrombus head” is not attached to the wall, but is in a free position (floating thrombus), can come off and then, with the blood flow enter the pulmonary artery and from there into the lungs. This condition is called pulmonary embolism (PE). Against the background of this complication, blood flow in the lungs is disrupted, which is manifested by difficulty breathing, shortness of breath, a feeling of interruptions in the heart, dizziness, and a cough with streaks of blood in the sputum. If the necessary treatment measures are not started in time, the patient may die.
Deep vein thrombosis has very specific symptoms. The disease usually develops acutely, especially if there are provoking factors. First of all, swelling of the limb affected by thrombosis appears. If this is acute thrombosis of the deep vein of the thigh, then pronounced swelling of the thigh occurs, but more often thrombosis of the deep veins of the leg occurs and then the lower leg swells from the ankle to the knee. Then the skin turns blue, and when an infection occurs, the skin of the legs becomes crimson red. Bursting pain and itching of the skin can accompany this pathology. Superficial veins swell and protrude from the skin, leading to an increase in skin temperature. If treatment is not started on time or is started incorrectly, the blood clot can grow and reach the uppermost parts of the thigh, this is called total thrombosis of the limb.
Get an online consultation
right now.
Get
Diagnosis of deep vein thrombosis is based on Doppler ultrasound during angioscanning. Multislice computed tomography with contrast helps establish the topical picture. A biochemical blood test, called a coagulogram, helps to assess the state of the blood coagulation and anticoagulation systems. All additional research methods, as well as the diagnosis itself, are prescribed by a phlebologist.
Treatment of deep vein thrombosis is a long and labor-intensive process. First of all, it is necessary to stop the spread of thrombosis and try to dissolve already formed thrombotic masses, in order to prevent pulmonary embolism and fatal complications.
In the acute period, treatment is best done in a hospital. An elastic bandage is applied to the limb or compression stockings with maximum compression are put on. During a period of unstable swelling on the leg, when it is difficult to choose knitwear in size, it is wiser to use elastic bandages, but at the same time apply them in two layers at the site of blood clot formation. Compression therapy is not used in patients with atherosclerosis of the vessels of the lower extremities, due to the risk of ischemia, and who have eczema or dermatitis of the skin of the legs.
Anticoagulants are prescribed - drugs that thin the blood and dissolve the blood clot. They are usually given as a subcutaneous injection once a day. The drugs in this group are low molecular weight heparins: Clexane, Fraxiparine, Fragmin. These drugs inhibit the activity of the thrombin enzyme or coagulation factor Xa, resulting in increased anticoagulant and thrombotic effects. The blood becomes more fluid, and the formation of a blood clot stops. The state of the coagulation system is monitored by assessing coagulogram parameters. After 2-5 days, the patient is transferred to oral coagulants, which are prescribed for at least one month. The most common drug from this group of rivaroxaban is Xarelto, its course dose is 15 mg 2 times a day for 3 weeks, followed by a reduction in dosage to 20 mg per day in a single dose. Previously used blood clot traps - vena cava filters - are no longer used to prevent pulmonary embolism due to many dangerous complications. Their use can only be justified in cases of high risk and bleeding when anticoagulant therapy is prescribed.
For deep vein thrombosis, treatment is carried out with phlebotonics, drugs that normalize the tone of the venous vessel and improve venous outflow. “Antistax”, “Phlebodia”, “Detralex”, “Venarus” - this is a far from complete list for the treatment of this complication, which occurs in more than half of the cases in patients with varicose veins.
Deep vein thrombosis of the lower extremities (clinical and anatomical forms)
- Deep vein thrombosis of the leg
Complaints of swelling of the foot, pain and tension in the calves, pain when pressing on the calf muscles. If thrombosis does not spread, it is almost asymptomatic. Sometimes there is thromboembolism of small branches of the pulmonary artery with cough and the development of pneumonia (pneumonia). Treatment of thrombosis of the veins of the leg can be carried out on an outpatient basis, under the supervision of a phlebologist with control ultrasound examinations.
- Thrombosis of the popliteal vein
Has a clear clinical picture. Severe swelling and tension of the lower leg, swollen saphenous veins, severe pain when walking. Thrombosis of the popliteal vein is very dangerous due to frequent pulmonary embolism, so treatment is best carried out in a vascular hospital. Most often, conservative therapy is carried out with antithrombotic drugs (heparin). If the patient had a thromboembolism, then urgent surgical treatment is necessary - ligation of the femoral vein above the thrombus.
- Clinic for deep vein thrombosis of the thigh and iliofemoral segment (ileofemoral phlebothrombosis)
It is characterized by a severe general condition, pronounced swelling of the entire lower limb, and severe pain. The saphenous veins are sharply dilated, the leg takes on a bluish color. With ascending deep venous thrombosis, thrombosis of the entire venous bed is possible with a block of venous outflow and the development of venous gangrene (blue phlegmasia), which is accompanied by high mortality. Pulmonary embolism often occurs with a fatal outcome. Treatment of ileofemoral phlebothrombosis is only in a hospital. For occlusive thrombosis, conservative treatment is possible, but it is better to remove the thrombus so that post-thrombotic disease does not develop. In case of floating thrombosis, urgent removal of the thrombus (thrombectomy) using innovative methods is necessary. A vena cava filter can be installed in cancer patients.
- Thrombosis of the inferior vena cava
The most dangerous disease. Clinically, it is manifested by a severe general condition, swelling of both legs. Kidney failure and blood in the urine often develop. With thrombosis of the liver segment, liver failure develops resulting in Budd-Chiari syndrome. Treatment of acute thrombosis of the inferior vena cava should be active. It is necessary to remove thrombotic masses, as surviving patients may develop severe inferior vena cava syndrome. For this, it is good to use our innovative methods and systemic thrombolysis. The effectiveness of this treatment
- Asymptomatic thrombosis
It should be said right away that there are silent thromboses, that is, completely asymptomatic. Therein lies a great danger. This problem is becoming more and more acute, because with the expansion of ultrasound examination of veins, signs of previous thrombosis are being found more and more often. According to some phlebologists, by old age, most people experience such asymptomatic deep vein thrombosis. In quantity they even exceed those that can be diagnosed without the use of ultrasound methods. The patient does not even feel any health problems, and serious complications occur in the midst of complete well-being, in the event of an increase in blood clot and closure of the main veins. It is not uncommon for the disease to be discovered only after the patient dies from these complications. From this position, if there are no signs of the disease and you are at risk, there is only one way out - you need to direct all your efforts to prevention.
Diagnosis of acute deep vein thrombosis of the lower extremities is very difficult. Signs of deep vein thrombosis appear only in certain localizations of the process. This is primarily due to the absence of clinical symptoms. According to some data, out of 1000 venous thromboses, only 100 have any clinical manifestations. Of these, 60 patients will develop PE, but only 10 will have clinical signs.
It should be recognized that today there is not a single clinical symptom, laboratory or instrumental sign that would indicate with absolute certainty the presence of PE and DVT. Clinical manifestations of thrombosis and ultrasound results can be the basis for the correct diagnosis of venous thrombosis. The clinical picture of deep vein thrombosis consists of a complex of symptoms that characterize a sudden disturbance of venous outflow with preserved arterial blood flow to the limb. Swelling, cyanosis of the limb, bursting pain, local increase in skin temperature, overflow of the saphenous veins, pain along the vascular bundle are characteristic to one degree or another for thrombosis of any localization. Movements in the joints of the limb and sensitivity remain virtually unchanged. General signs such as low-grade fever, weakness, adynamia, and slight leukocytosis occur in most patients. The diagnosis of thrombosis largely depends on the location of the lesion and the level of distribution of thrombotic masses.
What is venous thrombophlebitis?
The disease is an inflammatory process that takes place in the venous wall, and is accompanied by the formation of blood clots (thrombi), which have different densities and close the lumen of the vein. As a result, partial or complete blockage of blood vessels occurs.
The pathology has an acute and chronic form, and can occur in superficial and deep veins. TF is most often diagnosed in the lower extremities, but it can also affect the venous vessels of any other parts of the body. If therapy is not carried out correctly and on time, it can cause undesirable consequences, including:
- purulent abscess;
- blood clot separation;
- blood poisoning.
Thrombophlebitis of the superficial veins has more severe symptoms compared to the disease affecting the deep veins. However, in both cases, timely diagnosis is very important, which will allow you to begin treatment without wasting time, and thereby avoid worsening the situation.
Contrast venography
A method of direct staining of deep veins using the injection of a contrast agent under x-ray control. Phlebography is performed immediately before endovascular intervention for venous thrombosis. In our clinic, the study is carried out with a safe contrast agent - carbon dioxide, which does not have a harmful effect on the kidneys. Phlebography allows you to answer questions about the localization of blood clots, the mechanical reasons for their formation, and the condition of bypass tracts. During phlebography, the surgeon can perform interventions such as installing a vena cava filter to prevent pulmonary embolism, dissolving blood clots, or installing a stent in the area of narrowing of the deep vein.
Reasons for education
Blood clots stick together much faster in the area where the pathological lesion occurred. This provokes a more rapid narrowing of the lumen and disruption of tissue nutrition. Key factors contributing to the development of the disease include:
- excess weight;
- lower limb injuries;
- varicose veins;
- incorrectly administered injection;
- the presence of tumors in the digestive system;
- low level of physical activity;
- previous operations;
- pregnancy;
- prolonged stay in an uncomfortable position;
- alcohol abuse and smoking;
- hormonal treatment and contraception;
- autoimmune processes.
Women are at higher risk of developing the disease due to high estrogen levels. It has also been proven that COVID-19 in 70% of cases causes an overreaction of the immune system, which causes a large number of blood clots to form.
The difference between thrombophlebitis and varicose veins
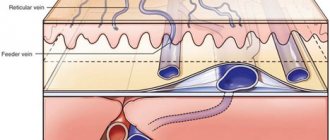
TF and varicose veins have similar symptoms. However, their nature is different. In the case of varicose veins, the vessels are dilated and their walls are thinned. The result is impaired blood flow and the formation of nodes. In the case of thrombophlebitis, inflammation of the venous walls and thrombus formation occurs. The thrombus clogs the lumen of the vessel, which leads to disruption of blood flow and swelling of the affected vessel.
The key difference between the diseases lies in the pathological mechanisms underlying each of them. Disruption of the functions of the valvular venous apparatus and excessive expansion of their lumen occurs as a consequence of destructive changes in the vessels formed under the influence of harmful factors. But the pathology occurs only with impaired blood circulation in the venous line and trophism of the soft tissues located around the affected vessel. A complication of varicose veins that cannot be treated is thrombophlebitis.
Exercises
A set of exercises allowed for thrombophlebitis of the lower extremities
With this pathology, patients are advised to do activities such as swimming in the pool and light exercise. These tasks have a minimal, gradual impact on the body, do not require sudden and intense movements, which are prohibited in this pathology, and help the body quickly get used to the load received.
The main methods allowed for the disease include:
- Measured walking with high knees and arms swing. On average, about 100 steps are performed. The main criterion for completing the task is correct breathing - slow, deep, it is recommended to inhale through the nose and exhale through the mouth.
- Running at an average or slow pace for short distances.
In a supine position
Exercises in a lying position:
- Legs and arms straight, make bending movements of the legs towards the chin. Perform about 10-15 times.
- Raise your legs straight up and stay in this position for a few seconds. Quantity – 5-10 times.
- “Bicycle” - performed lying on your back, arms parallel to the body. Alternately bending and straightening your knees, make circular movements, as when riding a bicycle. Execution time is within half a minute.
- Flexion and circular movements of the feet. Perform for half a minute.
- Alternately bend and straighten your knees, pressing them to your stomach. Performed 5-15 times on each leg.
- Lying on your side, raise your straight leg up about 10 times, then roll over to the other side and repeat the exercise on the other leg.
Exercises while sitting
Exercises in a sitting position:
- Pressing your legs together, slide your feet along the floor at a distance equal to the length of your foot. Repeat 10-15 times.
- Rest your heels and then relax your muscles – 10-15 times.
- While sitting, raise your legs on your toes, while tilting your body forward and putting pressure on your toes, hold in the position for 10 seconds, then relax.
- Make circular movements with your feet, first alternately, then with both feet together - 10-15 times in one approach. Can be repeated several times, resting between sets.
During training, the complexity of the exercises should be gradually increased - from the simplest to the more complex. The exercises should not be too difficult and should not cause discomfort.
What is prohibited for thrombophlebitis?
If a person develops a disease, he is strictly prohibited from:
- Wear uncomfortable high-heeled shoes.
- Lift heavy objects.
- Engage in sports that involve intense stress on the limbs.
TF of deep veins is a restriction for visiting saunas, drinking bowls and baths. This is due to the fact that high temperatures significantly accelerate blood circulation, which has an extremely negative effect on the course of the disease.
It is strictly forbidden to gain extra pounds, and therefore a person must pay special attention to proper nutrition. Animal fats, which can be replaced with vegetable oils, should be excluded from the diet. The amount of salt consumed should be kept to a minimum in order to eliminate swelling. Quitting alcohol and smoking is mandatory for TF.
Literature
1. Side-effects and complications of foam sclerotherapy of the great and small saphenous veins: a controlled multicentre prospective study including 1025 patients / JL Gillet // Phlebology. – 2009. – Vol. 24, N4. – P. 131–138.
2. Russian clinical recommendations for the diagnosis and treatment of chronic venous diseases // Phlebology. – 2013. – T. 7, No. 2. – P. 1–47
3. Kirienko, A.I. Compression sclerotherapy (a practical guide for doctors) / A.I. Kirienko, V.Yu. Bogachev, I.A. Zolotukhin. Ed. Academician of the Russian Academy of Sciences and Russian Academy of Medical Sciences V.S. Savelyeva. – M.: Publishing house NTsSSKh im. A.N. Bakuleva RAMS, 2004. – 40 p.
Why runners should be wary
DVT often occurs in athletes whose training involves endurance. For example, long-distance runners and cyclists.
The pulse is primarily to blame. Many athletes have a lower resting heart rate than the average person. This means that blood flow is also slowed down.
The second reason is muscle tension and increased risk of injury. Many runners experience swelling in their feet and legs. This weakens the blood vessels and can lead to damage to the walls.
The third and not entirely obvious reason is dehydration. If you don't drink enough water during and after training, your blood will thicken.
Ultramarathon runners are especially susceptible to DVT. Because in this case, long periods of tension are often followed by long periods of inactivity. Muscle stiffness, fatigue and exhaustion of the body aggravate the situation. In addition, such people may participate in competitions that require traveling by car or plane.
What can be done for thrombophlebitis?
For patients with thrombophlebitis of the legs, regular moderate physical activity is recommended, as well as wearing compression stockings during the day on an ongoing basis. Daily walking in comfortable shoes will also help improve the condition of a person suffering from TF. Physical activity is allowed, but the degree of its intensity must be determined together with the attending physician based on the stage of development and type of pathology, as well as the individual characteristics of the patient’s body.
Prevention of thrombophlebitis
If you have questions about how to treat thrombophlebitis and what measures to prevent it, you should contact a competent phlebologist. He will give precise recommendations regarding activities that will reduce the likelihood of developing the disease. People with two or more risk factors should definitely see a specialist. Prevention, carried out in time, will help eliminate the inflammatory process and the formation of blood clots in the veins. Prevention of the disease is also carried out to prevent its complications. Preventive measures include:
- Massage.
- Healthy lifestyle.
- Proper nutrition.
- Choosing the right clothes and shoes.
- Taking care of hygiene.
- Constant physical activity.
- Timely elimination of colds and infections.
Walking, swimming, cycling and dancing will have a positive effect on your health. Hardening procedures will help strengthen the walls of blood vessels.
Diagnostics
To diagnose the disease, you should contact a qualified specialist. He will conduct an examination and prescribe additional measures to study the patient’s condition, including:
- Ultrasound;
- phleboscintigraphy;
- angiography;
- phlebography.
Any experienced phlebologist will suspect TF already during a visual examination, during which he will detect dense and painful nodes located under the skin of a red tint. However, to accurately confirm the diagnosis, an ultrasound examination of the veins in the legs should be performed. This method will allow the doctor to examine thrombotic masses in the lumen of the vein and assess the degree and nature of thrombosis.
After examining the patient, the phlebologist receives data that will help him prescribe appropriate therapy. Yuzhny MC specialists conduct research using modern equipment from trusted manufacturers, which, combined with their qualifications, allows them to accurately identify the disease and begin its treatment.
Which doctor should I contact?
If there are clear signs of the development of TF or other vascular diseases (varicose veins, gangrene, thrombosis, tropical ulcers, etc.), you should consult a phlebologist. His competence includes examining the patient in order to make a diagnosis and subsequently prescribe treatment. You can also contact a specialist in this profile to receive clarification on preventive measures.
You can make an appointment with a phlebologist at a medical clinic, where experienced specialists work who have confirmed their qualifications with many years of successful experience in identifying and eliminating diseases of the venous system. The clinic is equipped with the latest technology, which allows diagnosis and treatment to be made even more efficiently and quickly.
Symptoms and signs of thrombophlebitis
Symptomatic signs of TF vary depending on the form of its course. In the case of acute pathology, its symptoms appear within the first two weeks. The subacute form is characterized by the manifestation of symptoms within a month.
If we are talking about TF of the superficial veins, then its signs are painful sensations when palpated, redness of the skin in the affected area, and the appearance of a clear venous pattern. TF of the deep veins is characterized by swelling. Symptoms also include:
- difference in temperature between healthy and affected areas;
- pain that increases with exercise;
- tissue tension;
- chills, etc.
Among the symptoms of the disease, there are also those that can only be detected during medical diagnosis. This:
- decreased blood circulation rate;
- thickening of vascular walls;
- occlusion;
- valve dysfunction;
- increased blood viscosity.
Thrombophlebitis, the symptoms of which are described above, requires urgent medical intervention if the swelling and pain are pronounced, and there is also fever or shortness of breath, accompanied by coughing attacks and spasms in the chest. These symptoms indicate an increased risk of blood clots breaking off and subsequently entering the lungs, which will lead to death.
Drug treatment
Prescription of medications for thrombophlebitis should be comprehensive:
- anticoagulants reduce blood clotting;
- non-steroidal anti-inflammatory drugs and antibiotics act on the very cause of blood clots – infection;
- for severe pain, painkillers are used;
- special external ointments help dissolve blood clots; anti-inflammatory gels are also applicable;
- Enzyme therapy is carried out to dissolve the blood clot and eliminate swelling;
- the action of venotonics is aimed at strengthening the walls of blood vessels and increasing their elasticity;
- Angioprotectors may also be additionally prescribed.
For the treatment of thrombophlebitis, the use of rutin is important. It increases the tone of large vessels, strengthens their walls, reduces swelling and inflammation. Heparin contained in ointments is no less important. Their use allows you to avoid taking medications internally.
In the absence of severe complications, the effect of drug therapy is felt within a few days.