Hemorrhagic stroke (HI) is a clinical syndrome in which there is a sharp development of focal and/or cerebral neurological symptoms due to spontaneous hemorrhage into the substance of the brain or into intrathecal areas. The pathological process is triggered by factors of non-traumatic genesis. This type of hemorrhage has the highest disabling ability and is associated with the highest risk of early death.
Statistics facts from reliable sources
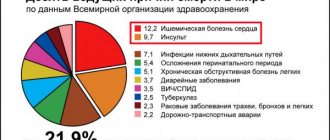
In the general structure of all types of strokes, hemorrhagic strokes account for 10%-15%. The frequency of its spread among the world population is about 20 cases per 100 thousand people. Experts, based on annual dynamics, report that in about 50 years all these indicators will double. Specifically in the Russian Federation, about 43,000-44,000 cases of HI are diagnosed annually. What is noteworthy is that it occurs approximately 1.5 times more often in men, but the mortality rate from its consequences predominates in women.
According to clinical observations, with this diagnosis, death occurs in 75% of people who are on mechanical ventilation, and in 25% of people who do not need it. Consolidated studies have shown that on average 30%-50% of patients die within 1 month from the moment of an attack of hemorrhage, and 1/2 of them die within the first 2 days. Disability (due to paralysis of the face and limbs, aphasia, blindness, etc.) among surviving patients reaches 75%, of which 10% remain bedridden. And only 25% of patients are independent in everyday life after 6 months.
Pathology represents a huge social problem, since the epidemiological peak occurs in working years - 40-60 years. Hemorrhagic strokes have become significantly “younger”; today they are quite common even among the youth group of people (20-30 years old). The risk category definitely includes people suffering from arterial hypertension, since in most cases this kind of hemorrhage occurs precisely because of chronically elevated blood pressure.
The primary factor that influences the prognosis of outcome is the promptness of providing adequate medical care to the patient.
Myocardial infarction and hemorrhagic alveolitis in systemic lupus erythematosus
Despite the well-known symptoms of systemic lupus erythematosus (SLE), each case of this disease is unique. The course of the disease is characterized by periods of exacerbations and remissions that occur while taking medications. Discontinuation of treatment is usually accompanied by exacerbation of SLE at varying intervals. The disease can begin with damage to one or more organs or progress at lightning speed, ending in death in a short period of time.
The main causes of death during the first year after the onset of the disease are the activity of SLE (damage to the kidneys, central nervous system - CNS) or the addition of an infection. Subsequent deaths may be caused by cardiovascular accidents, chronic renal failure and malignant neoplasms [1]. The use of glucocorticosteroids can reduce the incidence of deaths resulting from SLE activity.
We describe a patient with SLE in whom disease activity caused the development of disseminated intravascular coagulation (thrombohemorrhagic stage) and death in the first year after the onset of SLE.
Patient K., 18 years old, was admitted to the hospital of the Institute of Rheumatology of the Russian Academy of Medical Sciences in October 2003 with complaints of hemorrhagic rashes on the skin, pain in the right elbow, wrist and metacarpophalangeal joints of the right hand, swelling of these joints, hair loss, weakness, shortness of breath with physical activity.
The onset of the disease at the end of December 2002 was characterized by the appearance of erythema on the face, the development of arthritis of the small joints of the hands, low-grade fever, and a sharp decrease in body weight (in 2 months, I lost 6 kg). In January 2003, she was hospitalized in the rheumatology department of one of the hospitals in Moscow, where changes in urinary sediment (proteinuria, erythrocyturia and leukocyturia), anemia, increased antibodies to DNA and antinuclear factor (ANF, titers unknown) were detected, which allowed diagnose SLE. From the moment of diagnosis, she constantly received prednisolone (PZ - 35 mg/day), and after consultation at the Institute of Rheumatology (April 2003) also Plaquenil (400 mg/day). Despite the therapy, changes in urine tests (trace proteinuria and microhematuria) and immunological disorders persisted, and therefore cyclophosphamide - CP (total 1.2 g) was prescribed. Stop injections of CP and reduce the dose of PZ to 20 mg/day. provoked an exacerbation of SLE: in September 2003, a hemorrhagic rash appeared on the skin of the legs, and then throughout the body, painful aphthae in the mouth, arthritis and arthralgia recurred again, fever, and weakness began to increase. An episode of severe abdominal pain, nausea, and tarry stools occurred on September 30, and a decrease in hemoglobin to 81 g/l was noted. At the place of residence, the development of food toxic infection was excluded, rehydration therapy was carried out, after which the patient was sent to the Institute of Rheumatology. A brief history diagram is presented in Fig. 1.
Provocateurs of hemorrhagic stroke
The trigger for the appearance of HI can be quite a variety of factors that have a negative impact on intracranial hemodynamics and the condition of the cerebral vessels:
- persistent arterial hypertension (in 50% of cases);
- cerebral amyloid angiopathy (12%);
- oral administration of drugs from the anticoagulant spectrum (10%);
- intracranial neoplasms (8%);
- other causes are arteriovenous and cavernous malformations, thrombosis of the cerebral sinuses, aneurysms, vasculitis of intracranial vessels, etc. (20%).
Many of the patients with a history of hemorrhagic stroke have diabetes mellitus. It is a proven fact that diabetics, like hypertensive patients, are at risk. In long-term diabetes mellitus, blood vessels, including cerebral ones, are destroyed due to modification of blood chemistry with a predominance of glucose. If, against the background of elevated blood sugar, there is a tendency to constant increases in blood pressure, the likelihood of a hemorrhagic stroke increases by 2.5 times.
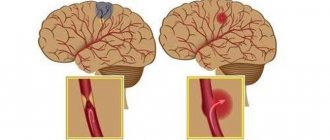
Pathogenetically, a hemorrhagic effect can develop as a result of rupture of a vessel (the predominant mechanism) or the leakage of blood elements into the surrounding brain tissue through the walls of capillaries due to their impaired tone and permeability. In the second option, there is no rupture and, as such, profuse hemorrhage. Just a small vessel allows blood to pass through pointwise. But even small-point hemorrhages, merging, can turn into very extensive foci, with no less fatal consequences than after a rupture of an artery or vein.
Clinical manifestations of HI
Shortly before the attack, pre-stroke clinical symptoms may precede the attack (not always), by which one can suspect impending danger:
- tingling, numbness of one facial half;
- numbness in fingers or toes;
- sudden weakness, dizziness, noise in the head;
- severe pain in the eyes, spots, double vision, vision in red;
- sudden staggering when walking;
- causeless tachycardia;
- attacks of hyperhidrosis;
- increased blood pressure;
- unreasonable occurrence of nausea;
- inhibition in communication and perception of other people's speech;
- flushing of the face, hyperthermia.
A cerebral stroke with hemorrhage is still characterized by an immediate acute onset without warning signs, which occurs during or almost immediately after vigorous activity, a stressful situation, or excitement. A hemorrhagic stroke is indicated by classic symptoms that develop suddenly, are pronounced and rapidly progress:
- sharp and severe headache;
- uncontrollable vomiting;
- prolonged depression of consciousness, coma;
- blood pressure above 220 mmHg.
Common signs of shock are also noisy breathing, epileptic seizures, lack of pupillary response to light, and spastic miosis. Depending on the location of the lesion, there may be a rotation of the head and rotation of the eyeballs in the direction of the affected hemisphere or contralaterally. Having discovered signs of GI in a victim, a person nearby must immediately call an ambulance!
Acutely developed hemorrhage leads to the fact that blood flows freely into certain structures of the brain, saturating them and forming a cavity with a hematoma. The bleeding continues for several minutes or hours until a blood clot forms. Over a short period of time, the hematoma quickly increases, exerting a mechanical effect on the affected areas. It stretches, presses and displaces the nervous tissue, causing its swelling and death, which leads to an intensive increase in neurological deficit (respiratory depression, loss of sensitivity of one half of the body, speech disorders, loss of vision, paresis of the swallowing muscles, etc.).
The size of the blood accumulation can be small (up to 30 ml), medium (from 30 to 60 ml) and large (more than 60 ml). The volumes of spilled liquid can reach critical levels, up to 100 ml. Clinical observations show that with intracranial hemorrhages exceeding 60 ml, the pathology ends in death in 85% of patients within 30 days.
Typical location of hemorrhages
Most often, and this is about 55% of cases, hemorrhages occur in the putamental zone. Putamental bleeding occurs due to rupture of degenerated lenticulostriate arteries, which causes blood to enter the brain shell. The culprit of pathogenesis with such localization is usually long-standing hypertension. In some cases, bleeding from the putamentum breaks into the ventricular system, which is fraught with tamponade of the gastrointestinal tract and acute occlusive-hydrocephalic crisis.
The next most common location is the subcortical region (subcortical). Subcortical GIs are observed in 17%-18% of cases. As a rule, the leading sources of such hemorrhage are ruptured AVMs and aneurysms against the background of increased pressure. The subcortical zones involved in the hemorrhagic process are the frontal, parietal, occipital or temporal lobe.
The third most common place, where brain hemorrhage is determined in 14%-15% of cases, is the optic thalamus, or thalamus. Thalamic hemorrhages occur due to the release of blood from the blood vessel of the vertebrobasilar region. Pathogenesis can be associated with any etiological factor, however, as always, the involvement of hypertensive syndrome is significantly more often noted.
In fourth place (7%) in terms of frequency of development are pontine GIs. They are concentrated in the back of the brain stem, that is, in the pons. Through the bridge, the cortex communicates with the cerebellum, spinal cord and other major elements of the central nervous system. This department includes the centers for controlling breathing and heartbeat. Therefore, the bridge is the most dangerous localization of hemorrhage, practically incomparable to life.
Causes
Since ischemic stroke is not considered as a separate disease, it is impossible to determine a single etiological factor for it. However, there are risk factors associated with an increased incidence of ischemic stroke, which can be divided into two groups:
1. Modifiable.
- myocardial infarction
- arterial hypertension
- atrial fibrillation
- diabetes
- dyslipoproteinemia
- asymptomatic lesions of the carotid arteries.
2. Unmodifiable.
- hereditary predisposition
- age
In addition, there are risk factors associated with lifestyle: low level of physical activity, acute stress or prolonged psycho-emotional stress, excess body weight, smoking.
Principles of disease diagnosis
The gold standard for making a diagnosis is computed tomography (CT). In the early period after an attack (1-3 days), this method of neuroimaging is more informative than MRI. Fresh hemorrhagic material, including 98% hemoglobin, appears on CT as a high-density, well-defined, bright inclusion against the background of darker brain tissue. Based on a computed tomogram, the epicenter zone, volume and shape of the formation, the level of damage to the internal capsule, the degree of dislocation of brain structures, and the state of the cerebrospinal fluid system are determined.
With the onset of the subacute phase (after 3 days), the red cells of the hematoma along the periphery are destroyed, in the center the iron-containing protein is oxidized, and the focus becomes lower in density. Therefore, along with CT scan, MRI is mandatory within 3 days and later. In subacute and chronic forms, the MR signal, in contrast to CT, better visualizes a hematoma with derivatives of hemoglobin oxidation (methemoglobin), which passes into the isodense stage. Angiographic examination methods are used in patients with an unknown cause of hemorrhagic stroke. Angiography is primarily performed on young people with normal blood pressure readings.
For adequate management of patients after an attack of intracerebral hemorrhage, an ECG and X-ray of the respiratory organs are required, and tests for electrolytes, PTT and APTT are taken.
Medical care in hospital
All patients receive intensive therapeutic care at an early stage in a neuro intensive care hospital. Initial treatment measures are aimed at:
- normalization of microcirculation, hemorheological disorders;
- relief of cerebral edema, treatment of obstructive hydrocephalus;
- correction of blood pressure, body temperature;
- functional regulation of the cardiovascular system;
- maintaining water and electrolyte balance;
- prevention of possible seizures;
- prevention of extracranial consequences of inflammatory and trophic nature (pneumonia, embolism, pulmonary edema, pyelonephritis, cachexia, DIC syndrome, endocarditis, bedsores, muscle atrophy, etc.);
- providing respiratory support (if the patient needs it);
- elimination of intracranial hypertension in HI with dislocation.
Prevention
Knowing your risk factors for stroke, following the advice of highly trained professionals, an annual comprehensive body check-up and a healthy lifestyle are the best steps you can take to prevent stroke. If you have had a stroke or transient ischemic attack (TIA), these steps may help prevent another stroke.
The help you receive in the clinic plays a significant role in stopping the acute period of a cerebral infarction.
The risk factors for possible complications after an attack will depend on how qualified and prompt assistance a team of neurologists, cardiologists, neurosurgeons, rehabilitation therapists and physiotherapists will provide you.
Many stroke prevention protocols are the same as cardiovascular disease prevention protocols. Basic recommendations for a healthy lifestyle include:
- Constant blood pressure monitoring. This is one of the most important things you can do to reduce your risk of stroke. If a patient has already had a stroke, lowering blood pressure may help prevent a subsequent TIA or stroke.
- Exercise, manage stress, maintain a healthy weight, and limit sodium, alcohol, and tobacco. In addition to recommending lifestyle changes, our doctor may prescribe medications to treat high blood pressure, as well as a vitamin and mineral supplement and fish oil.
- Reduce the amount of cholesterol and saturated fat in your diet. Eating less cholesterol and fat, especially saturated fat and trans fat, can reduce plaque in the arteries.
- Quitting tobacco use. Smoking increases the risk of stroke for smokers and nonsmokers exposed to secondhand smoke. Quitting tobacco use reduces the risk of stroke.
- Diabetes control.
- Maintaining a healthy weight. Excess weight contributes to the development of other risk factors for stroke, such as high blood pressure, heart disease and diabetes.
- A diet rich in fruits and vegetables. A diet containing five or more daily servings of fruits or vegetables may reduce the risk of stroke.
- Exercise can lower blood pressure. It will also help you lose weight, control diabetes and reduce stress.
Surgery for hemorrhagic stroke
The second stage of the treatment process is neurosurgical intervention. Its goal is to remove the life-threatening hematoma to improve survival and achieve the best possible satisfactory functional outcome. The sooner the operation is performed, the better prognosis can be expected. However, early surgery, as a rule, involves performing surgical procedures no earlier than 7-12 hours after the stroke. In the ultra-early period, it can lead to repeated bleeding.
When it is wiser to begin removing blood clots is decided by highly competent neurosurgeons. It was noted that operations performed even 2-3 weeks (inclusive) after the GI procedure can also lead to a positive effect. So the question of when to operate on a patient is entirely the responsibility of the doctor. Let us consider the fundamental surgical methods widely used for hemorrhagic strokes.
- Open decompressive craniotomy is indicated for medium and large subcortical, as well as large putamental and cerebellar hemorrhages. It is also addressed in case of pronounced displacement and increasing swelling of the cerebral component, deterioration of the patient’s neurological status. Open surgery is performed under complete general anesthesia using microsurgical optics. Removal of the accumulated clot is carried out through classic trepanation access. Next, an economical encephalotomy is performed, then the pathological component is sucked out with a special device. Dense accumulations are removed with fenestrated tweezers. At the end, the surgical field is thoroughly washed with sodium chloride solution, and thorough hemostasis is performed through coagulation and antihemorrhagic agents.
- The puncture-aspiration procedure is recommended for small hemorrhages of the thalamic, putamental, cerebellar location. The method consists of creating a small hole in the skull, puncturing the hematoma, and then freeing the brain from its liquid mass through aspiration. This technology can be implemented using one of two minimally invasive techniques: based on the principle of stereotactic or neuroendoscopic aspiration. Sometimes it is advisable to combine them with local fibrinolysis. Fibrinolysis involves installing drainage after puncture and aspiration into the hematoma cavity. Fibrinolytics are administered through the drainage over several days to activate the dissolution (liquefaction) of the blood clot and the removal of lysed blood elements.
Unfortunately, the functions of the central nervous system cannot be completely restored after hemorrhagic strokes. But in any case, it would be in the patient’s interests to go to a clinic where international-level doctors work in the diagnosis and surgical treatment of intracerebral lesions. This is the only way to ensure adequate and safe surgical support. Consequently, minimizing complications leads to more productive results in restoring quality of life.
We emphasize that the ideal execution of the operation in the right time increases the survival rate by 2-4 times. Proper postoperative care reduces the likelihood of relapse. It must be warned that a repeated stroke with hemorrhage in 99.99% of patients leads to death.
As a recommendation, we consider it important to say that the Czech Republic shows good results in the level of development of the field of brain neurosurgery in Europe. Czech medical centers are famous for their impeccable reputation and excellent rates of successful recovery of even the most difficult patients. And that’s not all: the Czech Republic has the lowest prices for neurosurgical care and one of the best postoperative rehabilitation. The choice of a medical institution for undergoing surgery, of course, remains with the patient and his relatives.
ICD-10
I63 Cerebral infarction
- Causes
- Pathogenesis
- Classification
- Symptoms of ischemic stroke Brain infarction in the MCA basin
- Cerebral infarction in the ACA basin
- Cerebral infarction in the PCA basin
- Cerebral infarction in the vertebrobasilar region
- Differential diagnosis
- Therapy in the acute period