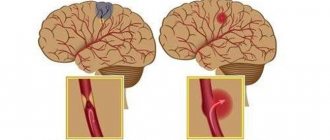
Hemorrhagic stroke (HI) is a clinical syndrome in which there is a sharp development of focal and/or cerebral neurological symptoms due to spontaneous hemorrhage into the substance of the brain or into intrathecal areas. The pathological process is triggered by factors of non-traumatic genesis. This type of hemorrhage has the highest disabling ability and is associated with the highest risk of early death.
Causes and mechanism of development of hemorrhagic stroke
The factors that cause rupture of the vascular wall and hemorrhage may be primary and secondary diseases of the cerebral arteries. Primary diseases initially develop in one or more vessels of the brain; they are not a consequence of any other diseases and often represent congenital changes. Secondary pathologies of the cerebral arteries appear against the background of other diseases, such as diabetes mellitus or systemic lupus erythematosus.
The most common primary factors may be:
- aneurysmal dilatation - an area where, due to the weakness of the vascular wall or the consequences of an injury, the artery becomes wider and adapts less well to increased blood pressure or other changes in vascular tone;
- vascular malformation is a congenital disorder of the structure of a vessel, which is manifested by the formation of “vascular glomeruli” with cavities of various sizes;
- other congenital anomalies of the arterial vessels of the brain.
Secondary causes that can lead to changes in cerebral vessels and their rupture include:
- arterial hypertension, especially difficult to treat;
- atherosclerotic damage to the vascular wall;
- vasculitis - inflammatory changes in the wall of blood vessels;
- thrombosis of intracranial veins, which lead to hemorrhage;
- diseases manifested by pathology of the coagulation system (blood and liver diseases);
- uncontrolled use of drugs that affect blood clotting (anticoagulants, antiplatelet agents, fibrinolytics);
- pronounced metabolic disorders that develop during long-term severe illnesses.
The most common cause of hemorrhagic stroke in elderly patients is arterial hypertension - this is about 80% of “vascular accidents”. The second place is occupied by atherosclerosis.
In age groups under 40 years, congenital local dilations of blood vessels (aneurysms) and malformations predominate among the causes of hemorrhagic stroke.
Due to the differences in the causes of the disease in different age groups, early and most accurate diagnosis of the pathology comes first. On our website you can find comprehensive information about methods for identifying risk factors for stroke, as well as find out in which centers they are carried out.
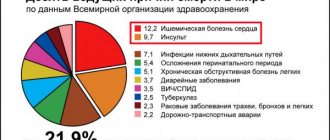
Statistics facts from reliable sources
In the general structure of all types of strokes, hemorrhagic strokes account for 10%-15%. The frequency of its spread among the world population is about 20 cases per 100 thousand people. Experts, based on annual dynamics, report that in about 50 years all these indicators will double. Specifically in the Russian Federation, about 43,000-44,000 cases of HI are diagnosed annually. What is noteworthy is that it occurs approximately 1.5 times more often in men, but the mortality rate from its consequences predominates in women.
According to clinical observations, with this diagnosis, death occurs in 75% of people who are on mechanical ventilation, and in 25% of people who do not need it. Consolidated studies have shown that on average 30%-50% of patients die within 1 month from the moment of an attack of hemorrhage, and 1/2 of them die within the first 2 days. Disability (due to paralysis of the face and limbs, aphasia, blindness, etc.) among surviving patients reaches 75%, of which 10% remain bedridden. And only 25% of patients are independent in everyday life after 6 months.
Pathology represents a huge social problem, since the epidemiological peak occurs in working years - 40-60 years. Hemorrhagic strokes have become significantly “younger”; today they are quite common even among the youth group of people (20-30 years old). The risk category definitely includes people suffering from arterial hypertension, since in most cases this kind of hemorrhage occurs precisely because of chronically elevated blood pressure.
The primary factor that influences the prognosis of outcome is the promptness of providing adequate medical care to the patient.
Types of intracranial hemorrhages
Depending on the location of the vessel from which the blood leaked, this type of stroke is divided into:
- parenchymal hemorrhage, characterized by the formation of a hematoma inside the brain or hemorrhagic impregnation of the nervous tissue;
- subarachnoid, which occurs when blood accumulates between the arachnoid and pia mater of the brain.
With parenchymal hemorrhage, depending on the caliber and location of the vessel, blood may break through into the ventricles of the brain. Such strokes are often characterized by an extremely severe course and loss of a relatively large amount of blood.
Classification
It should be noted that a brainstem stroke results in almost instantaneous death. Only in rare cases is it possible to save the patient’s life with such a diagnosis. At the same time, there is no likelihood of returning to a full life.
The brain stem is the center of all body systems and is directly connected to the spinal cord. It serves as a link between the commands of the brain centers and the nerves of the body: it is thanks to it that we are able to move, breathe, swallow, see, hear, and so on. The brain stem also regulates the circulatory system, thermoregulation, and heartbeat. That is why damage to it during a stroke most often leads to death.
Based on their origin, primary and secondary hemorrhagic stroke are distinguished:
| Primary | provoked by a hypertensive crisis or thinning of the walls of arteries and veins due to prolonged stress on them (for example, due to high blood pressure, physical and nervous overload, etc.) |
| Secondary | provoked by the rupture of an aneurysm, hemangioma and other vascular deformations and anomalies (malformations), congenital or formed in the process of life. |
Depending on the localization zone, I distinguish the following types of hemorrhagic stroke:
- Subarachnoid - hemorrhage into the space between the hard, soft and arachnoid membranes of the brain;
- Hemorrhage on the periphery of the brain or in the thickness of its tissue;
- Venticular hemorrhage - localized in the lateral ventricles;
- Combined type: occurs with extensive hemorrhage affecting several areas of the brain.
Peripheral hemorrhage is much less dangerous than intracerebral hemorrhage, which inevitably provokes the formation of hematomas, edema and subsequent death of brain tissue. Hematomas are also distinguished by location:
- Lobar - the hematoma is localized within one lobe of the brain, without going beyond the cerebral cortex.
- Medial - hemorrhage damages the thalamus.
- Lateral – damage to the subcortical nuclei localized in the white matter of the hemispheres (fence, amygdala, caudate, lenticular nuclei).
- Mixed - hematomas affecting several areas of the brain at once are most common.
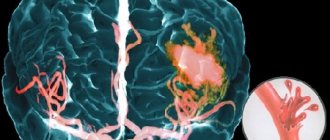
What happens during a stroke
Regardless of the cause of hemorrhagic stroke, the mechanism of damage to brain cells is the same. The pathological effect has several directions:
- Impaired tissue nutrition - due to the fact that the brain receives blood from several main vessels, this effect is partially compensated.
- Mechanical damage due to the fact that blood leaves the vessel under pressure and “pushes” the tissues apart.
In the case of parenchymal damage and hematoma formation, the second pathway is more pronounced, resulting in a disruption of communication between brain cells. Hemorrhagic permeation is a relatively uniform distribution of blood between the tissue structures of the brain, therefore the clinical course of such hemorrhage is more favorable.
In subarachnoid hemorrhage (SAH), there is a space where blood gets trapped. For this reason, mechanical damage is less than during the formation of a hematoma, but blood loss and malnutrition of brain tissue can be pronounced.
Cerebral hemorrhage (no matter how mild it may initially seem) is a condition that requires urgent diagnostic and therapeutic measures. Prescribing the correct treatment is possible only after neuroimaging, that is, magnetic resonance or computed tomography.
On our website you can get reliable information about the current discounts and promotions at various diagnostic centers for brain research this month. And also find out where it is possible to conduct an inspection at night, if necessary.
Surgical intervention
Any surgical intervention on the brain is a high risk and can often lead to serious complications, including the death of the patient. Therefore, surgical treatment is carried out in the presence of strict indications:
- Swelling or compression by hematoma of the medulla oblongata, which leads to the progression of neurological symptoms. In this case, to save the patient’s life, craniotomy is performed using a certain technique.
- Pathological changes in cerebral vessels (aneurysms, malformations), accompanied by bleeding. For treatment, special clips are used, which are surgically applied to the neck of the aneurysm.
- For ischemic stroke, when conservative therapy is ineffective, carotid endarterectomy followed by stenting can be performed. The operation is performed endovascularly (without incisions).
In the postoperative period, the patient's condition remains unstable for a long time. It can often be complicated by swelling of the brain tissue, which lasts up to two weeks. In the future, therapeutic measures are carried out aimed at restoring lost functions and preventing a recurrent stroke.
Manifestations of hemorrhagic stroke
Symptoms and signs of hemorrhagic stroke are very diverse, they depend on:
- process localization;
- prevalence of the lesion;
- volume and duration of blood loss;
- the degree of swelling of brain tissue and increased intracranial pressure.
The shorter the period from the onset of the disease to the provision of qualified care to the patient, the fewer complications and the better the prognosis. In order not to waste time, you need to know the general signs of a stroke:
- sudden weakness in the arm/leg;
- numbness of half the face, arms/legs on one side;
- new facial asymmetry;
- speech disorder;
- a sharp decrease in vision in one eye or blindness;
- causeless loss of consciousness, especially in combination with previous symptoms.
If any of the symptoms occur against the background of complete well-being, it is necessary to carry out an accurate diagnosis as soon as possible in a specialized medical institution.
All available information about the nearest medical centers where urgent computer or magnetic resonance imaging of the brain can be performed can be obtained by calling 8 (812) 317-00-37.
Different types of hemorrhagic stroke may occur in different ways, but they also have common features. The disease is often characterized by:
- abrupt onset;
- rapid deterioration of the condition;
- loss of consciousness;
- development in the afternoon, at the peak of physical or emotional stress.
Taking into account the peculiarities of the course of the disease, the most important factor for a successful outcome is time. This means that you should not wait for the condition to improve; you should urgently seek qualified medical help.
It is possible to carry out a timely and accurate diagnosis of this disease by dialing a phone number. Our employees will help you quickly select a medical center that meets your needs: the nearest location, the qualifications of specialists, the quality of diagnostic equipment, the cost of the study and the availability of current promotions.
General cerebral symptoms
General cerebral symptoms include:
- Headache of great intensity, which occurs suddenly and is accompanied by dizziness. Some patients describe it as “a blow to the head.” It does not stop on its own and is not relieved by painkillers. Often SAH is accompanied only by this symptom.
- Vomiting without previous nausea, caused by cerebral edema and increased intracranial pressure.
- Loss of consciousness followed by the development of a coma. This symptom may be the only manifestation of a hemorrhagic stroke. It is important that there is a person with the patient who saw what happened.
- Stunnedness, causeless drowsiness. However, often at the initial stage of development of hemorrhagic stroke there is increased emotional and motor excitability, which is then replaced by inhibition.
- Signs of dysfunction of the autonomic nervous system: cold sweat, feeling hot, dry mouth.
- An increase in body temperature to high values can be observed in severe cases.
Focal symptoms
Focal manifestations are a group of symptoms characterized by a number of specific neurological signs that occur depending on the location of the lesion.
The most common focal manifestations are:
- weakness in the arm/leg/half of the body, up to paralysis;
- violation of the movement of facial muscles, due to which the eyelid does not rise, the corner of the mouth drops and the cheek “sails” when exhaling;
- impaired skin sensitivity;
- pathology of speech, vision, hearing;
- exotropia;
- swallowing disorder;
- spatial disorientation of varying severity - staggering, tilting and turning to the side when walking, inability to assume a vertical body position.
Sometimes, based on characteristic focal manifestations, the localization of the pathology can be assumed:
- When the lesion is located in the frontal lobe, characteristic symptoms may be a forced rotation of the patient’s head and eyes in the direction of the hemorrhage. The so-called “frontal psyche” often develops, which manifests itself in an inadequate assessment of the state of health and a decrease in criticism of one’s actions.
- The localization of the hematoma in the temporal lobe may be indicated by early epileptic seizures.
- Hematomas of the parieto-occipital localization can sometimes have scant symptoms and are detected by chance during CT or MRI of the brain, which indicates the importance of neuroimaging methods.
- Hemorrhagic stroke in the brainstem often manifests as breathing and heartbeat disturbances.
- Damage to the cerebellum is characterized by loss of consciousness, vomiting, severe dizziness and loss of coordination.
It should be noted that these clinical manifestations can be seen with small hematomas. With its significant size, cerebral edema rapidly increases and the patient’s condition becomes so severe that it becomes impossible to determine focal symptoms.
Providing emergency first aid
A stroke occurs suddenly and requires immediate outside help.
The first step is to call a team of medical workers, and while it is on its way, take care of the victim, providing him with support. The process is often accompanied by vomiting, and the accumulated masses interfere with breathing. If problems with perspiration are detected, it is necessary to clear the pathways through which oxygen enters the lungs. To do this, the person should be laid on his side and with a finger wrapped in gauze or a piece of clothing, clean the oral cavity. If you have instruments with you that can measure pressure or blood sugar levels, it is recommended to record the values of these parameters and report them to the arriving doctors.
An important indicator is the moment of onset of symptoms. It would not be amiss to note the time of its occurrence. The use of drugs aimed at lowering blood pressure is contraindicated. Increased pressure after a circulatory disturbance in the brain stem is a normal reaction of the body necessary to adapt to an emergency situation. Eating food or water is also contraindicated; there is a possibility of a negative effect that will aggravate the matter. If a person loses consciousness, it is allowed to be moved, despite existing myths that state the opposite.
The place should be arranged in such a way that the upper body and head are raised, and clothes are unbuttoned to facilitate the flow of oxygen into the lungs. If the incident occurred in a confined space, it is advisable to open the windows and provide fresh air and peace.
If the victim experiences convulsive muscle contractions and foamy discharge from the mouth, it is necessary to place a pillow or rolled up clothing under the head, and also monitor the position of the arms and legs so that the patient does not injure himself and others. Holding the limbs while contracting is strictly prohibited; this will lead to worsening of the situation. The person providing assistance must be prepared for repeated attacks and remove foam from the mouth in a timely manner.
You cannot take measures to restore consciousness, much less use ammonia for this. Its effects can cause lung failure and ultimately death. During the period of pre-medical measures, it is necessary to monitor the heartbeat and pulse. If cardiac arrest is determined, immediate resuscitation is required through chest compressions and mouth-to-mouth or mouth-to-nose artificial respiration.
Meningeal symptoms
Signs of irritation of the meninges can occur with parenchymal hemorrhage due to cerebral edema, but they are more characteristic of subarachnoid hemorrhage.
The most typical sign is a stiff neck, when the patient is unable to press the chin to the chest when lying down.
If the patient bends his knees while checking for rigidity, this is another sign of irritation of the meninges, which is called Brudzinski's sign.
Complications of hemorrhagic stroke
The most common complication of non-traumatic hemorrhage is epileptic seizures. They are divided into early, which arose in the first week after a stroke, and late, which developed 7 days after a cerebrovascular accident.
To a serious life-threatening illness, the human body responds with a systemic inflammatory response - an increase in body temperature, changes in blood tests. Such a complication may indicate a deterioration in the patient’s condition. Then the doctor assumes an increase in the source of hemorrhage or the addition of an infection.
The consequence of maintaining a recumbent position may be the development of deep vein thrombosis of the legs, which will entail the development of other, no less dangerous, diseases.
Complications also include cardiac decompensation, which can manifest itself in the development of various arrhythmias, cardiomyopathies, and congestive pneumonia.
Due to damage to brain tissue, memory and mental performance may be impaired.
Diagnosis of hemorrhagic stroke
In order for a person without medical education to be able to promptly suspect the initial signs of a stroke in a relative or friend, special recommendations have been developed.
The “Face-Hand-Speech” test involves detecting the most typical signs of pathology:
- Detection of facial asymmetry.
- The patient needs to extend both arms in front of him. If one of them involuntarily descends, then there is a possibility of a vascular accident.
- The patient is asked to give his full name, address, time of year to determine speech impairment and the person’s orientation in space and time.
There are simplified versions of the tests, for example, UZP - smile, speak and raise your hands. If there are noticeable deviations in these actions, emergency measures should be taken to transport the patient to the hospital, that is, call an ambulance.
Before providing effective treatment, the doctor must answer two questions:
- Is there a stroke?
- If yes, what type of stroke developed?
Determining the nature of brain damage is only possible using CT or MRI - without these highly accurate research methods, the diagnosis of stroke is incomplete.
There are signs that are more likely to indicate the occurrence of a hemorrhagic stroke:
- The patient was previously diagnosed with arterial hypertension. In this case, the medications did not have the desired effect or the person did not take them.
- Deterioration of the condition is associated with a peak in physical activity or emotional stress.
- A sharp and significant deterioration in health with pronounced cerebral and focal symptoms.
For subarachnoid hemorrhage, slightly different signs have been identified, including:
- Young age of patients.
- Often the primary symptom is a severe headache.
- Insignificant severity of focal symptoms.
Often an important distinguishing feature of hemorrhagic stroke from ischemic stroke is the increase in impairment of consciousness with unchanged motor and sensory pathology. This may be a sign of an enlarged hematoma.
Differential diagnosis is vital because treatment for different types of stroke can vary dramatically.
Left-hand side
If the left side is affected, the consequences are characterized by disruption of the right side of the body. The patient experiences complete or partial paralysis, and not only the leg and arm are affected, but also half of the tongue and larynx. Such patients develop gait disturbances and a characteristic posture of the right hand (folded in a boat).
The victim experiences deterioration in memory and speech, and the ability to clearly express thoughts is impaired. Damage to the left hemisphere of the brain is characterized by problems with recognizing time sequences; it cannot decompose complex elements into components. Impairments in written and oral speech appear.
Instrumental diagnostics
Computed tomography is the gold standard for detecting cerebral hemorrhage. This study is distinguished by its accessibility, information content and short scanning time.
A CT scan performed in the first hours of the disease will help the doctor establish an accurate diagnosis and prescribe the correct treatment.
If the cause of the vessel damage is a malformation, then to identify it using CT, it is necessary to administer a contrast agent. Magnetic resonance scanning without any problems will allow you to localize pathologically altered vessels without paramagnetic enhancement.
MRI is more sensitive to small foci of hemorrhage and helps to more accurately determine the stage of the process. However, in order to clarify the hemorrhagic nature of the stroke, an MRI scan should be done 24 hours after the onset of the disease. Even many years after a vascular accident, an MRI of the brain will reveal pathology.
Since MRI shows the structures of the brain in more detail, this type of tomography is preferable to determine the root cause of a hemorrhagic stroke.
Each method has its own advantages and disadvantages, so before using them, it is recommended to examine a specialist - a neurologist.
Since the patient’s further well-being depends on the time of initiation of treatment, the primary diagnosis is carried out using computed tomography. Later, after starting the necessary therapy or surgical treatment, an MRI will help clarify the cause of the stroke.
Treatment of hemorrhagic stroke
After identifying signs of a stroke, relatives or friends need to provide emergency assistance to the victim, which consists of:
- positioning the person on the right side (especially when vomiting) to prevent stomach contents from entering the respiratory tract;
- raising the upper half of the body by approximately 30 degrees;
- measuring blood pressure and helping to take medication for high blood pressure (in this case, you should not give medications that need to be washed down with water, because a stroke may be accompanied by a swallowing disorder);
- organizing optimal air access, that is, loosening the collar, tie, belt and freeing from restrictive clothing.
Upon arrival of the ambulance team, any information about the disease will help in correct diagnosis. To do this, you need to tell doctors about:
- time of onset of the disease;
- the nature of the development of the pathology: the condition worsened sharply or gradually;
- the symptoms with which the disease began;
- signs of a stroke that occurred later;
- chronic diseases (especially those that could be the cause of the development of a vascular accident);
- constant use of medications;
- blood pressure numbers (if it was measured).
The medical professional should tell everything that happened to the victim.
General principles of treatment
After admission to the hospital, the neurologist assesses the severity of the condition, and then determines whether the patient needs to be operated on or whether it is better to treat him conservatively.
Many doctors agree that the most dangerous are the 3rd day after a vascular accident, and stabilization of the condition occurs on days 5-7-14, depending on the severity of the pathology.
Regardless of the type of stroke, treatment begins with:
- Bed rest.
- Elimination of any physical stress. For this purpose, laxatives and other symptomatic drugs may be prescribed, for example, antitussives for severe dry cough.
- Organization of patient care for the prevention of infectious complications and bedsores.
- Adequate nutrition depending on the level of consciousness: if the patient can swallow on his own, he eats gentle food through the mouth, if he cannot, through a tube.
- Prescription of drugs that regulate blood clotting. This is necessary to stop bleeding or prevent its recurrence.
- The use of neuroprotectors - medications that reduce the “suffering” of brain cells from oxygen starvation.
Medicines are prescribed only when they are necessary and not contraindicated.
Types of paralysis on the right side
According to the nature and localization of vascular accidents, the types and subtypes of paralysis are classified:
- Central paralysis. It develops when the areas of the brain and spinal cord responsible for the function of movement and the state of the neuromuscular complex are damaged. Characterized by specific spastic reactions. With the central form of paralysis, all muscles are affected, which are in constant tension, and when calm they show clonus - rhythmic twitching, mainly in the area of the knees and feet. In many areas, diagnostic reflexes are absent or weakened.
- Peripheral paralysis. With this type of stroke, a decrease or absence of neurological reflexes develops. The tone in the muscles is not determined, they atrophy, decrease in mass, patients lose the ability to move, self-care and generally do any activity. The main task is to restore the conduction pathways of impulses from the brain and spinal cord to the neuromuscular system. By the nature of the pathological symptoms and the areas of their location, it is possible to determine which segments of the central nervous system are out of order.
Management of patients with subarachnoid hemorrhage
If the diagnosis of subarachnoid hemorrhage is confirmed, the patient must remain in the hospital for at least a month. Treatment consists of:
- Monitor blood pressure and lower it with medications if necessary.
- Prescriptions of drugs that relieve headaches and agitation.
- Normalization of breathing and metabolic disorders.
- Reduce intracranial pressure by administering osmotic diuretics and elevating the head of the bed for several weeks.
- Carrying out therapeutic measures to prevent complications in the form of spasm of cerebral vessels, that is, the prevention of ischemic disorders.
The danger of SAH lies in the fact that many patients consult a doctor only some time after the onset of the pathology. Therefore, treatment may be less effective.
Management of patients with intracerebral hemorrhage
Hemorrhagic stroke is a condition that requires emergency diagnosis, adequate treatment and observation.
To do this you need:
- Conduct constant monitoring of the patient’s condition, especially in the first days after the onset of the disease: monitoring breathing and indicators of the state of the cardiovascular system.
- Monitor blood pressure numbers. They are often not reduced to normal levels, so as not to impair blood supply to the brain and provoke vasospasm.
- Prescription of hypoglycemic drugs - in almost half of patients, blood glucose levels increase.
- Use of antipyretic drugs. An increase in body temperature entails worsening cerebral edema, increased intracranial pressure and can lead to a significant deterioration in the patient’s general condition.
- Carrying out symptomatic therapy and treatment of complications.
Drug therapy
Drug treatment is an integral part of patient resuscitation, prevention and recovery.
The therapy provided should be comprehensive and aimed at preserving the vital functions of the body. The main directions for this: Correction of disorders of the respiratory system. If necessary, connection to a ventilator. In the acute period, infusion therapy with plasma preparations and rheopolyglucin is carried out. Normalization of blood pressure indicators. At high blood pressure levels, antihypertensive drugs are prescribed, making sure that changes to normal values occur smoothly and gradually. The main drugs used are from the group of ganglion blockers and ACE inhibitors. In case of severe hypotension, glucocorticosteroids and dopaminomimetics are administered. Reducing body temperature is carried out using non-steroidal anti-inflammatory drugs.
Reducing intracranial pressure and cerebral edema - with the help of diuretics. In some cases, a hypertonic saline solution is administered.
Restoring blood supply to the affected areas and preventing thrombosis. Here they use drugs from the group of antiplatelet agents and anticoagulants.
Improving the nutrition of brain tissue and intracellular metabolism is carried out with the help of nootropics, antioxidants, and cytoprotectors.
The treatment of hemorrhagic and ischemic stroke has its own characteristics. In case of hemorrhage, the use of anticoagulants and antiplatelet agents is contraindicated. The main treatment is aimed at stopping the bleeding and removing the hematoma. Treatment with medications is carried out in the intensive care unit. The following substances are prescribed:
- diuretics aimed at preventing edema;
- sedatives;
- oxygen therapy - if the patient is able to breathe on his own, catheters are installed, otherwise a special support device is connected;
- muscle relaxants to prevent seizures;
- blood thinners that increase blood flow;
- antihypertensive drugs to prevent recurrent vascular ruptures.
At first, all drug therapy is aimed at eliminating repeated attacks and severe consequences.
Doctors keep an eye on the patient until the body’s functioning is completely normalized, and when the patient’s well-being improves, they are transferred to a ward for further recovery. Make an appointment
Rehabilitation after hemorrhagic stroke
Recovery of post-stroke patients is an important stage in improving a person’s quality of life. Carrying out these activities helps eliminate existing movement and sensitivity disorders.
Medical rehabilitation should be:
- individual - developed for a specific patient;
- timely - start as early as possible;
- adequate - depend on the patient’s condition and his capabilities;
- staged - gradual, slow complication of exercises and an increase in the variety of rehabilitation methods;
- long-term;
- comprehensive - for greater efficiency, the maximum possible rehabilitation methods are used to influence the human body from different angles;
- successive - when a patient moves from one medical institution to another, recovery measures must continue each other.
The main criterion for starting rehabilitation measures for hemorrhagic stroke is not only normal hemodynamics (blood pressure, heart rate), but also the reverse development of changes in the brain (for example, signs of a decrease in cerebral edema).
The most important factor influencing the quality of recovery is the active participation of the patient in the rehabilitation process.
The transition to more complex exercises is made only if the condition of the patient’s cardiovascular and respiratory systems is monitored.
How long does it take for speech to be restored?
Rehabilitation of speech functions usually begins a week after the rupture of a blood vessel in the brain, provided that the patient’s condition is stable. However, there are situations when the patient is not able to start exercising even after a month. One way or another, rehabilitation therapy should begin no later than two months later. Otherwise, it will be much more difficult to regain lost abilities.
It is very difficult to give an accurate forecast regarding the time of speech recovery after a stroke. Rehabilitation is a step-by-step process with a clear sequence. The duration of each stage varies and is individual for each patient. On average, the maximum improvement in speech abilities is observed in the first six months after the illness. The entire recovery period lasts from three to five years.
Rehabilitation in the intensive care unit
12-24 hours after a vascular accident, it is already possible to carry out restoration measures. Before they begin, a test is performed to assess independent swallowing, after which the patient’s feeding method is selected.
The following rehabilitation methods are used during the acute period of a stroke:
- Treatment by position. The position of the patient's head/arms/legs should be changed approximately every two to three hours, as well as turned to the side (if the condition allows it). In order to hold a person in a certain position, bolsters or pillows are used.
- Verticalization - giving the patient an upright position. This can happen passively (with the help of a functional bed or table), passive-active and active. However, to carry out this rehabilitation method, it is necessary to ensure the stability of the circulatory system. More often, verticalization begins in the neurological department.
- Breathing exercises can be carried out in various ways depending on the patient’s condition: vibration with the hands while exhaling, in a position that facilitates breathing, contact breathing (stimulation by touching the hands to the chest) and others.
- Therapeutic gymnastics includes assistance in restoring not only the large muscles of the limbs, but also the muscles of the neck and eyes. At the initial stage, passive gymnastics is performed, when flexion/extension of the patient’s fingers, arms and legs is performed by a qualified physical therapy nurse.
Also during this period, physiotherapeutic treatment is actively used: magnetic therapy, magnetic laser therapy, reflexology, electrical stimulation, darsonvalization and other methods.
Recovery in a rehabilitation center
The most effective assistance in rehabilitation is provided in specialized medical centers. It includes the following methods:
- kinesitherapy – training in walking and everyday skills;
- electrical stimulation of peripheral nerves and muscles;
- physiotherapy and massage;
- classes with a speech therapist-aphasiologist to restore speech;
- use of neurotrophic medications (Cerebrolysin, Piracetam, Semax);
- psychotherapy;
- biofeedback sessions;
- acupuncture;
- occupational therapy.
- Stroke on the left side: consequences and features of recovery. How long do people live with this diagnosis?
If the patient ends up at home, the possibilities for rehabilitation are reduced.
Rehabilitation in the acute period
At this stage (from 24 hours to 3 weeks), maintaining the achieved effect and improving exercise tolerance plays a significant role. For this purpose, methods such as:
- treatment by position;
- massage, which is equivalent to passive gymnastics;
- breathing exercises;
- active verticalization in the absence of contraindications (if necessary, using additional support);
- mechanotherapy;
- training on cyclic simulators.
During this recovery period, active correction of speech disorders is carried out with the involvement of speech therapists.
Lifestyle
Stroke is a disease in which a person must start life in new conditions. Most people find it difficult to accept their condition, so deep depression is as dangerous a complication as the physical manifestations. Already in the first stages of recovery, much attention is paid to this aspect.
The scientific, material and technical base of the Yusupov Hospital allows patients to undergo rehabilitation procedures using modern equipment that meets European standards.
Rehabilitation in the early recovery period
This stage begins 21 days from the onset of the disease and lasts up to six months.
Early recovery can take place in rehabilitation centers, clinics or at home. Self-execution of exercises is possible only if they are performed correctly and there is no need for constant monitoring of the patient. Therefore, all exercises at home are selected strictly individually.
The period of early rehabilitation should be a continuation of the inpatient recovery phase. Nowadays, more attention is paid to everyday skills: renewing them or teaching possible alternatives. Equally important is assistance in a person’s social adaptation.
Rehabilitation objectives
The main objectives of the ongoing rehabilitation are:
- Work on restoring lost everyday and physiological functions of a person suffering from a stroke. Restoring full range of motion, the ability to independently care for oneself and perform simple household chores.
- Restoration of lost professional ability to work with a return to the previous place of activity or assistance in retraining.
- Maintaining the necessary social activity of a person, first of all, restoring his contact with loved ones and the ability to make new acquaintances;
It is very important to prevent a possible relapse and correct the patient’s current lifestyle.
Rehabilitation in the late recovery period
This stage lasts from six months to a year after the stroke, and sometimes longer (with persistent changes). Rehabilitation in the late recovery period involves preparing the patient for the maximum independence that he can achieve.
In addition to physical rehabilitation, work continues on social adaptation and restoration of professional skills or reorientation.
Most experts point to the positive effects of occupational therapy, especially work related to the earth.
During this period, a person may need psychological support, so psychotherapeutic consultations are carried out.
Fighting bedsores
Bedsores are a dangerous enemy of bedridden patients who have to remain in bed for long periods of time. Bedsores appear in areas that are subject to the greatest pressure - the tailbone, shoulder blades, buttocks, legs, forearms.
Bedsores in advanced stages require surgical treatment. There are cases when a patient was saved in intensive care, but then, due to poor care, he died from sepsis that developed from banal bedsores. Nursing after a stroke is exactly the case when an experienced and conscientious nurse is just as important as a doctor. And sometimes it’s even more important.